We are not alone, but you probably knew that already.
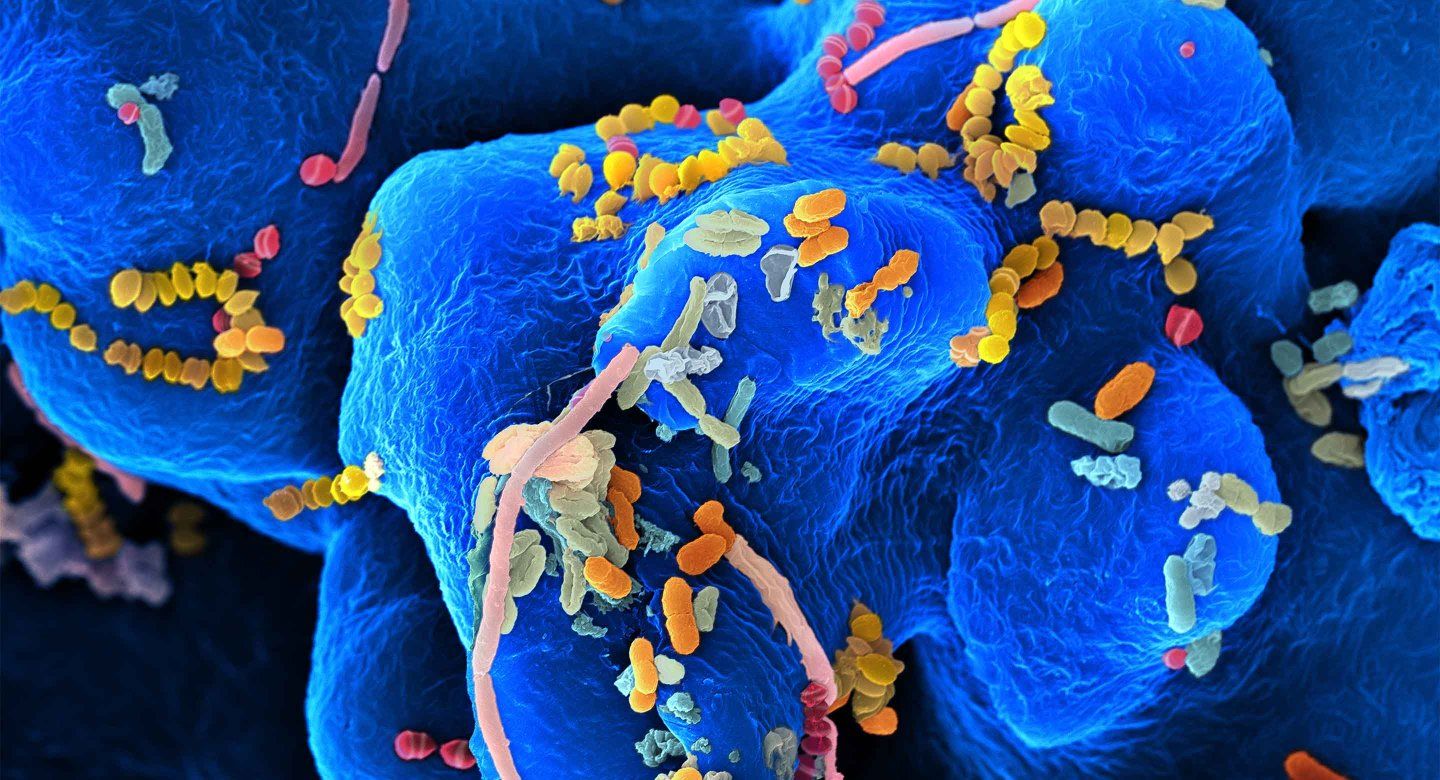
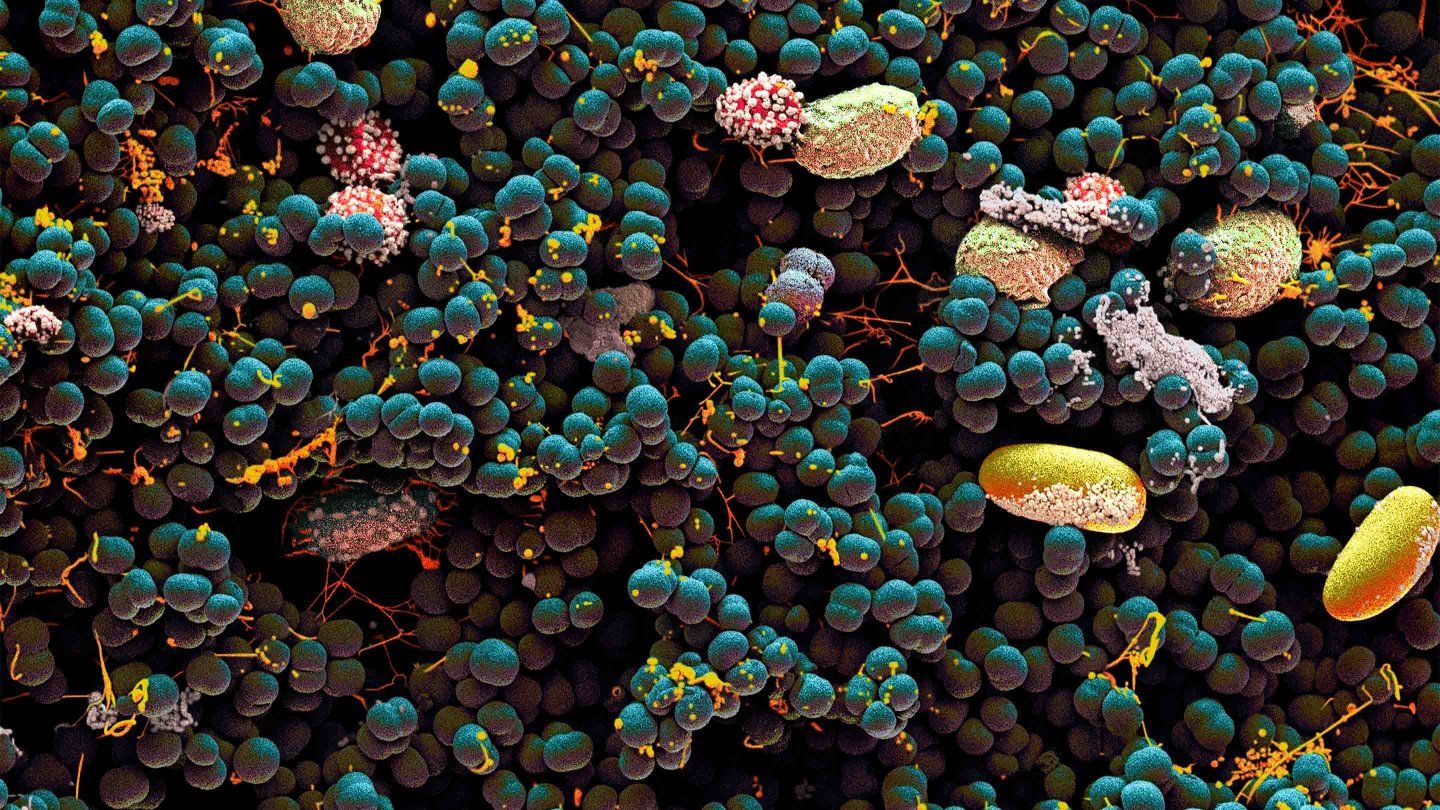
Our own bodies teem with life. Our intestines are packed with thriving invisible ecosystems. Our skin crawls with tiny critters. Our mouths are a jungle. Microbes – mostly bacteria, but also other minuscule beings such as viruses and fungi – live in our ears, noses, genitals, and lungs. They even travel in breast milk.
