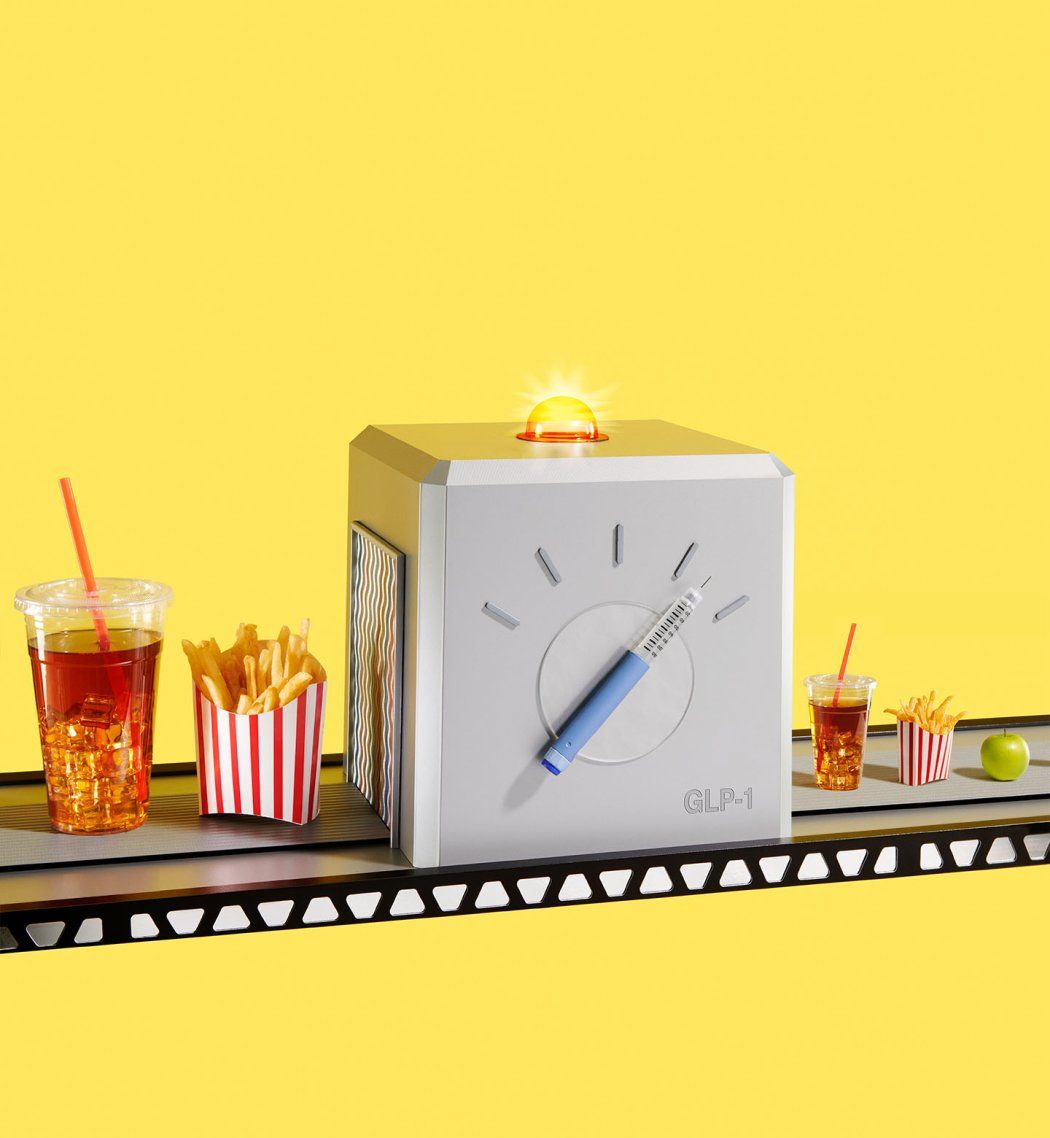
Whether you view the latest weight loss drugs as a miracle or a menace, the hype around them is impossible to ignore. Ozempic seized the spotlight first; a weekly injection intended to treat diabetes, it was quickly repurposed by people trying to trim down. Then came Wegovy, a high-dose version officially marketed as an obesity treatment. The drugs have proven so popular that the market value of the Danish company behind them recently exceeded the entire economy of Denmark. In November, Eli Lilly’s Zepbound joined their ranks.
