In the winter of 2015, at the beginning of his first term as surgeon general of the United States, Vivek Murthy, MD, embarked on what he called a “listening tour of America.” In cities and towns across the country, he sat down with people from all walks of life – parents, teachers, business owners, philanthropists, community leaders – and asked what health issues troubled them most.
As the nation’s doctor, he was prepared to hear about problems like diabetes, mental illness, infectious outbreaks, and the opioid epidemic. And he did. But he also picked up on a common complaint that he hadn’t anticipated. This affliction, he later wrote, “ran like a dark thread through many of the more obvious issues that people brought to my attention.” Most people didn’t identify it as a health concern, but Murthy understood that it was causing them great pain and, in some cases, making their other ailments worse.
What unites so many Americans, he realized, noting the irony, is loneliness.
We’ve all felt it from time to time – that ache of wanting to be close to other people, to belong, to be loved. When it persists, it strains our hearts and spreads inflammation, damaging our tissues and blood vessels. And the impacts on our health can be profound.
Research consistently shows that prolonged loneliness and isolation (a distinct but similarly fraught experience) increase our risk for cardiovascular disease, immune dysfunction, insomnia, stroke, dementia, depression, and anxiety. It’s no wonder that lonely or isolated people are also more likely to die young. According to a massive analysis of 70 studies with more than 3.4 million participants, loneliness and social isolation raise the chance of early mortality as much as smoking and obesity.
Ashwin Kotwal, MD, MS, a geriatrician at UC San Francisco, is one of a growing number of physician-scientists who have been calling on health systems to address patients’ fundamental need for human connection. “A lot of us have been screaming from the rooftops for a while that this is important,” he says. When I visited him earlier this year at the San Francisco VA, he was still dealing with the fallout of the pandemic lockdown. “When patients didn’t see their family members for many months, they really declined,” he told me. “Their dementia got worse. They developed pressure injuries because they weren’t getting out of bed as much. The use of antipsychotics increased a ton.”

As a palliative specialist, Kotwal often helps patients prioritize meaningful social activities, such as attending a daughter’s wedding or a grandson’s graduation. “What people care about at the end of life is not being alone, probably more than not being in pain,” he says. Only recently, though, have health care providers at large begun to see loneliness as a serious health concern. “Many clinicians didn’t understand how it was our responsibility to do something,” he says. “The feeling was, ‘This is outside the scope of our clinical practice.’”
Kotwal’s UCSF colleague Carla Perissinotto, MD, MHS, a fellow geriatrician who helped train him in the field, was one of the first researchers to get a paper on loneliness accepted by a medical journal. Her landmark study, published in 2012 in the Archives of Internal Medicine (now JAMA Internal Medicine), found that loneliness predicts worsening disability and death in people over age 60. “There was a lot of skepticism in the medical community,” she recalls, even though social scientists had been documenting the phenomenon for decades. Often, when she would present her results at scientific conferences, physicians in the audience would dismiss them, saying “This isn’t a big deal” or “It’s just depression.”
Perspectives have shifted as evidence of a loneliness epidemic has mounted. The prevalence of loneliness has risen steadily since the 1970s, when Americans began consuming more digital entertainment – such as television, and later, social media – and participating less in social and civic activities, such as going to church or joining a labor union or bowling league. Today, almost half of U.S. adults say they are occasionally lonely, and about 1 in 10 are frequently lonely – far more than the number with other chronic conditions, including heart disease and cancer.
After his national tour, Murthy sounded the alarm, as did several prominent health organizations. COVID-19 drove home the urgency of their message. As rates of loneliness spiked because of social distancing, many physicians saw for the first time how isolation could exacerbate frailty in an elderly patient or erode the mental health of a young one. “If there’s a silver lining to the pandemic, it’s that there’s now an explosion of interest in addressing this problem,” Kotwal says.
