Should Women Take Hormones to Manage Menopause?
UCSF gynecologists cut through the confusion.

The average woman will spend almost a third of her life in menopause. UCSF gynecologists Mindy Goldman, MD, and Tami Rowen, MD ’09, MS, explain how hormone therapy may ease the transition.
Despite being a universal experience for women, menopause often seems shrouded in stigma or confusion. But menopause is having a moment: Women today can choose from a wealth of options to address their unique needs during this time in their lives, say UCSF experts.


What is menopause?
Goldman: Menopause is defined as one year without a period. Perimenopause takes place in the years leading up to menopause. During this time, a woman may begin to have symptoms such as menstrual irregularities or hot flashes but still has periods.
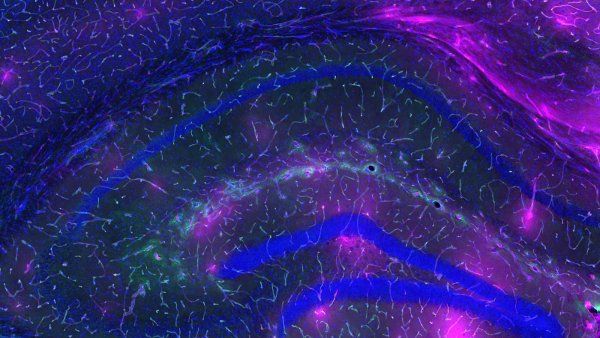
Rowen: These symptoms are caused by fluctuating and declining levels of the hormones estrogen and progesterone. Hormone therapy is medication that replaces the estrogen and progesterone the body stops making during the transition to menopause.
Women don’t understand why they are struggling at work: Why is that word on the tip of their tongue but they can’t find it? It’s not dementia; it’s menopause.”
What are symptoms of perimenopause?
Goldman: Well-known signs may include night sweats, mood swings, vaginal dryness, weight gain, and decreased sexual desire. Less common symptoms may include hair loss, joint pain, heart palpitations, dry mouth, and changes in gastrointestinal functioning.
Rowen: Another symptom women may not recognize is cognitive changes, like word-finding ability. Women don’t understand why they are struggling at work: Why is that word on the tip of their tongue, but they can’t find it? It’s not dementia; it’s menopause.
How does hormone therapy work?
Goldman: Hormone therapy includes estrogen and progesterone. Estrogen is typically the component of hormone therapy that alleviates most of the symptoms; progesterone is used if women have a uterus, as it prevents uterine cancer.
Rowen: Also, hormone therapy isn’t just pills to swallow. Oral estrogen can be associated with blood clots, so people who are at higher risk for blood clotting disorders should not be taking estrogen pills. But estrogen can also be given topically – via a skin patch, cream, gel, spray, or vaginal ring – which bypasses the liver and reduces the possibility of blood clots.
Goldman: Perimenopausal women should also keep in mind that the dosage of hormones in hormone therapy is lower than in birth control; it’s not an adequate form of contraception.
Does hormone therapy benefit the body in other ways?
Goldman: Yes. Hormone therapy can have many other benefits: Progesterone can help with sleep, estrogen can help prevent bone loss, and if started around or soon after menopause, can prevent heart disease and possibly cognitive loss.
Why did hormone therapy fall out of favor?
Rowen: After menopause, women’s heart disease risk increases. More than 20 years ago, the Women’s Health Initiative (WHI) study, a long-term national health study focusing on ways to avert heart disease, breast and colorectal cancer, and osteoporosis in postmenopausal women, aimed to assess hormone therapy’s effectiveness in preventing heart conditions.
Goldman: The intentions of the study were good: Researchers were evaluating whether the use of hormones prevented heart disease, the most common cause of death. But in 2002, the press published findings suggesting that the combination of estrogen and the specific type of progesterone the WHI study used increased the risk of breast cancer and didn’t prevent heart disease.
Yet what didn’t get publicized was that estrogen decreased the risk of breast cancer.
So, is there a link between hormone therapy and breast cancer?
Rowen: Hormone therapy will not necessarily increase the risk of breast cancer – we know that specifically for estrogen alone, though the role of specific types of progesterone is more complicated, and there is likely a risk. However, it doesn’t mean a woman won’t get breast cancer on hormone therapy. I want to be very clear about that: One in eight women will get breast cancer – but not necessarily because of hormone therapy.
Women considering hormone therapy should speak with their health care provider to develop a plan specific to their personal health history.
Is there a good time for women to start and stop hormone therapy?
Goldman: If a woman begins hormone therapy within 10 years of menopause or before age 60, the benefits usually outweigh the risks. And there’s no reason to stop based on age. But as women get older, they may develop cardiovascular risk factors. For example, if you have plaques in your arteries or a history of blood clots, the use of estrogen is felt to be risky.
Rowen: Yet if you take estrogen before artery plaque buildups are formed, research shows it can prevent cardiovascular disease.
Goldman: I also don’t want to imply that anyone who is over age 60 can’t take hormones. Everyone’s individual circumstances are different.
Does estrogen prevent bone loss?
Rowen: Yes. Absolutely. Estrogen can help maintain bone density. There is no study that has not shown that estrogen is protective of bone health.
How reliable are blood tests to measure hormone levels?
Rowen: Not at all reliable. During perimenopause, your ovaries are like a sputtering car; you’ve got your foot on the gas, but it comes out erratically. Tests for estrogen and follicle-stimulating hormone – the hormone that tells your ovaries to make estrogen – often show inconsistent results.
During menopause, however, I will check a patient’s hormone levels if I’m treating them with hormone therapy and they don’t seem to be responding to it, or if they’re having side effects. It helps to assess if someone is absorbing the medication properly.
Who shouldn’t take hormone therapy, and what are some alternatives?
Rowen: I don’t recommend it to anyone who has cardiovascular disease or a hormone-sensitive cancer that uses hormones to grow, such as some forms of breast, ovarian, uterine, or endometrial cancer.
Goldman: If you can’t take hormones, you may need to find other treatments for your individual symptoms.
In May 2023, the FDA approved Veozah, a new medication to decrease hot flashes. It works by blocking neurotransmitters in the brain that regulate heat and cold sensitivity. Other studies have shown symptom improvement from low doses of some antidepressants and neuropathic pain relievers, as well as anti-seizure, overactive bladder, and blood pressure medicines.
How can women maintain sexual health?
Rowen: I encourage women to continue to maintain sexual activity as much as they feel like they’re able to. I don’t ever want anyone to have sex if they don’t want to, but the truth is, the healthiest thing for your sexuality is to stay sexually active. It’s incredibly good physically. It releases neurotransmitters associated with sexual desire. It’s very good for the vagina. It bonds you with your partner by releasing a hormone called oxytocin.
But if sex hurts, you’re not going to want to do it. Vaginal dryness can be treated with topical estrogen creams or inserts, or various lubricants. If it’s truly a medically based lack of desire and not due to other medical or relationship factors, there are drugs that are approved for pre- and perimenopausal women, such as Addyi and Vyleesi.
Don’t assume you have to suffer through menopause symptoms or ignore how you feel and think, ‘This is just part of aging.’”
What advice would you give women during this time in their lives?
Rowen: Stay physically active. Cardiovascular disease, cancer risk, sleeplessness, sexual dysfunction, depression, and anxiety all improve if you move more. And not only cardio; women should build muscle mass, too, to protect their bones. You don’t need to take up bodybuilding in your 60s, but resistance training is important.
Goldman: Don’t assume you have to suffer through symptoms or ignore how you feel and think, “This is just part of aging.” Find a provider who understands perimenopause to help you figure out if your concerns are related to it.