The medications have inspired a lot of hope but also intense debate. Do they deepen our bias against fat and make life more miserable – draining patients not just of money but also dignity and joy? Or are they the cure that people with obesity – roughly 40% of American adults – have been waiting for? Before you make up your mind, consider what UCSF experts have to say about the new wave of weight loss drugs.
1
So far, they seem much better than the get-thin-fast drugs of yore.
The history of weight loss medication is littered with drugs that seemed like impressive, easy solutions – at first. Chemist Derek Lowe, PhD, summarized the decades-long quest to find a cure for obesity as, “for the most part, a bottomless pit into which people shove money and time.” The demand for this kind of drug is overwhelming, according to Suneil Koliwad, MD, PhD, UCSF’s chief of endocrinology and metabolism and an expert in diabetes and obesity.
“This can lead to less scrutiny and caution after a weight loss drug gets initial approval from the U.S. Food and Drug Administration,” Koliwad says. “There used to be fen-phen billboards, remember? Then five to 10 years later, we started seeing vascular and cardiac issues. They just needed time to manifest.”
Fen-phen, a combination of fenfluramine and phentermine, was a popular diet drug in the ’90s. But it’s far from the only pharmaceutical failure. For example, amphetamines were once widely prescribed for weight loss, until they were linked to high blood pressure, heart complications, anxiety, and aggression. Did we mention amphetamines – street name “speed” – are addictive?
So there’s good reason for skepticism. But Koliwad – who holds UCSF’s Grodsky/JAB and Woeber-Mount Zion Distinguished Professorships – says the latest treatments really might be the solution some patients have been hoping for. The drugs work by mimicking a hormone called glucagon-like peptide-1 (GLP-1), which curbs hunger. GLP-1 also slows down the movement of food from the stomach to the small intestine – hence a feeling of fullness – and increases insulin production, lowering blood sugar. Patients with diabetes have been taking older versions of GLP-1 agonists for almost 20 years.
The gist? GLP-1 drugs make you eat less. Over time, obese patients lose roughly 12% of their body weight on Wegovy (semaglutide) and about 18% on Zepbound (tirzepatide, which targets GLP-1 and another gut hormone, GIP.) Diana Thiara, MD, medical director of the UCSF Weight Management Program, says the results can be “amazing and life-changing” for people with obesity, a condition linked to a host of health risks.
Recent studies have shown that semaglutide also helps people with obesity lower their high blood pressure and reduce their odds of heart attacks or strokes. Michelle Albert, MD, MPH, UCSF’s Haas-Stern Professor of Cardiology and past president of the American Heart Association, says it’s unclear exactly how semaglutide prevents heart attacks and strokes, and it’s uncertain whether the drug has a similar impact on patients who don’t have heart disease already. Still, she’s excited about the news.
“It’s a big deal because cardiovascular disease is the number-one killer globally,” Albert says.
Early evidence suggests the drugs might also improve depression and substance abuse disorders. Because the drugs seem to dampen inflammation in the brain, they’re now being studied as a possible way to prevent neurological diseases like Parkinson’s and Alzheimer’s, too.
2
They come with risks that we’re still learning about.
The potential side effects of GLP-1 drugs are no fun: nausea, vomiting, fatigue, diarrhea, constipation. Most patients nudge up to the recommended dose, slowly adjusting to the drugs to minimize discomfort. Thiara, who is also an assistant professor of clinical medicine, says some patients stick to a lower dose because they can’t tolerate more GLP-1 medication, which is fine. What she worries about are the patients who feel pressure to power through.
