If you want to talk about estrogen, it’s impossible to avoid the topic of reproduction. The sex hormone makes puberty, periods, and pregnancy possible.
But new research is redefining this hormone, uncovering its powerful influence throughout the body — on the skin, kidneys, bones, and more. UC San Francisco scientists are contributing to this shift in our understanding, revealing estrogen’s potential to shape our health in myriad ways, from chronic pain to brain degeneration.
Fueling the Motivation to Move
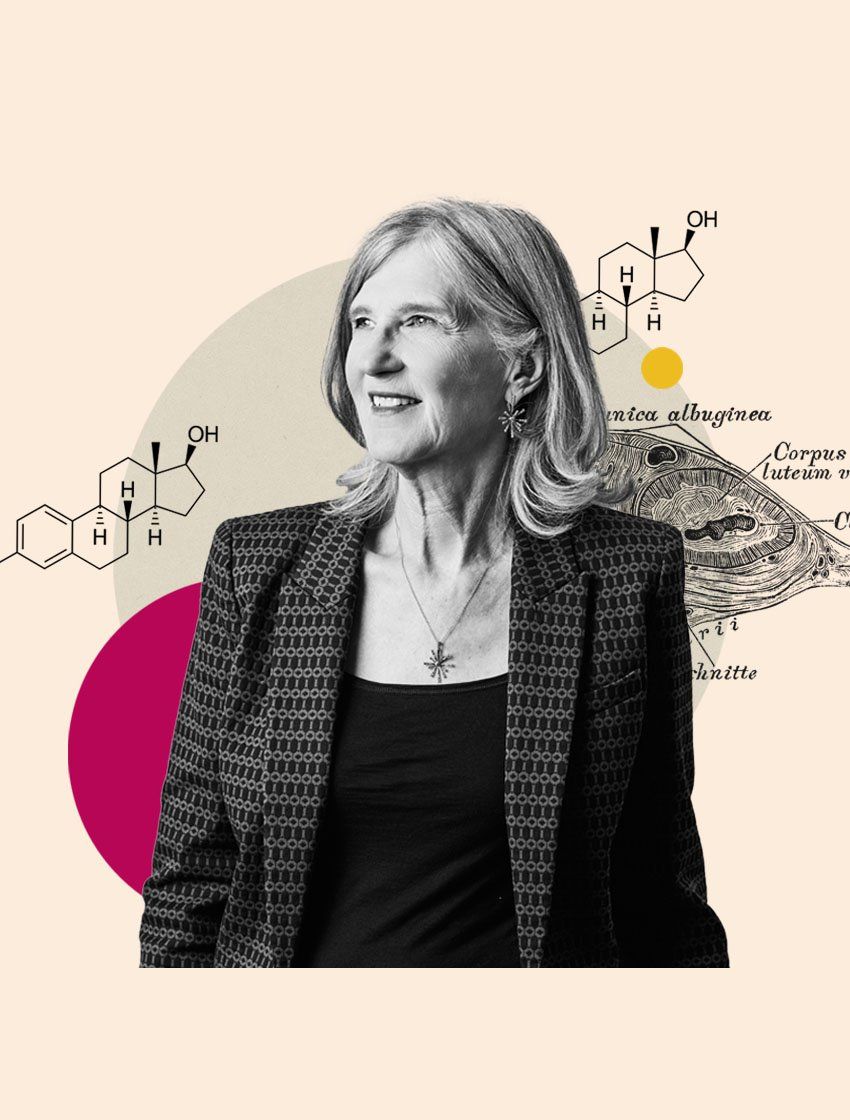
Few people have dug deeper into sex hormones than Holly Ingraham, PhD. She’s spent many years teasing out the mechanisms behind sex differences.
For example, right before females ovulate — when estrogen reaches its peak — they tend to be more physically active. The behavior has been noted in all kinds of animals, from humans to hamsters to horses. The evolutionary theory behind this restless energy? When you’re more driven to explore, you’re more likely to find a mate.
Ingraham, UCSF’s Herzstein Professor of Molecular Physiology, wanted to figure out exactly how estrogen spurs this kind of activity. Her team used CRISPR technology to study mice and map how proteins attach to DNA in their brains. They discovered a group of brain cells in the hypothalamus that get stirred up by estrogen. When the sex hormone binds to estrogen receptors in these neurons, it also switches on the MC4R gene, which nudges the female mice to move more.
