On March 18, 2020, feeling useless and fearing that I might fall ill from the coronavirus, I decided to start tweeting.
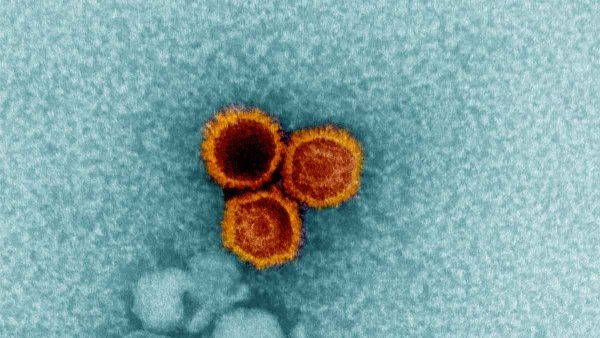
By mid-March, we’d already seen massive outbreaks of COVID-19 in China and Italy. Cases were emerging in the U.S., too, many in a nursing home outside Seattle. And in early March, the Grand Princess cruise ship, with more than 100 passengers and crew stricken by the SARS-CoV-2 virus, had sailed under the Golden Gate Bridge; I could see it from my window at UCSF’s Parnassus campus. Taken together, these incidents made it seem inevitable that San Francisco – the second densest city in the U.S., and one that relies on tourists – would get hit by the full force of the pandemic. As a 62-year-old man, it was clear that I was in a high-risk category. My mind did what anxious minds do: spool out a series of worst-case scenarios. Is my will up to date? Does my wife know my passwords?
My feeling of uselessness was a bit more surprising. I’m chair of one of the top academic departments in the nation, with 800 faculty; a yearly budget of $600 million; and world-renowned clinical, research, and educational programs. My life consists of making decisions, some of them important ones. Yet UCSF’s response to COVID-19 amounted to a health care version of martial law, with all key planning decisions made by a small incident-command task force. This was crucial – there was no time for committees and fiefdoms – but it left me without a lot of decisions to make. I found myself spending about 12 hours a day on Zoom updates, drinking in a fire hose of information about disease curves, transmission rates, the ins and outs of PPE, the ethics of rationing ventilators, and more. But there wasn’t much I could do with the information.
And so, on the night of March 18, I got on Twitter and wrote a thread describing some of the key issues we were facing. I had a sense that people – both laypeople and medical professionals – were hungry for information, and that without it the vacuum would be filled with rumor, fiction, and existential dread. And I wanted to do something useful with all the new information I was taking in. I talked about PPE; testing; our workforce; and our new dedicated COVID units in the hospital, the emergency department, and the clinic. I also shared some of our data regarding our early experience with COVID, including case rates, hospitalizations, and fatalities, taking advantage of UCSF’s long tradition of transparency.
That first tweet generated a lot of interest, so I decided to do more. The next day, I posted a series of ground rules. Interest grew, and before long, I was spending a couple of hours each day on my tweets, pulling in compelling articles, conversations with experts, anything that seemed interesting and important. My readership grew. I had been on Twitter since 2011 and had generated a healthy following of about 20,000. Now, my followers grew by about 5,000 each week. I noticed that some experts were tweeting in their particular niches, be it epidemiology, or testing, or policy. I decided that my tweets would take advantage of my broad interests as a generalist and my position as a leader, talking about COVID-related issues as they applied to clinical medicine, policy, ethics, technology, and epidemiology, while layering in what I was learning from my front row seat to the inner workings of a world-class academic medical center. I’d also offer a special focus on the situation in San Francisco and California.
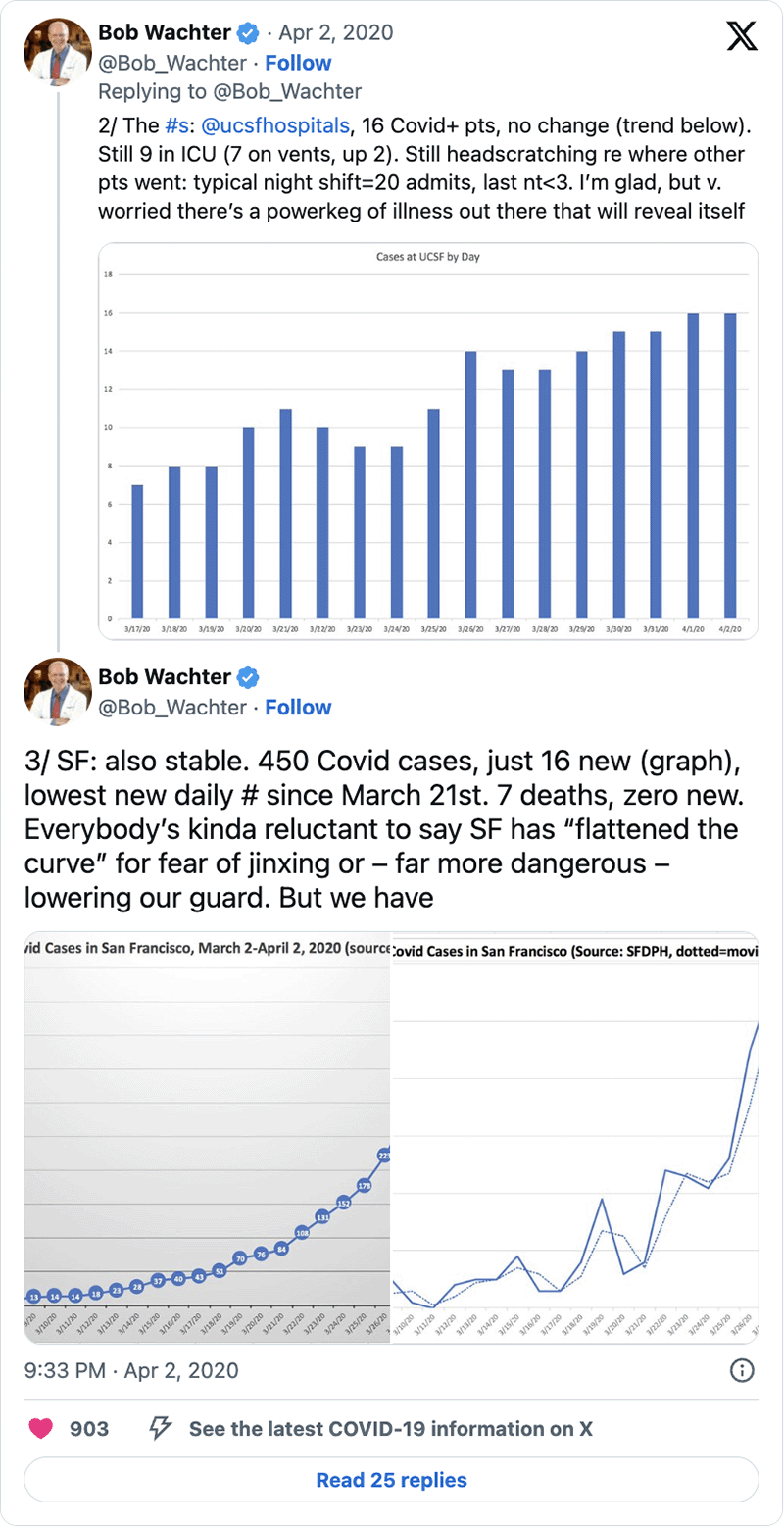
