Nurses – theirs are the first faces we see on our way into the world, and are likely to be the last faces we see on the way out. For every sudden illness or injury in between, nurses are the ones who conjure up calm from the chaos of an emergency room. They are the ones who divine the origin of our pain or fear so that healing can begin. We sought out faculty and graduates of UCSF’s School of Nursing in the thick of a typical day and asked them if they could pick another nurse from a crowd of strangers. They universally answered yes: Nurses would be the ones deep in conversation – the most reflective and engaged people in the room. These are qualities that have defined nurses since the profession began. Here’s how they look on the modern nurse, whether he or she is in the delivery room or in a hospice, analyzing genetic data or writing code for an app.

Community
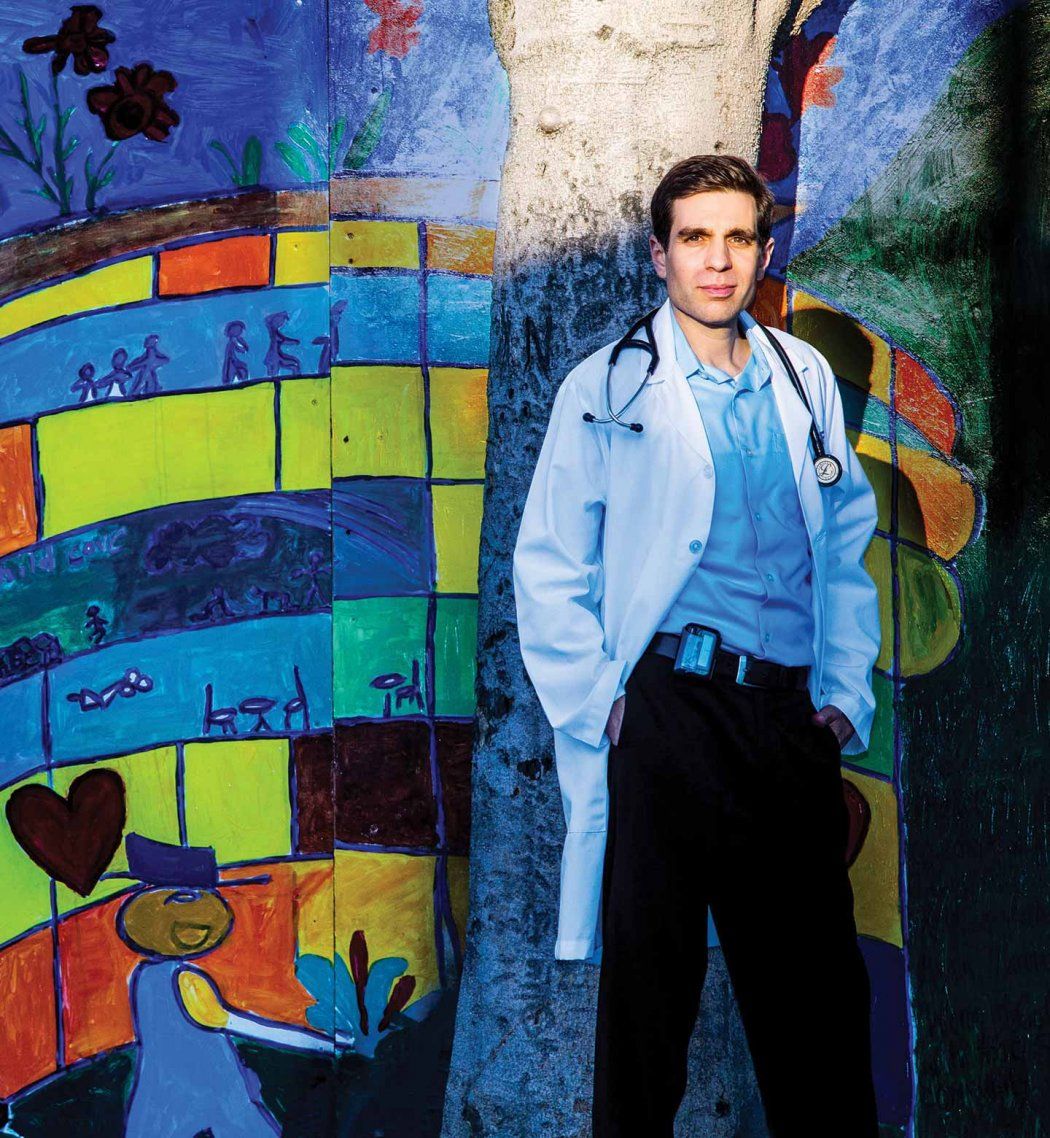
I was diagnosed as being HIV-positive in 2004 and took on all that condition’s stigma and shame. I got acutely ill very fast and lost weight visibly, but I still kept it from my family. They had invested so much love and care in me, and I felt I had ruined it all. Then I got cancer. The medical staff would shoo my parents out of my hospital room when they had to discuss HIV, until one day when they sent in a nurse named Laurie to talk to me. She had noticed how loving and concerned my parents were. She said, “I have a gay son, and if he had HIV, I would be upset at first, but then I would want to love and support him through it.” She gave me a bracelet that she said held all the love and support of the team. I put the bracelet on to finally tell my parents. She showed me how really listening to somebody, being present without judgment, even for just an hour, can change someone’s life. Laurie set the bar. Now I’m a nurse practitioner working with HIV-positive youth and HIV-negative youth at high risk for HIV. I’ve been a part of two ad campaigns to erase the stigma of AIDS. Though some of my patients have seen my picture on buses and billboards, I usually don’t tell them I have HIV because my work is about their experience, not mine. But the virus is always in the room with me; it gives me a deeper understanding of what my patients are going through. It’s hard not to love somebody when you hear their story and what they walk with. It’s an incredible gift and window into humanity.
Jonathan Van Nuys, RN, MS ’13, NP