The field of modern microbiome science is only about 15 years old, but what we’ve learned in that time is absolutely staggering, says Susan Lynch, PhD, who directs UCSF’s Benioff Center for Microbiome Medicine. Scientists have surveyed microbial life on virtually every surface of the human body and in nearly all its nooks and crannies. They estimate that as many 1,000 species of bacteria alone may inhabit just one person. These tiny tenants are about as numerous as our human cells, and their genes may outnumber our own a hundredfold or more.
But these bugs aren’t just along for the ride. Starting at birth or even earlier, they help train our immune systems to distinguish friend from foe. They help us break down food. They even manufacture molecules that neurons in our brains use to communicate. Given the remarkable symbiosis between our bodies and their microbial communities, scientists often refer to the human-microbiome team as a “superorganism.”
Teasing apart the connections between our microbiomes and our health can be tricky, however. It’s not always clear, for example, whether changes in a sick person’s microbiome have caused their disease or whether the disease – or something else – has changed their microbiome. Further complicating matters is the fact that everyone’s microbiome is different. The makeup of your microbial zoo depends on factors particular to you, such as your diet, age, and where you live. Consequently, what makes a microbiome “healthy” or “unhealthy” most likely varies from person to person.
Still, experts are starting to piece together the puzzle. At the Benioff Center for Microbiome Medicine, more than 130 scientists are working together – like a superorganism themselves – to unlock our microbes’ secrets and turn those insights into new therapies. The following are eight areas of research that offer tantalizing evidence of how our microbiomes influence our health, and how we might one day manipulate them to prevent and treat disease.
Depression
Bacterial Blues
If you’ve ever experienced depression, you know it’s not just “all in your head.” It isn’t even all in your brain.
“Depression is truly a whole-body disease,” says Ryan Rampersaud, MD, PhD, an assistant professor of psychiatry at UCSF’s Weill Institute for Neurosciences. This common mood disorder has been linked to a range of biological and environmental factors – including, he points out, your gut bugs.
In a 2016 study, scientists found that the digestive tracts of people with depression harbored microbial ecosystems that were less diverse than those of healthy controls (think city park versus rainforest). Then the scientists transplanted stool from the depressed humans into the stomachs of rats. Subsequently, the rats exhibited “depression-like” behaviors, such as avoiding open spaces (suggesting anxiety) or losing interest in drinking sugar water (loss of pleasure) – evidence that the makeup of our microbiomes can influence our moods.
But how do our microbes talk to our brains? Studies show that gut microbes can trigger the intestines to release molecules called neurotransmitters that the brain uses for signaling, including serotonin and gamma-aminobutyric acid. Many gut microbes even make neurotransmitters themselves. Some of these molecules then seep into the bloodstream and travel to the brain, where they might affect how we think or feel. A 2019 study found that some bacterial species were less abundant in people with depression. And people whose microbiomes were more capable of making a molecule related to the neurotransmitter dopamine reported a higher quality of life.
In his own lab, Rampersaud is studying the microbiomes of people with depression before and after an eight-week course of antidepressants. He wants to identify any changes in their microbiomes as their depression lifts. For example, he may find that a certain bacteria-made molecule is lacking in depressed patients but increases as their mood improves. If that’s the case, he imagines, doctors could one day supplement depression treatments with probiotic pills containing bacteria that make the depleted molecule.
“What I hope is that we can help alleviate suffering,” Rampersaud says.
Gum Disease
Down in the Mouth
You may have a separate insurance plan for your teeth, but the health of your mouth is tightly tied to the health of the rest of your body. “The two are intertwined in so many ways,” says Yvonne Hernandez-Kapila, DDS ’90, PhD ’97, the associate dean for research at UCLA School of Dentistry and a UCSF adjunct professor of orofacial sciences.

Heart disease, for example, is unusually common in people with gum disease. So are certain cancers. Scientists are still unpacking the mechanisms behind these connections, but Hernandez-Kapila believes mouth microbes are at least partly to blame.