“We’re living in a world that values thinness so much,” she says. “There are patients watching GLP-1 TikTok videos and thinking vomiting and extreme nausea are normal, and they’re not.”
We’re living in a world that values thinness so much. There are patients watching GLP-1 TikTok videos and thinking vomiting and extreme nausea are normal, and they’re not.”
Albert agrees that the side effects, while mild or temporary for many, can’t be underestimated. Some people find the drugs unbearable.
“Someone I know was put on semaglutide,” says Albert. “They’re older, and they became severely dehydrated and experienced an exacerbation of their atrial fibrillation [irregular heart rhythm]. They went off the drug. It might have helped with their diabetes and weight loss. But as people age, they’re thinking not just about quantity but also quality of life.”
For others, GLP-1 agonists can slow digestion to a problematic degree. Patients have sued the drugmakers after developing dangerous conditions, such as stomach paralysis and bowel obstructions. Koliwad says these complications are incredibly rare, but it’s important for patients to know they’re a possibility.
“The stomach contents are retained sometimes for days on GLP-1s,” Koliwad says. “People facing surgery have fasted for 24 hours so they can safely get anesthesia. And physicians find there’s still food in their stomachs.”
Thiara also says the risks of taking GLP-1 medication during pregnancy haven’t received nearly enough attention, given that the majority of patients on the drugs are women.
3
They’re not meant for everyone. People have figured out how to get the drugs anyway.
The new weight loss medications are approved by the Food and Drug Administration (FDA) only for obesity, which the agency defines as a body mass index of 30 or greater. The FDA makes exceptions for patients who don’t quite meet that threshold but have a related condition, like high blood pressure. Insurers tend to have similar criteria. Of course, that doesn’t stop providers from writing “off-label” prescriptions for people willing to pay out of pocket for them.
“There are different reasons why people want to lose weight,” Koliwad says. “One is that, medically, the weight loss will allow them to be healthier. But depending on the individual, the most powerful reason might be cosmetic.”
There are different reasons why people want to lose weight.... But depending on the individual, the most powerful reason might be cosmetic.”
The soaring demand for GLP-1s has created shortages across the country. In response, semaglutide and tirzepatide were added to the FDA Drug Shortages Database, allowing compounding pharmacies to produce generic versions. In turn, telehealth companies began selling the drugs at prices far lower than the average $1,300 per month paid for brand-name GLP-1s.
New Yorker writer Jia Tolentino – who wears a size 4 – documented her experiment buying the drugs on a telehealth site. It cost her just $250 for a three-month supply: “I expected to be caught out during the Zoom appointment that I assumed was coming. Instead, a nurse practitioner named Nicole sent me a direct message laced with cheerful emojis.… I asked if she would help me manage the side effects but got no reply.”
Koliwad and Thiara are both concerned that telehealth companies rarely provide meaningful medical supervision for patients prescribed GLP-1s. In this common scenario, people are injecting the drugs at home and hoping for the best.
“We see a lot of them having problems with side effects. They show up in the emergency room or urgent care or come to specialists like me,” Koliwad says. “We have to undo problems that they have from medicines that they got in random ways.”
It’s unlikely the drugs will stay on the FDA’s shortage list forever. Eventually, the supply and demand should stabilize. When the new GLP-1 drugs come off the list, compounding pharmacies are supposed to stop selling semaglutide and tirzepatide, which will send many off-label patients scrambling for affordable medication. Some are already shifting to older, less expensive GLP-1 agonists.
4
The people who need weight loss medication the most are still having trouble getting it.
The shortages have made it difficult for some people to get GLP-1 agonists – even those with health insurance coverage for the drugs. Thiara says patients had to track down doses at far-away pharmacies last year, sometimes driving hours to retrieve a prescription.
