New Fellowship Represents a Paradigm Shift in Global Health
Leaving lasting systems and educating local providers is the goal of this first-of-its-kind fellowship.

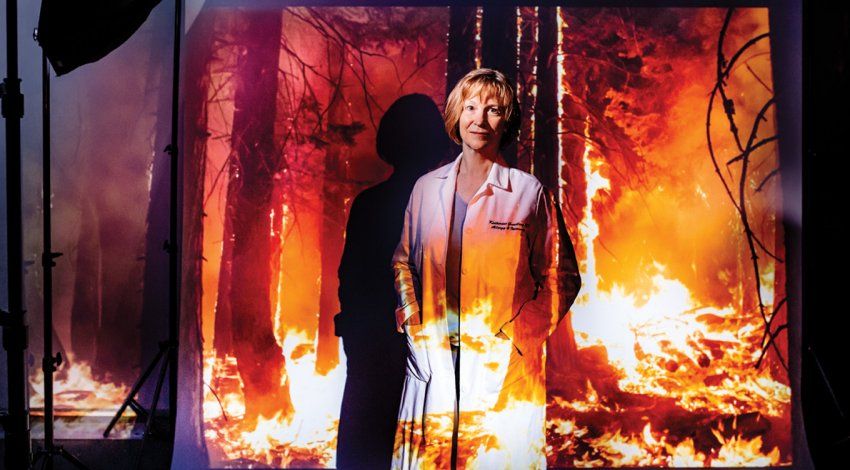
Global Health-Hospital Medicine Fellow Palav Babaria (at center, in scrubs) worked closely with colleagues at a Haitian hospital to develop lasting health care solutions.
Palav Babaria, MD, was working her first shift in a rural Haitian hospital when she was informed of a man in the ICU with end-stage kidney failure. In-country for only 12 hours, Palav learned the hard way that there was no formal referral process to hospitals in Port-au-Prince, three hours away. There were no Haitian doctors available right then, and the local ambulance was on another call. “We finally got an ambulance from another town. I scribbled down some notes and sent him on his way,” recalls Babaria, a UC San Francisco Global Health-Hospital Medicine Fellow. “I have no idea whether he even made it.”
Several months later, Babaria had to refer an HIV-positive woman to another hospital. This time, her colleague Pierre Jacquelin Auguste, MD, a physician trained in Haiti, called up a friend at a hospital with many HIV specialists. He explained the case, made sure the patient had a bed, and arranged transport. “Everything happened at the snap of his fingers because he knew the local resources,” says Babaria. “In global health, there is just no substitute for local knowledge.”
Everything happened at the snap of his fingers because he knew what the local resources were. In global health, there is just no substitute for local knowledge.”
The experiential wisdom garnered from working in the developing world is critical for physicians like Babaria, who intends to devote her career to enhancing care in resource-poor areas. “In a setting where there are few formal processes in place, the ties between local professionals are lifesaving,” she says. “Partnering with in-country colleagues to develop systems out of their informal relationships is a great solution going forward.”
Leaving systems in place, as well as educating local providers to carry them out, represents both the goal of the Global Health-Hospital Medicine Fellowship (GHHMF) – the first fellowship of its kind in the world –
and a paradigm shift in global health. “Over the years, global health and tropical disease eradication movements have had some great successes, including the smallpox vaccination program and the headway we’ve made with HIV,” says Sriram Shamasunder, MD, who co-founded the GHHMF with Phuoc Le, MD, MPH. “But they left little infrastructure.”
GHHMF fellows, by contrast, work in public hospitals and are actively engaged with the ministries of health and nongovernmental organizations in their host countries of Haiti, Liberia, and India. “Our fellows work with the public sector on long-term quality improvement projects driven by local people and organizations,” says Shamasunder.
The fellowship also seeks to train the next generation of global health leaders. As the burden of chronic disease continues to rise worldwide, those leaders must bring hospital-based tools to the field to manage the complexity of care. Babaria estimates that nearly half her patients suffer from chronic diseases, with heart failure being the most common diagnosis. “Ideally we would like to see our patients with heart failure, hypertension, or diabetes once a month to track their progress,” she says. But asking patients to make frequent treks to the hospital poses too big a burden. Typically, a patient would have to walk for hours to reach a main road, then spend a month’s salary to hire a motorcycle for the last leg of the trip. Only the sickest made the journey. “I knew if my patient was a mother that there were children home, unattended,” says Babaria. “And if my patient was a father, no one was earning a wage that day.”
By the year’s end, Babaria and her in-country colleagues had developed a chronic hypertension clinic – run by Auguste – to address the enormous toll of chronic disease.
Shamasunder hopes the fellowship will be a new prototype for global health. “We want to create a longitudinal model, where we mentor the local population, learn from them, and create reliable and predictable protocols that improve the lives of the poorest,” he says.