Consider gingivitis, she says. This inflammatory gum disease, and its worse form, periodontitis, are linked to worrisome changes in the oral microbiome: Certain unfriendly bacteria proliferate, suppressing friendly bacteria. Studies suggest that this shift elicits chronic inflammation, which can cause bone loss. Heart disease and other internal ailments might arise when bad bacteria that multiply in the mouth – along with the molecules they make – leak into the bloodstream and travel around the body, stirring up more trouble wherever they land.
In experiments in mice, Hernandez-Kapila showed that bacteria associated with gum disease can also encourage the growth of cancers in the head and mouth. These discoveries have led her to a potential new cancer therapy. By treating the mice with nisin, a molecule made by certain bacteria and that is able to kill other bacteria, she found that she could shrink the animals’ tumors.
“We can specifically target microbiomes to change the course of the disease,” Hernandez-Kapila says. In collaboration with her UCSF colleagues, she is now launching a clinical trial of nisin in patients with oral cancer. She wants to see how the molecule alters their mouth microbiomes and whether the tumor-shrinking powers observed in mice hold true for humans, too.
Eczema
Surface Tension
No matter how thoroughly you scrub yourself in the shower, your skin still bustles with microbial life. And that’s a feature, not – ahem – a bug.
The skin microbiome has many benefits, including keeping harmful bugs out. “It’s doing a lot for us, even if we can’t see it,” says Tiffany Scharschmidt, MD ’08, a UCSF associate professor of dermatology.

Scharschmidt studies the relationship between skin microbes and inflammatory skin diseases like eczema. Scientists have long known that the immune system participates in these diseases, she says. “What we’re trying to understand is how the microbiome plays a role.”
Early in our lives, Scharschmidt notes, our immune systems learn to recognize our skin’s microbial inhabitants as what she calls “part of the broader self” and to coexist with them peacefully. But what happens if this rapport turns sour? Say, for instance, the makeup of these microbes shifts later in life. Could that change nudge our immune systems toward misbehavior? Could inflammation and disease follow?
The microbial ecosystem in the gut might also contribute to immune dysregulation in the skin. In a 2022 paper, Scharschmidt’s team showed that chronic inflammation in the intestines of mice caused inflammatory molecules to migrate to the skin, prompting immune cells there to attack friendly bacteria. This immune system mischief also led to skin inflammation.
Scharschmidt hopes to learn how our immune systems communicate with our skin bacteria in times of good health as well as bad, which includes deciphering the precise immune cells and processes involved. “The overarching question,” she says, “is ‘Can we decode this language?’”
Multiple Sclerosis
Building up the Nerves
Recently, Sergio Baranzini, PhD, the Heidrich Family and Friends Professor of Neurology at UCSF’s Weill Institute for Neurosciences, led a study looking at the microbiomes of more than 500 people with one thing in common: multiple sclerosis, or MS.

In MS, a person’s immune system attacks the protective sheath around nerve cells in their brain and spinal cord. This can cause a range of symptoms, including vision problems, pain, fatigue, and loss of muscle control.
Because our gut microbes interact closely with our immune systems, Baranzini wonders whether variations in the makeup of our microbiomes could increase our risk of MS and other autoimmune conditions. It’s possible that the molecules those bacteria make could be more important than the actual species of bacteria. “Sometimes,” he says, “it doesn’t really matter who’s there, as long as a particular function is being provided.”
Baranzini’s lab and others have begun gathering compelling evidence that gut microbes play a part in MS, in addition to other known risk factors, including genetics, smoking, and infection with the Epstein-Barr virus. The new study, published in 2022 by a global consortium of labs that Baranzini leads, was the largest of its kind to date. The researchers found several types of bacteria, along with molecules made by bacteria, that were either more or less prevalent in MS patients than in healthy subjects living in the same house.
These differences might encourage inflammation, the authors wrote, and make the effects of MS worse. They hope the findings can lead to “designer probiotics” that improve the lives of MS patients.