“We still have delays, and lots of people do give up,” says Thiara, who is planning a study about health disparities in accessing GLP-1s for weight loss.
Shortages aside, many insurers still won’t pay for GLP-1 agonists unless the patient has been diagnosed with diabetes or cardiovascular disease. A 2003 law currently prohibits Medicare from covering drugs for weight loss alone. Meanwhile, states get to decide whether to cover the drugs under Medicaid. The net result? A lot of people struggling with obesity can’t afford the most effective treatment. Obesity rates are highest among Black and Latinx adults, people in rural areas, and people with low incomes.
“The populations that would benefit most haven’t even been included in the trials in significant numbers,” Albert says. “They often can’t get the drugs now because they’re expensive. And the injection alone is not a solution. It has to be partnered with lifestyle changes.”
To be clear, eating a lot less does drop the numbers on the scale. But exercise is still important – for your heart, bones, brain, and more. And the nutritional quality of your food matters, not just the quantity. Talya Kurzion, MS, RD, a clinical dietitian with UCSF Health, says patients taking GLP-1s should prioritize fruits and vegetables; whole grains; lean protein; and the healthy fats found in olive oil, nuts, and seeds.
Of course, it’s tough to put all that advice into practice. For people with low incomes – many juggling multiple jobs, caring for young children or elderly relatives, or living in areas where fresh produce is hard to come by – the hurdles are much higher.
“The time and effort component of cooking healthy meals is a big barrier,” Kurzion says. “Still, these medications do offer meaningful help. People taking them have fewer cravings. They don’t feel the calling for fast food so much.”
These medications do offer meaningful help. People taking them have fewer cravings. They don’t feel the calling for fast food so much.”
Legislative efforts to expand insurance coverage for GLP-1 medications are already underway. Even if those initiatives fail, the cost of the blockbuster weight loss medications is expected to come down in the future. Additional GLP-1s might enter the market in a few years. Several contenders are already in development, as pharmaceutical companies race to find better drugs for weight loss. For example, AstraZeneca recently spent $2 billion to license an experimental pill that might have fewer side effects than the injectable treatments.
5
GLP-1 weight loss might not look – or feel – the way you expect.
While the health benefits of GLP-1s have gotten plenty of press, their potential to help people transform themselves aesthetically has received even more attention. Until recently, it only took typing “oze” into Instagram for the suggestion “ozempick [sic] before and afters” to pop up. With it came countless makeover images – primarily of women – and tips on how to deal with “Ozempic face” (shorthand for the bitter realization that a skinnier face sometimes reveals one’s advancing age).
In short: A lot of people taking GLP-1s want to look better, and they’re toting around hopes that might not match reality. Despite setting expectations before patients start GLP-1s, Thiara says many still believe the drugs will enable them to reach their ideal weight.
“People who’ve been on Wegovy for a year or so will come to me and say, ‘Well, now I’m plateauing. What else can we do?’” Thiara says. “I’ve had this conversation like seven times in the last week. A 12% drop in body weight falls within the average. But for some people, there’s this idea of how they want to look. They’re disappointed.”
Online, speculation runs wild on what the rise of GLP-1s will mean for American culture and, in turn, our mental health. Are we devolving to a ’90s-era obsession with thinness? Will the drugs destroy the movement for body acceptance?
Jason Nagata, MD ’13, an eating-disorders expert and associate professor of pediatrics, says social pressure to look thin never really went away. Studies of teenage girls across the U.S. suggest that two out of three are trying to lose weight. For adolescent boys, the results are more complex – with a third wanting to lose weight and another third hoping to bulk up with muscle. Nagata is concerned that some people taking GLP-1s might fixate on weight loss at any cost.
Eating disorders affect people of all sizes.”