Yet even as doctors increasingly recognize loneliness as a public health crisis, they face a thorny question: How, exactly, do you help a patient who is lonely? “It’s much easier as a physician to say, ‘Oh, you have high cholesterol. Here’s your statin,’” Perissinotto says. But what do you prescribe for social distress?
Better Than a Pill
Last July, Perissinotto hosted a retreat at the UCSF geriatrics division for a half-dozen employees of the Curry Senior Center, a community nonprofit in San Francisco’s Tenderloin district. Her husband, who is a chef, had prepared a lunch of roasted chicken and cauliflower, a kale and wheatberry salad, and hand-rolled pasta made with flour he had milled himself. “The shape is strozzapreti, which means ‘strangled priest,’” she delightedly informed the group.
Nearly a decade ago, Perissinotto, a natural socializer, began building relationships with the Curry Center and other Bay Area organizations that foster social connections. These hard-earned partnerships have allowed her, together with Kotwal and others, to start studying loneliness intervention programs alongside the people who run them. “As medical academics, we often forget that the answers are in the communities we serve,” she says. Her goal is to identify the strategies that work and determine how to replicate them.
The assembled Curry employees included former salespeople, tech workers, insurance agents, and social service administrators. They now staff a program that pairs them with elderly residents in and around the Tenderloin who are lonely or socially isolated. Because the staffers share some of the same interests and experiences as their clients – they might be part of the LGBTQ+ community, say, or also be coping with mental health issues – they refer to themselves as peers. That’s not to say that just anyone with a common background can do this work. Although the positions don’t require formal qualifications, most of these Curry employees are trained in peer support, a specialization newly recognized by the state of California that entails skills like conflict resolution and trauma awareness.
As the food warmed in the oven, Perissinotto introduced herself. The peers have been working with her team to collect data on the Curry program for several years now, sharing their reflections and surveying each other’s clients every six months, but this was the first time that many of them had met her or heard the backstory of the UCSF-Curry collaboration.
“I became interested in loneliness really by chance,” she told them. “Obviously, I knew about it because we all experience it at some point our lives, but I’d never asked about it in a clinical setting.” Then one day, during her residency, she stumbled upon a questionnaire developed by researchers at UCLA to measure loneliness, and she had an epiphany. “It was like, ‘Why aren’t we talking about this in medicine? And what do we do about it?’ Fast-forward to seven years ago, when I met Daniel.”

Daniel Hill, a Gandalf-like figure in his early 60s, has managed Curry’s peer program since its inception in 2015. Before that, he’d been employed at a homeless services organization, but after a shooting at his office, he became afraid to leave his house and stopped going to work. He eventually took another job, in AIDS hospice care, then was laid off and “sunk right back into that place of depression and isolation.” Nevertheless, he “went through the motions” of applying for jobs in order to get unemployment benefits and ended up landing the one at Curry.
The role was a perfect fit, though it took Hill a while to realize it. “Me being a peer is one of the closets I’ve had to come out of,” he later told me. “I don’t know if it was shame so much as a recognition that PTSD and major depression weren’t things you talked about in the workplace. But then I saw how my staff was using their experiences to uplift others, and I was inspired. I started saying, ‘Yes, I’m a peer too.’”
In 2017, the Curry Center was looking to evaluate the impact of Hill’s program to help raise funding, which is how he got put in touch with Perissinotto. “I just kind of thought we were this old hippie, granola program run out of a basement in the Tenderloin,” he explained at the retreat. “And then Carla comes along, and the next thing you know…”
“…I’m bringing you coffee and lunch,” she interjected with a laugh.
“And we start talking about validated measures, and then the questionnaires come out, and all of a sudden we were able to translate granola into diamonds, you know what I mean?”
By diamonds, Hill means data. For two years, the research team had surveyed 74 participants in the Curry program who ranged in age from 59 to 96. After the team tallied the input, the results were unequivocal: Peer support increased social interactions and reduced feelings of loneliness and perceived barriers to socializing, such as physical ability, cultural difference, and mood. By the end of the study period, the incidence of depression had dropped from 38% to 13%.
