Five Big Lessons from the Pandemic
When future historians look back on this moment, they will draw many conclusions from our response to this crisis. Here are five big lessons that UCSF experts already see taking shape.

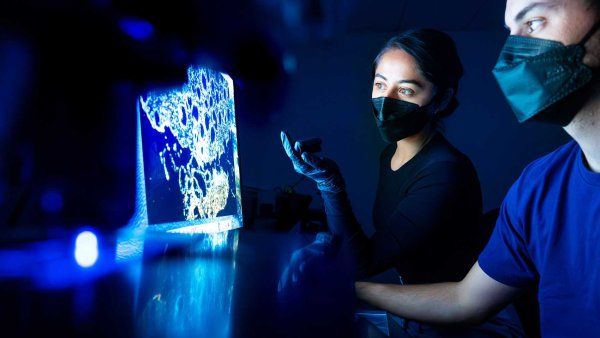
1. Science doesn’t always move slowly
“It’s been fantastic to see how fast science can move when people collaborate. We’ve been breaking down silos between scientists, laboratories, and institutions worldwide, as well as between universities and pharmaceutical companies. Structural biologists are talking to virologists who are talking to clinicians. It is the way we should do all science in the future. It’s not just connections between, for example, work on genes and work on proteins; it’s about building connections between people.”
Nevan Krogan, PhD
Professor of cellular and molecular pharmacology; director, UCSF Quantitative Biosciences Institute
2. We are failing the most vulnerable
“This pandemic exposed deep, preexisting inequities. Although COVID-19 can affect everyone, the impact of this epidemic is not felt equally, and managing the pandemic will require us to focus on the most marginalized among us. We’ve learned that we have to pay attention not just to the conditions that lead to increased transmission but also to the things that make it hard for people to isolate, to quarantine, to get tested.”
Kirsten Bibbins-Domingo, PhD ’94, MD ’99, MAS ’04
Lee Goldman, MD, Professor of Medicine; chair, Department of Epidemiology and Biostatistics
3. Supply chains are a weak link
“We’ve learned that the supply chain is an extraordinarily complex organism. And it is fragile in the sense that, if you take out a few key sources, it’s difficult to ramp up as quickly as we’ve needed to. The vast majority of supplies we needed – PPE and swabs – came from the two countries that were the most devastated early on, Italy and China, and U.S.-based suppliers didn’t have the capability to scale up quickly.”
Joshua Adler, MD
Chief medical officer and executive vice president for physician services, UCSF Health
4. Video visits are here to stay
“Before the pandemic, about 2% of our visits were conducted as video visits. Currently, we’re at about 60%, with some clinics at 90% to 100%. We’d been working on increasing those numbers for several years, and there had been a lot of resistance. And then all of a sudden, we changed. We’ve learned that we can conduct a fairly complete evaluation, including – more so than you would guess – parts of the physical exam. There’s no question in the early data that patients really appreciate this, particularly patients who come from quite a distance to be seen.”
Susan Smith, MD
Chief faculty practices officer and senior vice president, UCSF Health
5. Delayed consequences enable bad behavior
“Today, we know a lot about the virus, including how it spreads and how to prevent it. Today’s risks are mostly about behavior, particularly masking and social distancing. And the surges we have seen have predictably occurred in places with the most at-risk behavior. A friend recently said to me, ‘The virus is a great teacher.’ No, not really. Fire is a great teacher: Touch it and it hurts like hell. For SARS-CoV-2, a person or a state can act badly and do fine for a while, confirming their belief that precautions are for wimps. By the time they feel the fire, it’s too late.”
Robert Wachter, MD
Lynne and Marc Benioff Professor of Hospital Medicine; Holly Smith Distinguished Professor of Science and Medicine; chair, Department of Medicine