“Eating disorders affect people of all sizes,” Nagata says. “We have often seen people considered overweight or obese who start with a weight loss journey that is well intentioned. Then it becomes an obsession and gets out of control. They can lose such a significant amount of weight in such a short period of time that they develop complications from starvation and have to be hospitalized.”
Nagata suggests that patients taking GLP-1s check in regularly with a physician or nutritionist who can monitor their progress and flag unhealthy behaviors. Thiara and Koliwad, who both prescribe GLP-1s, do this. Part of what they look for is too-rapid weight loss – which, in addition to straining vital body functions, can accelerate muscle loss. Thiara’s clinic also offers counseling. Dropping a lot of weight can stir up unexpected psychological challenges.
“You can see some people mourning their previous selves,” Thiara says. “A patient told me, ‘People used to be so mean in public.’ Now, they’ve lost weight and society is treating them better. But they’re struggling with it.”
For example, when writer Elna Baker lost 110 pounds, she got a lot of attention and affirmation – but it felt flimsy. Her story on the podcast This American Life unpacked the questions that haunted her long after the dramatic makeover was complete. Did her new partner like her, or did he just like her new body? She still longed to be loved exactly as she was, fat or not.
6
Once you start taking GLP-1s, the drugmakers suggest you stay on them. Forever.
The downsides of GLP-1 medication might not seem so daunting if you only took it temporarily. Unfortunately, the existing studies are clear: People who go off the drugs eventually regain much of their lost weight. Still, insurers and many patients remain eager to define an end point for the treatment.
“The most common question patients ask me is, ‘When can I stop it?’” says Koliwad. Even patients who tolerate GLP-1 treatment just fine don’t necessarily enjoy the medication’s effects. Indulgence is, for better or worse, how many people relax, celebrate, socialize. For example, Thiara described a patient who asked if she could stop her medication for a week or two; she wanted to enjoy decadent meals and drinks during a birthday trip. Taking a break is OK, Thiara says. But if you stay off the drug, expect cravings to return with full force.
In the future, Koliwad thinks it’s possible that many people might use GLP-1s for a time, adjust their eating and exercise habits, then maintain their new weight with an “off ramp” of coaching or other support. He anticipates studies pairing GLP-1 medication with lifestyle modification programs.
“Maybe five years after they stop taking the drug, people would need another two‑year course to sustain the effects,” Koliwad says. “But that would still be a lot cheaper than taking it for their whole life.”
Thiara isn’t so optimistic. Researchers have been investigating and tweaking exercise and diet interventions for many years. Obesity has surged anyway. About a decade ago, adult obesity rates of 35% were unheard of in the U.S. A couple of years ago, 22 states exceeded that rate.
“We can’t put someone on GLP-1s for only two years and expect them to maintain,” Thiara says. “We know that doesn’t work.”
The factors fueling excess weight are complex: social, environmental, genetic. But big picture, biologically, humans evolved in scarcity. If our ancestors’ brains didn’t urge them to eat – ravenously, whenever an opportunity arose – they probably didn’t live long enough to pass along their genes. For many Americans today, food is abundant and cheap. But it’s still wildly difficult for most of us to walk away from, say, a warm cookie or a juicy cheeseburger. Some research suggests that common, highly processed foods – packed with sugar, fats, and other potentially harmful ingredients – might be almost as addictive as cocaine.
We live in a food environment that is constantly pressuring people to make indulgent decisions.”
“We live in a food environment that is constantly pressuring people to make indulgent decisions,” Thiara says. “On top of that, genetics predispose some people to having excess weight.”
GLP-1 medications have the potential to usher in much-needed nuance in how Americans understand obesity. Some believe that conversation – even amid the endless ads and op-eds and Instagram “before and afters” – is already happening.
“We’ve shifted away from attributing the problem to individual willpower,” Koliwad says. “For decades, we didn’t emphasize that. People thought that failures to lose weight were their fault when the game was rigged against them. Now the question is, how do we create a more even playing field?”
Videos: Walter Zarnowitz