“I knew we were helping people,” said Hill, who is a co-author on the 2021 paper reporting the finding. “But this was like, ‘Whoa.’ And Carla – I love her – she goes, ‘Show me a medication that will do that.’”
I just kind of thought we were this old hippie, granola program...And then Carla comes along, and the next thing you know...we were able to translate granola into diamonds.”
Daniel HillManager of the Curry Senior Center peer program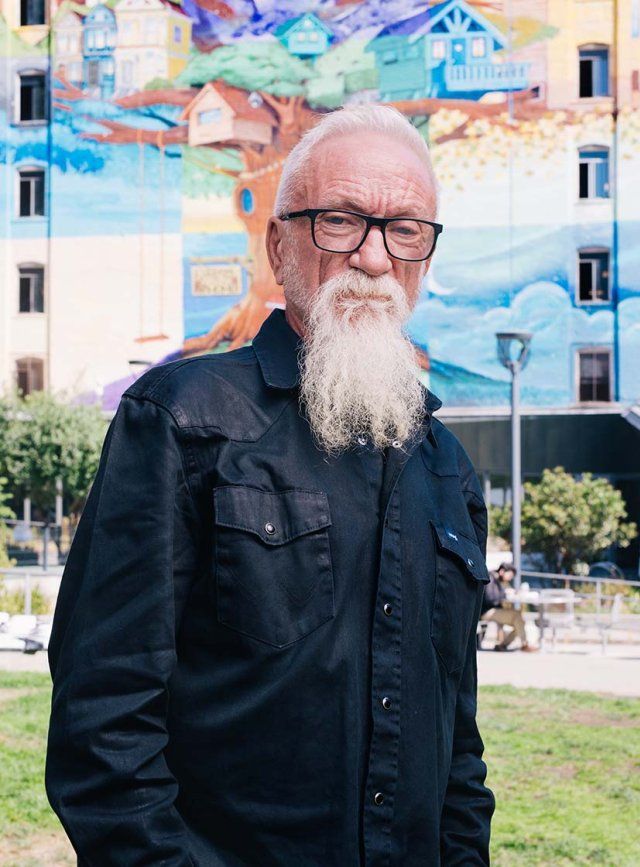
A Professional Friend
A few weeks after the retreat, I met Alessia Furlow, one of the Curry Center peers and Hill’s assistant manager, at her office in the Tenderloin. Though it’s known for seediness and crime, the neighborhood is a place of multitudes. Vibrant, stories-high murals adorn its drab brick facades, some of the last refuges of affordable living in the city. Children shoot hoops, dealers hawk fentanyl, and old men play dominos and practice tai chi. Commuters jostle past shoppers and parents pushing strollers, while people down on their luck slump under storefronts advertising pupusas or money orders or bánh mì or live jazz.
Furlow, who is in her 30s, had agreed to introduce me to one of her clients, a 73-year-old named Maggie Hosmer. Despite the age gap, Furlow says she finds it easy to connect with older residents. “I love to laugh,” she says. “So I think I just come across as open and fun.” She will join clients for coffee or lunch, stroll with them to a park, or just sit and chat with them in their homes – whatever they’re up for. “There’s no agenda,” she says. “It’s about cultivating trusting relationships.”
There’s no agenda. It’s about cultivating trusting relationships.”
On our way to Hosmer’s apartment, Furlow took a detour to show me the Cadillac Hotel, where many of the seniors in Curry’s peer program live. When it opened in 1907, the Cadillac was billed as San Francisco’s “most select” luxury inn, featuring 180 rooms and a grand ballroom. But after the neighborhood declined in the 1960s, the building became a residential community, with staff providing social services to tenants – a role now filled by Curry Center case managers.
