The orthopedist was yelling in Leeann Bongiorno’s face: “There’s nothing wrong with you! You just want drugs!”
But Bongiorno wasn’t asking for drugs – she simply wanted help.
For two years, Bongiorno, 54, had been living with pain that she describes as a deep burning sensation far worse than kidney stones or natural childbirth. “They can give you a little something to take the edge off childbirth. I never had anything to take the edge off the leg pain.”
By the time of Bongiorno’s encounter with the orthopedist, she had been to four doctors seeking relief from her excruciating pain. They all asked the same question: What happened? The frustrating part was that Bongiorno couldn’t think of anything that had set off the pain. One day it was just there.

“That’s exactly what’s complex about it,” explains neurologist Cindy Chai, MD, a pain medicine specialist and associate professor of anesthesia at UC San Francisco. “People can have neuropathic pain from dysfunctions of the nervous system without an identifiable injury to the nerve. It can happen gradually or suddenly.”
Stories like Bongiorno’s are far from rare. She is one of 17 million adults in the United States, almost 9% of the population, who suffer from high-impact chronic pain – pain so severe it disrupts their daily life. Even more people, about a quarter of the population, suffer from chronic pain, which persists continually or intermittently over three months or more. And that number is rising. It went from 20% of adults in 2016 to 24% in 2023.
But pain isn’t just a lingering symptom. It’s a disorder of the nervous system – and UCSF researchers are looking for biomarkers to identify, measure, and predict pain while developing new ways to retrain how the brain experiences it.
Acute pain is so universal that it’s the most common reason people seek medical care, and it’s usually fairly straightforward. If someone has an abscessed tooth, for example, the cause of the acute pain is clear. Chronic pain can also have obvious sources, like arthritis. But with high-impact chronic pain, figuring out the cause is often more complicated. “Fundamentally, in chronic pain relief, we lack a lot of knowledge about which part of the nervous system is producing the pain,” says neurologist Prasad Shirvalkar, MD, PhD, also a pain medicine specialist and associate professor of anesthesia at UCSF.
Even when the source is known, there’s no guarantee that the available treatments will work. Anesthesiologist Christopher Abrecht, MD, the chief of pain medicine and medical director of UCSF’s Center for Pain Medicine, says treatment is largely trial and error. The source of Bongiorno’s pain turned out to be sciatica, and she did everything her doctors told her to do – physical therapy, acupuncture, and medications – but they didn’t work. “Nothing could touch the pain,” she says.
Finally, stymied as to how to help Bongiorno, the doctor who’d yelled at her suggested she go to UCSF. In 2020, orthopedic surgeon Sigurd Berven, MD, a professor of surgery, performed a spinal fusion to relieve Bongiorno’s sciatica. The surgery was a success, and at last, after two years, she was pain-free – for about a month.
Pain wasn’t finished with Bongiorno yet.
When pain becomes the disease
Historically, pain was seen only as a symptom or warning of some other disease or as the result of an injury. “If you have pain in your arm from a fracture, the fracture is the problem.... And if you treat the underlying condition, the pain gets better,” Abrecht says.

But sometimes the pain doesn’t get better. For instance, a fractured bone could heal perfectly following treatment, yet the pain could persist. Or two people, similar in age and health, can have the same surgery, but only one might end up with lasting pain. Or a patient might undergo a successful surgery, only to develop chronic pain at the surgical site. “We don’t know what’s wrong – everything looks good – but the patient is having severe pain,” Abrecht says. This was the case with Bongiorno. Her original pain had run down the back of her right leg; the new mystery pain ran down the front of her leg. Within six weeks of surgery, the pain was even worse than the sciatica pain had been.
When pain inexplicably persists, it ceases being a symptom and becomes a syndrome in its own right. “Pain can be a helpful, natural experience that is a protective mechanism for the body, but it can also be a pathologic condition of its own,” Abrecht says.
It’s all in your head – literally
Whether it’s a symptom or a condition, pain seems straightforward: A person steps on a nail and then feels pain. But pain is more complicated than that; it isn’t actually experienced until it’s processed in the brain.
Before a person feels pain, pain receptors in the body release neurotransmitters that send signals up the spinal cord and then to the thalamus, the brain’s relay station. The thalamus processes the signals, which then travel to other parts of the brain (resulting in the perception of pain), and the brain then sends messages back to the body. Here’s where it gets complicated: These messages are shaped by a complex set of factors, including the person’s genetics, memories of past episodes of pain, environment, and emotions – all of which influence how they feel the pain. Those factors can either amplify or mute the pain signals.