What Makes a “Healthy” Microbiome?
The short answer is that no one really knows – at least not yet.
“We’ve learned a lot about what can go wrong with the microbiome,” says UCSF’s Peter Turnbaugh, PhD. But despite the boom in microbiome research over the past decade, today’s scientists can’t tell you precisely what to eat or buy to nurture your microbes in ways that promote health.
“I’d be skeptical of anyone who claims they know the ‘right’ diet for your microbiome,” Turnbaugh says. That’s because our microbial communities are just as unique and unpredictable as we are. “The microbiomes of healthy people vary tremendously, both between individuals and over time,” he says. So no one can define exactly what a healthy microbiome looks like for a particular person at a particular moment. And no one can say precisely how to feed your microbiome to make it act a certain way.
Even so, it appears that there may be benefits to eating dietary fiber, which is found in vegetables, fruits, whole grains, and other plant-based foods. We can’t digest fiber on our own; our gut bacteria chew it up for us. There is some evidence that the molecules these bacteria produce when they break down fiber help lower inflammation and keep blood sugar under control. But not all fiber is the same, Turnbaugh warns, and different types – as well as other components in fiber-rich foods – may interact with our microbes in ways that are less understood.
What about probiotics? A host of pills, yogurts, and lotions promise to boost our health through the power of microbes. But like other supplements, these products aren’t regulated by the Food and Drug Administration. That means there’s no guarantee that a product actually contains the bacteria it claims to, or even if it does, that those bacteria will help you. (If you want to learn what’s in a particular product and the science behind it, Turnbaugh recommends the website usprobioticguide.com.)
With everything scientists are discovering about the role our microbiomes play in our health, we all want to know how to keep these bugs functioning at their best. But microbiome medicine likely won’t lead to simple, one-size-fits-all solutions. “The reality is a lot more complicated,” Turnbaugh says. “There’s always more to learn.”
Allergies & Asthma
Bugs to Help You Breathe
We acquire our first microbes from our mothers, during birth or even in utero. Over our first years of life, our microbiomes rapidly diversify, and these germs provide our developing selves with a “library of microbes,” says Susan Lynch, which trains our immune systems to tolerate their presence.

This early microbial education, she adds, may explain why babies delivered vaginally are less likely than those born by cesarean section to acquire allergies or asthma in childhood. Without that early conditioning, the immune system can mistake a harmless substance, such as pollen or pet dander, as being dangerous. (Allergies and asthma are also less common among children who grow up on farms.)
Such associations suggest that the microbiomes we cultivate as infants affect our health later in life. But how? Lynch’s own research has begun to yield some answers. In a 2016 study, she showed that patterns in the composition of the gut microbiomes of 1-month-old babies could predict which kids were at much higher risk of acquiring allergies by age 2 and asthma by age 4. The gut microbiomes of the high-risk infants were missing a wide range of anti-inflammatory molecules, she found.
Then, in a subsequent paper, Lynch identified a molecule made by the high-risk infants’ gut bacteria that seems to be responsible for the later emergence of allergies. Her team showed that the molecule travels through the blood to the airway, where it impairs immune cell activity, leading to inflammation.
In 2016, Lynch co-founded a company called Siolta Therapeutics to turn her findings into treatments. One product now in development will deliver a cocktail of live bacteria into the guts of newborns most at risk of allergies and asthma. The hope is that these bugs will start making the asthma-protective molecules that are underproduced by the babies’ native microbiomes.
“We’re trying to build healthy microbiomes from the very earliest stages of postnatal life,” Lynch says.
Preterm Birth
Early Influencers
About one in 10 babies in the United States is born preterm – before 37 weeks of gestation. These infants are at higher risk of disability and death. But scientists have struggled to pinpoint the causes of early birth – or ways to prevent it. That’s why Marina Sirota, PhD, a UCSF associate professor of pediatrics, is excited to have found hints to answers in the vaginal microbiome.