In the lobby, an eight-piece swing band was setting up for a concert. “Oh, hey, Sonya, how are you doing?” Furlow greeted a case manager in a Warriors T-shirt.
“I case manage everybody on the fourth floor,” Sonya Lister told me, adding that she refers tenants to the peer program whenever they seem cut off from the bustling community around them. “It’s a phenomenal program,” she said. “It really helps people come out of their shell.”
When we arrived at Hosmer’s place, a small sunlit studio in the nearby Fillmore district, she welcomed us wearing a blue turtleneck, black slacks, and slippers. Her gray hair was cropped short, and she wore tiny gold hoop earrings. Hanging by her bed was a popular 20th-century print by Maxfield Parrish that depicts a naked figure bending over a young woman in a dreamy Grecian scene. “A lesbian classic,” she quipped.
Gay culture is something that she and Furlow had quickly bonded over. Before they met in 2021, Hosmer was spending her days holed up at home reading. She’d lost touch with her family, and most of her friends had died or moved away. “So I’d go to the library every month and get lesbian novels and whodunits, and I’d just read them from eight in the morning to six at night,” she told us. “I’d get real lonely, but I didn’t recognize what it was.”
Then one day, she went to the Social Security office to check on her benefits, and the door was boarded up. Same thing at the bank. She waited for the bus, but all the drivers refused to stop. “Finally, somebody came along and said, ‘You don’t have a mask. That’s why the bus keeps going by you.’” She hadn’t known that a pandemic had broken out or that businesses were shuttered due to protests over the killing of George Floyd.
She called the Curry Center so she could read the news online and heard they had a technology program. “I said, ‘I want a tablet and a lover,’” Hosmer recalls.
“So I got the tablet,” she says, and then grins. “I’m still working on the lover.”
What Curry did offer was a peer. Furlow was one of the first people Hosmer had hugged in a long time. She helped Hosmer sign up for dating sites and warned her about romance scams. They binged on The L Word and watched Screaming Queens, a documentary about a little-known uprising by drag queens and trans women in the Tenderloin in 1966. They sat on Hosmer’s bed eating mango strips and Thai chili almonds and talked like girls at a slumber party.

Lately, Hosmer has been reaching out to more people. She started going for walks and out to eat with another client of Furlow’s. She invited a former coworker to join her for a haircut and reconnected with an old friend who shares her love of music and poetry. And she got a cat, a gray-and-white tabby named Sheba. “Right now, my life is kind of settled,” she said. Rarely does she feel the twinge of loneliness anymore.
Before we left, I asked Hosmer how she thought about her relationship with Furlow. Who was this warm, supportive person to her?
She turned to her peer. “I consider you a friend,” she told Furlow. “Would that be weird if I said, ‘This is my friend Alessia?’”
“No, that’s not weird at all,” Furlow replied. “I mean, it’s part of my job, right? But I definitely feel like there’s a companionship. There’s that intimacy of friendship, for sure.”
What Doctors Can Do
Curry’s peer program works precisely because it’s so informal. When the UCSF team analyzed in-depth interviews with clients and peers, they found that almost all the participants used the word “friend” to describe their peer. The program’s flexibility and agenda-free ethos, the researchers wrote, “facilitated trust and gave clients a safe space to build skills and confidence.” Clients felt that the peers genuinely cared about them and didn’t judge or condescend to them, as other service providers sometimes did. (As one peer put it, “I’m not a doctor talking down to you, like, ‘Oh, you need this and that, and here’s your problem because I say so.”)
The program’s creators had assumed that would-be clients were isolated because they weren’t getting services like counseling and mental health care. But that wasn’t the case. “What we discovered was that everybody’s connected to services,” Hill says. Most clients, it turned out, already had doctors and therapists and case managers, and they didn’t want any more. (“I have enough,” one client said.) The problem, in other words, wasn’t that lonely people weren’t being referred to providers; it was that their providers weren’t referring them to programs like Curry’s.