Each day, I began my tweets with a local update. My model was that of a war correspondent embedded in an army unit, my tweets serving as a kind of “news from the front.” While I thought I’d be chronicling a tsunami, as the days passed it became clear that, due to strong and early actions by political and corporate leaders and impressive cooperation from citizens, San Francisco and the Bay Area had, in fact, “flattened the curve.” The “San Francisco story” went national, and many people and media outlets looked to me and my tweets as a source for that narrative.
At the time I launched my tweets, I also decided to repurpose another forum to disseminate information: our Medical Grand Rounds. Until mid-March, these rounds were a relatively sleepy and traditional forum in which experts presented updates on the latest clinical findings or research advances. The audience might have hit 100 for a particularly newsworthy topic or speaker.
We quickly converted them into COVID Grand Rounds, highlighting the most interesting topic each week: the disease curve, new treatments, insights into the workings of the virus, our evolving understanding of testing, COVID and health disparities, and more. Our live Zoom audiences for Grand Rounds often topped 2,500, and our first 10 conferences were viewed on YouTube more than 250,000 times.
It’s remarkable to consider that all of these methods of communicating – Twitter, Zoom, and YouTube – did not exist 15 years ago. Their popularity, and the fact that they are now seen as go-to sites for up-to-date and trusted information about COVID, creates an extraordinary opportunity to communicate with professional and lay audiences around the world. Of course, they also create opportunities to spread misinformation. The Wall Street Journal profiled me in mid-May, and the title of the article – “Doctors are Tweeting About Coronavirus to Make Facts Go Viral” – cleverly made this point.
I decided early on that part of my goal was to be authentic, which meant that if real life intruded into or influenced my work or worldview, I’d post that (hopefully without being silly or too self-indulgent). And if I came upon something humorous and it helped me get through my day, I’d post that, too. So people got to see my dog, Newman, and his terrible pandemic haircut. They got to follow the eating competition between two dogs, Mabel and Olive, breathlessly announced by BBC sportscaster Andrew Cotter. Most infamously, on April 1, they got to see my lunch of SpaghettiOs and Double Stuf Oreos.
And they got to see the poignancy of the pandemic, too, such as when I posted my interviews with UCSF physicians who had volunteered to care for patients in the hardest-hit areas of the country: Queens, New York; and the Navajo Nation. Or the story of the Kansas farmer who selflessly donated his mask to the state of New York.
Perhaps most interesting and gratifying was feeling the appreciation of the public as I did my best to explain the science and the medicine of COVID. There’s never been a time that I can recall in which everyone wanted – needed – to know things that physicians and scientists spend years learning: how viruses spread, how to interpret test results, how clinical trials are designed, and what abbreviations ranging from PCR to PPE mean. While scientists had the advantage of knowing a lot of foundational information and concepts, COVID-19 was a great leveler: on January 1, 2020, no one knew anything about this particular virus.
And so we have all learned about it together.
Robert Wachter is chair of the UCSF Department of Medicine, the Lynne and Marc Benioff Professor of Hospital Medicine, and the Holly Smith Distinguished Professor of Science and Medicine.