If the nail grazes the person’s toe, for example, there might be some pain – but the perception of the situation is what drives the pain. If the nail sticks out of the person’s shoe and has blood on it, they could think the nail had pierced their foot and perceive a great deal of pain. Or they could take off their shoe and see that the nail had only grazed their toe and perceive less pain. In both cases, the biology is exactly the same but the perceptions are different. And all of this happens in a nanosecond.
Click on the numbers to learn more. Illustration: Farah Hamade
“It’s in your mind, essentially,” Abrecht says. “When you hear that pain is ‘just in your brain,’ that translates to people as ‘You think I’m crazy and I’m making it up,’ which is not the case. Pain is a complicated experience, and many factors are involved – and some of those are modifiable and some are not.”
Breaking pain’s vicious cycle
Everyone feels pain differently, but one universality is that people with debilitating chronic pain are often consumed by it.
“One patient told me it feels like a million paper cuts – there’s the pain component and then there’s the suffering, the overwhelming weight of this unrelenting sensation that takes up all of their energy,” Chai says. They’re unable to do anything other than think about and manage their pain. “It’s not unusual for patients to say, ‘If you can just take away my pain for an hour, I will feel better.’ It’s this kind of oppressive burden,” she says.
Many of those with chronic pain can’t work or maintain relationships, which creates a vicious cycle. Without social support, someone to care for them, or feeling valued in society, they can become depressed and anxious, which makes the pain worse. Chai explains that pain, mood, and sleep are intimately related, overlapping like a Venn diagram.
In some cases, chronic pain may lead to central sensitization, which is when the central nervous system becomes overly sensitive to stimuli. In other words, the brain learns pain too well, Chai says.
“Here’s the thing. Acute pain is necessary for life because it’s the alarm system to tell you that something is wrong,” she says. “But in chronic pain cases, it’s like the check engine light in your car that never turns off. The problem is not your engine – it’s the light.”
Pain psychologists help teach patients ways to unlearn their pain, to retrain their nervous system so they’re experiencing sensation without the associated suffering.
“If you are sitting in a chair, if you want to, you can feel the sensation of the chair against your back,” Chai explains. “But until I said that, you probably weren’t thinking about it at all because our brains are wired to block out sensations that aren’t useful.”
For chronic pain patients, though, the brain interprets even neutral sensations as pain and suffering. In effect, pain psychologists help patients retune their sensitivity to their check engine light, giving them tools to reprocess pain, to get in touch with their nervous system and take control of some of the things we normally don’t think about.
Attacking chronic pain from all angles
Chai says that patients who have chronic pain are best served in a comprehensive pain center with multidisciplinary providers. “And by multidisciplinary, I mean pain physicians with different training backgrounds, pain psychologists, and physical therapists.”
Both she and Abrecht stress the importance of holistic, personalized care, which is a longtime hallmark of UCSF’s Center for Pain Medicine. Treatments often combine medications, delivered in various ways, that can decrease inflammation and the sensitivity of the nervous system. Nerve blocks can also be used, both diagnostically and therapeutically, to target pain. Cognitive and psychological approaches, along with complementary therapies like massage, acupuncture, or aromatherapy, may be part of the plan as well.
The use of opioids presents a particular challenge. Many patients are afraid to take them for fear of addiction, says Christine Miaskowski, RN, PhD, an expert in pain and symptom management and UCSF’s Lamb Professor. She works with cancer patients and says that fear is a real challenge that must be overcome. “I tell people, ‘You’re not sleeping, you’re not eating, you can’t enjoy your family.… Would you tell me that you would be afraid to take your insulin if you were a diabetic and needed insulin?’”
The search for a biomarker
One of the biggest challenges in treating chronic pain is its invisibility: It doesn’t show up on any scan, and there’s no quantitative test to measure it. That’s why finding a reliable biomarker – an objective signal that indicates how much pain someone is feeling in real time – is what Shirvalkar calls “one of the holy grails of pain research.”
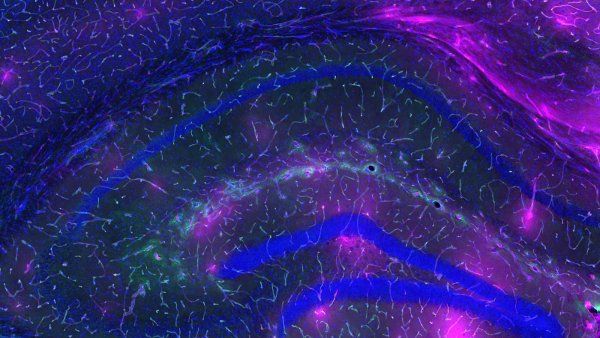
In his lab, he studies brain activity using tiny electrodes implanted in the brain to decipher which areas and circuits harbor important signals related to each patient’s pain. This dual-purpose research allows his team to both study the fundamental biology of pain and develop potential treatments.