“It’s this really old, primitive part of the brain that controls many things: sleep, temperature regulation, food intake, sexual behavior, water retention,” Ingraham says. “This region is exquisitely sensitive to estrogen, and these particular neurons drive locomotion. It’s wild: When you activate them, you see this huge spike in physical activity.”
Observations in mice don’t always translate to humans, but Ingraham hopes her team’s findings might lead to solutions for aging women struggling with a diminished desire to move. This shift tends to happen around menopause, when the ovaries dramatically reduce their production of estrogen and progesterone. Extra weight often settles in, too. And a sedentary life, beyond being arguably less fun, comes with increased odds of heart attacks, diabetes, back pain … the list goes on.
Notably, the MC4R receptor is also a target of Vyleesi, an injectable medication approved in 2019 to spark arousal and desire in premenopausal women who have inexplicably lost their libido. Unfortunately, exactly how Vyleesi does this is still unclear — and the medication hasn’t been studied in older women.
Of course, many women use hormone therapy to cope with symptoms of declining estrogen. But Ingraham says we need much more research into estrogen’s effects, along with new alternatives — especially for women with conditions that dramatically heighten the risks of hormone therapy, like breast cancer.
“The big question,” she says, “is whether we can deliver estrogen just to the brain and get its benefits there, without affecting the rest of the body.”
Amplifying Gut Reactions
That brings us to a part of the body that can overreact to estrogen: the gut.
Women are about 80% more likely than men to be diagnosed with irritable bowel syndrome (IBS), a digestive disorder that can include cramping, bloating, diarrhea, and constipation. Again, there are theories about why female colons might function in ways that helped our ancestors reproduce, even if they prove frustrating for modern life. Increased gut sensitivity in a pregnant woman might, say, protect a developing fetus from harmful substances.
“The thinking is that you wouldn’t make the same mistake twice,” Ingraham says. “If you’re getting massive gut pain, you’re going to avoid that food or that toxin.”
But tracking every ingredient one consumes is almost impossible with today’s typical grocery haul — let alone at a restaurant. And we’re still learning how women develop this gut sensitivity. Ingraham’s lab recently showed, in a mouse model of IBS, that estrogen triggers a chain reaction in the gut. Certain gut cells detect byproducts from gut bacteria. Estrogen makes those cells extra sensitive, prompting them to release a chemical signal. The signal then activates cells that squirt out serotonin, which makes the gut’s nerves more excitable. Voilà! Gut sensitivity.
“Estrogen is basically turning up the sensor for acetate,” Ingraham explains. “It’s a compound gut bacteria produce when they break down certain carbs. GI doctors often tell IBS patients to reduce those carbs with a low FODMAP diet, but it’s very hard to follow.”
FODMAP stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols — short-chain carbohydrates that can be tough to digest. Eliminating them entirely is difficult because they’re found in nutritious foods like onions, beans, apples, and yogurt. IBS patients sometimes avoid these carbs for a few weeks, then reintroduce them, one at a time, to see what they can tolerate.
We now live about three decades beyond menopause. We need to truly understand how the hormones affect us. Maybe none of this mattered back when most people died by age 40 or 45. But it matters now.
Holly Ingraham, PhD
Ingraham thinks it might be possible to treat IBS in a new way one day — not by reducing estrogen or experimenting with tedious diets, but by calming down certain receptors in the colon. In the meantime, her lab continues to investigate exactly how estrogen influences our bodies, for better and for worse.
“We have huge fluctuations in our hormones, unlike men,” Ingraham says. “And we now live about three decades beyond menopause. We need to truly understand how the hormones affect us. Maybe none of this mattered back when most people died by age 40 or 45. But it matters now.”
Tapping the Body’s Own Painkillers
Sex differences in pain conditions have also sparked researchers’ curiosity about estrogen. Unfortunately, for many women, pain is an ordinary — albeit miserable — experience. It can ebb and flow with the menstrual cycle, ease with pregnancy, surge with childbirth. In addition, women suffer more from chronic pain conditions. They’re three times as likely as men to develop migraines, and about four in five patients with fibromyalgia are women.
For Élora Midavaine, PhD, a UCSF postdoctoral scholar, the importance of sex differences in pain became undeniable during an experiment. She was testing a new analgesic drug meant to treat bone pain, and it wasn’t working.