One reason is stigma. “No one wants to raise their hand and say, ‘Hi, I’m Daniel. I have no friends,’” Hill says.
And most providers don’t ask. Clinicians often worry that bringing up loneliness and isolation will make patients uncomfortable, says pediatrician Matt Pantell, MD ’13, MS, who studies social drivers of health at the UCSF Center for Health and Community and with the UCSF Social Interventions Research and Evaluation Network.
But that fear is probably unfounded. In a 2021 study of more than 250 patients recruited from primary care clinics nationwide, Pantell and his colleagues reported that 94% of subjects said they wouldn’t mind being screened for social isolation. “In general, patients are very open to being asked about social factors in clinical settings,” he says.
Of course, asking is just the first step. Some physicians might be hesitant to discuss loneliness and social isolation, Pantell says, because they don’t have good answers. “There’s no perfect solution for everyone,” he acknowledges. But helping a patient find one starts with getting to the root cause, something doctors are well-trained to do. And the fix might be surprisingly simple. Maybe a quiet grandmother just needs a hearing aid so she can talk with her grandkids. Maybe a shy tween needs a ride to play sports with his friends. Maybe the patient has their own ideas about what they need.

Meanwhile, social prescribing – recommending community resources or activities that can help address social needs – is burgeoning. A prescription for loneliness could be a referral to a peer program like Curry’s, a support group, an after-school club, or even a robotic pet. To make referrals easier, UC hospitals and other medical centers are starting to link databases of community service organizations with electronic medical record systems, Pantell says. “There are a ton of amazing interventions that most clinicians have no idea exist.”
Elena Portacolone, PhD ’11, MPH, MBA, a sociologist at the UCSF School of Nursing’s Institute for Health and Aging, says that health care providers could also do more to prevent patients from becoming severely lonely or isolated in the first place. Patients are particularly vulnerable after being diagnosed with a serious illness, she says, especially if they live alone.
In her own research, Portacolone has interviewed nearly 100 older adults living alone with cognitive impairment, a reality for 4.3 million people in the U.S. Many of them have become so withdrawn that they are difficult to find, and she’s learned to rely on tips from emergency responders, librarians, and even cockroach inspectors. Suicidal thoughts among her subjects, she says, are sadly common.
“These people are struggling with chronic uncertainty and frustration about not knowing what’s going on or what to do,” Portacolone says. “The diagnosis should be a moment where providers can help create or foster a deeper support network.”
Good Medicine
Five years ago, just as the project with the Curry Center was getting off the ground, Ashwin Kotwal called on a patient at an assisted living facility. “She was an older woman in her 90s, a veteran,” he recalls. He’d been summoned because she wanted to use the End of Life Option Act, a California law that allows people who are terminally ill to request an end-of-life drug from their doctor.
This was surprising because the woman wasn’t terminally ill. Although her vision was waning and she used a wheelchair, she was otherwise in fair health. She had children and grandchildren who visited her often.
When we start to recognize the value of human connection, we can make a huge difference in the quality of people’s lives.”
“But as we talked, I learned that she had completely lost her sense of belonging because her disabilities had prevented her from being able to volunteer in her community,” Kotwal says. Helping people had given her a sense of purpose, of connection. So instead of a pill, he prescribed her a gig taking calls for Friendship Line, a California hotline that lends a sympathetic ear to older adults feeling lonely or depressed. Over time, and with more care, her spirits lifted, and she no longer wished to die.
“When we start to recognize the value of human connection, we can make a huge difference in the quality of people’s lives,” Kotwal says. Programs like Curry’s have long understood this. But they’re tiny, underfunded, and under-professionalized – “granola” ventures scraping by on the sidelines of medicine’s shiny arena. “People outside of health care have developed a tremendous amount of expertise,” he says, and it’s time that physicians catch on. “It’s actually good medical care.”