In a 2020 study, Sirota measured the variety of bacterial species in the vaginal microbiomes of pregnant women. In general, she says, “we think of microbial diversity as a positive.” The more diverse your gut microbiome, for instance, the more likely you are to have good blood pressure, bowel function, and other markers of health. In the vaginal microbiome, however, “diversity is actually not a good thing,” Sirota points out.
Her study showed that pregnant women with a greater diversity of vaginal microbes were more likely to deliver their babies prematurely. This correlation was strongest in microbial measurements taken during the first trimester. Sirota also found several types of bacteria that were either more or less abundant in mothers who went on to deliver preterm.
These differences, she warns, are merely associations. Sirota’s data can’t tell her whether a mother’s microbiome actually causes early birth. It’s possible that other factors in a pregnant woman’s environment, such as her diet or chemical exposures, might alter her microbiome and induce an early delivery.
Regardless, Sirota is using computer science and large microbiome data sets to identify the mothers and babies in the greatest danger. “The goal is to figure out whether we can apply machine learning and predict women who are at a higher risk of preterm birth,” she says.
Diet
Heavy Questions
You may be a vegetarian, a sushi aficionado, or someone with an unbreakable diet soda habit. Your microbes have preferences, too. In the lab of Peter Turnbaugh, PhD, a UCSF professor of microbiology and immunology, researchers are studying the relationship between diet, weight, and what our gut bacteria like to munch on. “We’re interested in how the things that we eat affect our microbes, and in turn, how the microbes affect what we eat,” he says.

For example, his team found that after just five days on a diet of meat, eggs, and cheese, people’s microbiomes looked significantly different than after five days on a plant-based diet. And the microbes that flourished on the plant-based diet produced more of a certain molecule that fights inflammation. In other research, Turnbaugh showed that raw and cooked potatoes also have differing effects on our microbial ecosystems.
Such changes to our microbiomes might influence our ability to gain or lose weight. As a graduate student, Turnbaugh led a study showing that when gut microbes from obese mice were transplanted into skinny mice, the skinny mice gained weight. More recently, in a 2021 study, his team showed that the opposite is also true: First, human volunteers consumed an extremely low-calorie, liquid diet that made them lose weight. Then the researchers placed stool from those subjects into the guts of germ-free mice. Although they were allowed to eat whatever they wanted, the mice shed weight, just as the humans had.
Turnbaugh is also exploring how our microbiomes interact with the medicines we swallow. He recently found, for instance, that certain gut bugs can break down a common cancer drug. “Microbes are fantastic chemists,” Turnbaugh says. “They are essentially stealing the drug before it reaches the cancer.”
Cancer
Taming Tumors
Cancer, in which our bodies’ own cells change and grow out of control, might seem totally separate from the world of microbes. But in reality, “the microbiome is crucial to understanding how cancers start and progress,” says genitourinary oncologist Rohit Bose, MD, PhD, an assistant professor at UCSF’s Helen Diller Family Comprehensive Cancer Center.
Bose is investigating the connections between the microbiome and prostate tumors. Do some bacterial species cause tumors to grow faster or slower? Do microbes produce molecules that make a tumor more or less sensitive to treatment?
“There’s already experimental evidence that the microbiome changes how prostate cancers respond to therapies,” he says. Previous research has shown, for instance, that gut bacteria can make compounds similar to our own hormones, and those compounds can make prostate cancer harder to treat. Now, in collaboration with Susan Lynch’s lab, Bose’s lab is testing in mice how gut microbes, and the molecules they make, affect prostate tumor growth.
He’s also curious about bacteria that hide in patients’ urinary tracts and around the prostate itself. These microbes interact with their environment and crank out various molecules that may affect inflammation and the immune system, just as gut microbes do. “So it makes sense that they, too, would affect the initiation and the development of cancer,” Bose says.
“We’re just at the beginning,” he adds. He also believes that what he and others discover will have implications beyond the prostate. “We think it will be widely applicable to how other kinds of cancers evolve,” observes Bose.