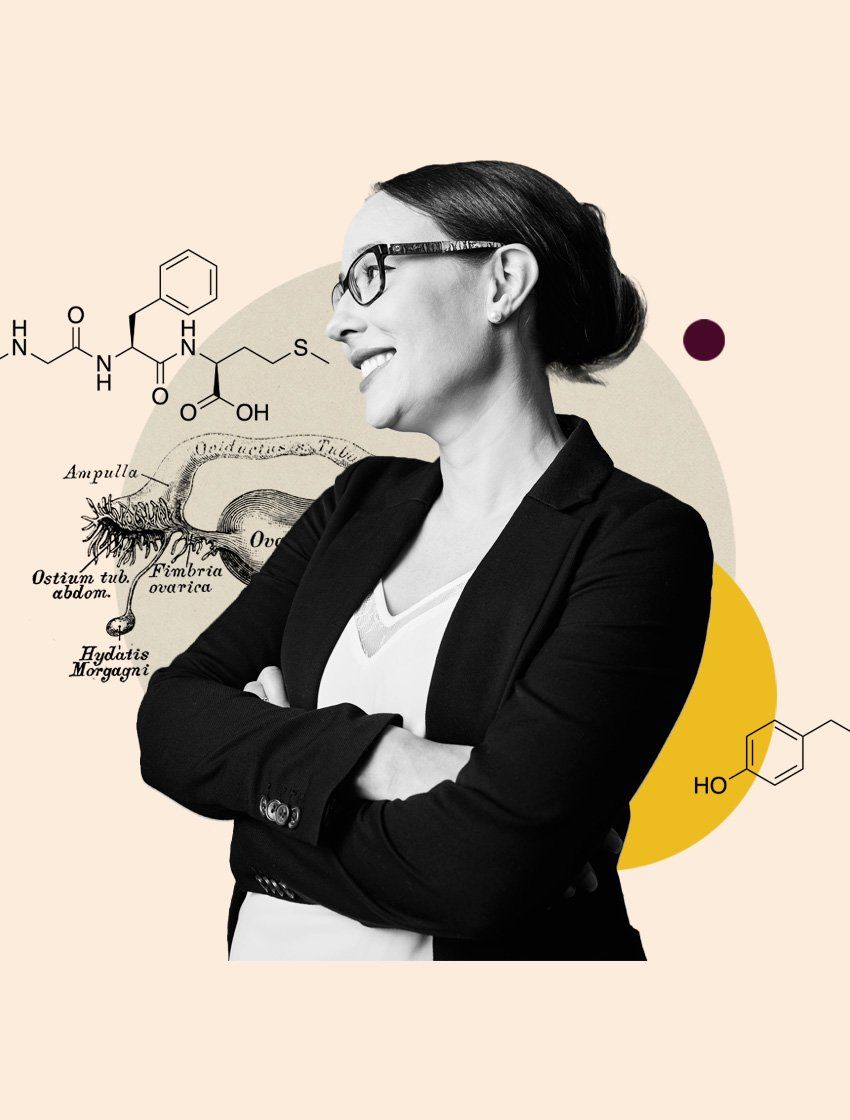
“I tried for a year, maybe two years,” Midavaine says. “It felt like forever. One day, I had a gut feeling that I should test that drug in male mice because I had only been working with females. Suddenly, it had a beautiful analgesic effect.”
It’s notable that Midavaine was working with female mice in the first place. For many years, biomedical researchers often ignored sex differences, favoring male animals in experiments because cycling sex hormones might complicate their results. This practice created gaps in knowledge, which led to drug doses that harmed women because their sex-specific effects weren’t known. In 2016, the National Institutes of Health finally issued a policy requiring researchers to consider sex in NIH-funded experiments.
By 2022, when Midavaine joined the lab of Allan Basbaum, PhD, chair of the UCSF Department of Anatomy, she knew she wanted to investigate sex differences — and she was curious about the role of immune cells in mediating pain. A few years later, she was the lead author of a study that revealed a surprising way sex hormones can suppress pain.
Midavaine and her colleagues found that female sex hormones can tell the immune system to produce its own natural opioids — similar to the pain-relieving compounds in prescription drugs but made by the body itself. Estrogen and progesterone act on special immune cells in the meninges, the protective layers surrounding the brain and spinal cord. These cells, called T regs, then release enkephalins, natural pain blockers that calm nerve signals.