A breakthrough came in 2023, when Shirvalkar’s team implanted electrodes in the brains of four patients who then tracked their pain at home. Patients reported the level and location of their pain and their other symptoms multiple times a day, while also capturing 30-second snapshots of their brain activity with the press of a button on a remote provided by the study. Using this data and machine learning, the team was able to predict, based solely on brain signals, when each patient would experience a high or low pain state.
Notably, they were predicting real-world chronic pain. They also discovered that the signals for acute and severe chronic pain are distinct – not just a more enduring version of the same thing, Shirvalkar says.

Now that they’ve shown they can track signals in the brain and predict when someone’s going to be in significant pain, the team is developing a pain “thermostat” using deep brain stimulation (DBS). “We’re taking those signals and, when the brain activity in real time indicates someone might be having a higher pain episode, we trigger the stimulator to turn on and short-circuit that activity,” Shirvalkar says. His team is currently testing the feasibility and effectiveness of this approach, called DBS closed-loop therapy. “We’re using this technology to try to develop biomarkers that might help predict who might respond to what therapy and what their long-term outcomes might be,” Shirvalkar says.
The ultimate goal is to personalize DBS closed-loop therapy using these biomarkers while reducing the chance that the brain becomes desensitized to the effects. “Hopefully, by making it like a thermostat, we’re delivering therapy only when it’s needed and thereby preventing the brain from learning to ignore it,” Shirvalkar says.
Rewiring relief: high-tech hope for chronic pain
Less than a year after Bongiorno’s surgery, her mysterious new pain was so bad that her right knee would buckle when she stood. Eventually, she stopped leaving the house. “I lost friends. I was sitting on the sidelines as my life went by,” she says. None of the treatments were working, so Bongiorno’s team sent her to Shirvalkar.
I was thinking,‘Is this how my life is going to be? I can’t live like this.’ But Dr. Shirvalkar said, ‘I’m going to stay here with you, and we’re going to figure this out.’ He gave me hope.”
Bongiorno says she walked into his office literally broken, like a kicked puppy. “I was thinking, ‘Is this how my life is going to be? I can’t live like this.’ But Dr. Shirvalkar said, ‘I’m going to stay here with you, and we’re going to figure this out.’ He gave me hope.”
At that first appointment, Shirvalkar explained neuromodulation – a technique that uses electrical impulses to disrupt pain signals traveling along nerves. Nerves are like electrical cables that carry signals to the brain but that can transmit only so much information at once – just as bandwidth determines the amount of data that can be transmitted over an internet connection. So the idea is to overwhelm the bandwidth of the nerves to block or quiet the pain signals.
For localized pain, doctors might use peripheral nerve stimulation (PNS), placing a thin wire electrode less than a millimeter thick near the affected nerve. The electrode sends tiny, rapid electrical pulses that produce mild tingles which essentially replace the pain. For more widespread pain like Bongiorno’s, spinal cord stimulation places two tiny wire electrodes in the epidural space of the spine. “It’s like a pacemaker for your spine,” Shirvalkar says.
Patients first try a temporary external device. If it reduces pain by at least 50%, permanent electrodes are surgically implanted. A small battery-powered generator is also implanted in the patient’s abdomen or buttocks and then controlled by a remote.
Bongiorno agreed to try spinal cord stimulation at that first appointment and received a temporary device just two weeks later. About a month after that, in early 2021, she received the permanent electrodes and generator.
Neuromodulation works for some people but not others, and experts don’t have a good understanding of why its effects are so variable. Patients and clinicians work together to find the right settings.

For her first year with the stimulator, Bongiorno used a high frequency, which had no effect on her pain. “It was awful because you get your hopes up, you think this is the answer, and it’s not working,” she says. “You feel guilty and shameful for not getting better. It was frustrating because the trial worked for me. I assumed the permanent stimulator would be put in, and I would go about my happy life,” Bongiorno says. But she didn’t give up because she had faith in Shirvalkar, who was in constant contact with her as they adjusted the settings. “I would always leave his office more hopeful than when I walked in.”
After about a year of no improvement, they switched her stimulator to a lower frequency – and, boom, that was it. “From my waist to my toes, I vibrate, and I can increase or decrease the intensity. I’m telling you, it sounds weird, but that works. I have zero pain.”
Living pain-free for the past four years, Bongiorno is no longer sitting on the sidelines. She’s back to playing tennis, walking, sailing, and playing with her grandchildren. In a recent note to Shirvalkar, she wrote, “In December, we completed our fifth solo sailing trip through the Grenadine Islands. I owe it all to you. [The spinal cord stimulator] literally changed and saved my life.… I am living my best life and enjoying it to the fullest. Words cannot describe.”
“I never thought life would be this good,” Bongiorno said in a subsequent conversation. “You can’t keep me down.”