But this was true only for female mice, not males. Again, evolutionary theories might explain the finding. Perhaps extra pain relief has helped females of many species continue to secure food and protect themselves from harm during the discomfort of pregnancy.
Midavaine’s work might also help explain why some women experience more pain after menopause, when both estrogen and progesterone levels drop. She hopes her team’s findings will open the door to treatments that harness the body’s own painkillers, potentially offering relief without a high risk of addiction. Because pain is so personal — shaped not just by nerves or the brain, but by how we feel — it’s been difficult for researchers to study, let alone develop new drugs that reduce it without dangerous side effects.
“Pain is a very complex experience,” Midavaine says. “Emotions modulate pain. Sex hormones modulate pain. Expectations or even human contact can interact with pain.”
In the meantime, there are many ways to tap the body’s ability to produce its own opioids. That’s why psychological interventions and alternative therapies like massage can often ease pain, even without medication.
Protecting the Brain
Another factor fueling researchers’ interest in estrogen: its possible role in autoimmune disorders. We still don’t understand why these diseases mostly strike women — or whether deciphering the underlying sex differences will lead to more tailored treatment strategies.
Take multiple sclerosis, or MS. The severity of this disease varies greatly — from fatigue and weakness to loss of mobility — but the damage comes from the immune system attacking the myelin that protects nerves. Women are three times more likely to develop MS than men, and scientists have long suspected that hormones play a role. Hormonal shifts like puberty often trigger autoimmune diseases. And MS symptoms often ease when a form of estrogen unique to pregnancy, estriol, surges. After pregnancy, however, estriol levels become nearly undetectable again.

“During pregnancy, the risk of MS-related immune activity quiets down,” says Riley Bove, MD, UCSF’s Rosenberg Ach Family Professor of Neuroimmunology. “But once the baby’s delivered, you see an increase in immune activity and new brain injury. About 50% of women who are untreated have new brain lesions postpartum.”
UCLA scientists found that estriol can actually repair myelin damage in mice, and they’re still studying whether estriol might benefit people with MS. Bove wanted to understand how the hormonal dip of menopause might shape the course of the disease as well.
After more than a decade of tracking nearly 200 women with MS, Bove and her colleagues found that their mobility declined faster after menopause, even after accounting for age, weight, and tobacco use. The women took longer to complete a short walking test, and their fine motor skills and cognitive performance also dipped.
Bove’s team also measured a blood biomarker called neurofilament light chain, which indicates increased degeneration of nerve cells — a hallmark of advancing MS. Those levels ticked up after menopause, too.
“We wanted to know: If you lose these reproductive hormones, do you see increasing neurodegeneration?” Bove muses. “And we saw an inflection point after menopause. It’s a signal that maybe reproductive hormones are relevant to brain health and repair.”
Because only 17% of the study participants used estrogen therapy, Bove’s team couldn’t determine whether it slowed the MS decline associated with menopause. In mice, estrogen shows protective effects in the brain — but Bove says it’s been much harder to demonstrate in humans. She believes more research into hormone therapy is needed for women with elevated odds of developing neurological damage, whether due to MS or a genetic factor.
“In that high-risk group, would some form of hormone therapy potentially protect the brain?” Bove asks. “When we think about precision medicine, we have to think about which patients might benefit the most from an intervention and design studies accordingly. It’s not a one-size-fits-all model.”
While Bove doesn’t have a study like this planned yet, she’s been thrilled to see more research funding devoted to women’s health in recent years — especially for conditions that emerge in middle age.
“For a long time, we didn’t have funding agencies investing in this kind of work,” Bove says. “It’s one thing when you’re talking about studying women’s bodies in relation to childbearing, which society values. But after menopause? There’s been this lack of ability to hear women and their concerns.
“But I see that changing. We all want brain health at age 80. I’m curious about what we need to do earlier, at age 50, 60, 70, to get there.”
The science of estrogen — and how these emerging insights might help patients — is still unfolding. While researchers may not align on the implications of every study, many agree on this: The latest wave of research unpacking the effects of sex hormones is long overdue.
“Historically, we have basically defined women’s health as nothing more than reproduction and breast cancer,” Ingraham says. “That always struck me as completely narrow-minded — and it could explain why breakthroughs in women’s health have been so slow to emerge. We have a lot of work to do.”