JoAnne Saxe center, standing)
Interprofessional Education
I’m a faculty clinician with the VA Centers of Excellence in Primary Care at the San Francisco VA Medical Center, working with Patient Aligned Care Teams, where nurse practitioner students and medical residents train together in a primary care clinic. An important feature of team-based care is the daily “huddle” [above]. The huddle provides the team with an opportunity to collectively support every patient who will be seen one-on-one later that day [left]. It’s given me an appreciation for the overlap between the professions. Some physician colleagues whom I have mentored have such giving and sharing hearts that they’ve mastered what is traditionally thought of as nursing care. And I’ve seen nurses who are phenomenal diagnosticians. I think the more we play in the same sandbox – and multiprofessional teams are the direction we are headed in – the more we’re going to find out what each of us brings to the team as a person who has life experiences and talents and a particular professional expertise.
JoAnne Saxe, RN, MS ’82, DNP

Midwifery
My job at SFGH could never be routine – it’s not about woman after woman pushing a baby out. Each woman is different; she brings her whole life story into the room. Childbirth can be joyful, like it was for Yulishea [pictured holding her baby], or complicated. A mother may be giving the baby up for adoption or may feel ambivalent about having a child, or there may be a fetal loss. It’s still her experience. We try to help people be in the moment to have their baby in the best way possible for them. I am continually in awe of the strength women draw upon to get themselves through such an intense life transition.
Margaret Hutchison, CNM, MSN

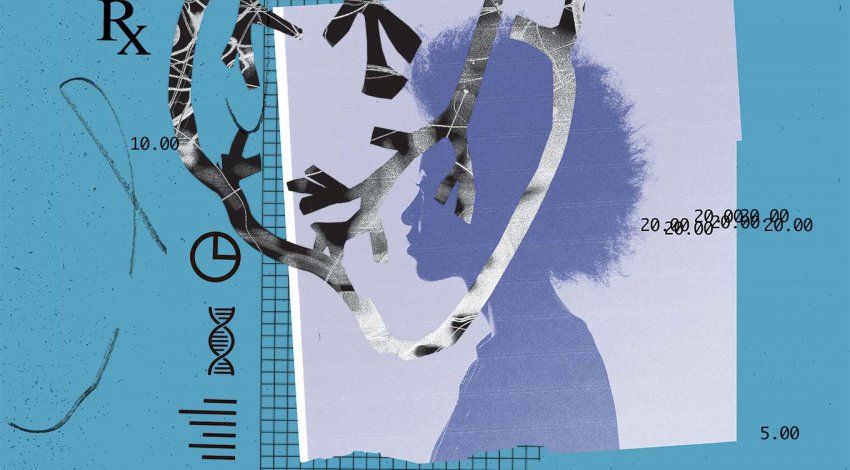
Laboratory
I think most people who study symptom management in patients with cancer are envious of what we have at UCSF. I tell my graduate students that they have to sit in the room with our group to believe it. There are usually 10 of us – physicians, statisticians, a bioinformaticist, a psychologist, nurses, and Brad Aouizerat, PhD [left], a molecular geneticist. We all look at the same data, tracking pain scores up and down. But we explore those relationships in a far richer context because we have different lenses that we look through. Without Brad, I couldn’t be drilling down to the genetic causes behind the pain, and without me, Brad couldn’t sort out the symptom data and relate it to the treatment the patient received. It’s a dream team.
Christine Miaskowski, RN, PhD, postdoctoral alumna

Digital Innovation
I remember the moment that completely changed my research career: I opened a letter from the wife of one of my clinical trial patients, telling me that her 35-year-old husband had had another heart attack and died, leaving two small children behind. I decided right then that if I wanted to save lives, I had to start with prevention. Now I develop apps at UCSF to prevent diabetes and cardiovascular disease. As a former critical care nurse, I know patients need simplicity when dealing with difficult health issues. My challenge is to effectively apply ever-evolving digital technologies to patients’ lifestyle changes. Our patients have had great success – they tell us so with great pride.
Yoshimi Fukuoka, RN, PhD ’03
UCSF Nursing Students

Sam Lee, RN, MA: Former public affairs officer, 4th Combat Camera Squadron, U.S. Air Force
Goal: Family nurse practitioner

Margeaux Marquis, RN: Former emergency department technician at St. Joseph Hospital of Orange
Goal: Clinical nurse specialist in critical care/trauma medicine

Brianna Singleton, MPH, RN: Former student, University of San Francisco School of Public Health
Goal: Adult-geriatrics nurse practitioner, with a specialty in occupational and environmental health

Diana Teng, RN: Former teaching assistant, Cañada College’s Human Anatomy Lab and Skyline College’s EMT Skills Lab
Goal: Adult-geriatrics nurse practitioner, with a specialty in occupational and environmental health

David Vlahov (center)
Dean, UCSF School of Nursing
My older brother developed mumps encephalitis at age 18 months; he was severely brain damaged, and my parents had to institutionalize him when he got too big for them to handle. There, they trained him to shave and take care of himself through operant conditioning, giving him a cup of coffee for each task he completed. My dad and I visited him every Sunday. Once, when he was about 16, we took him to McDonald’s. He saw the coffee pot across the counter and just started climbing over. People grabbed their kids and ran. My dad and I were saying, “Don’t worry, he just likes coffee.” Nursing is how you care not only for my brother, but also for the family, given all the stigma and shame. It’s a profession that goes beyond the patient in front of you to the family and population context. I brought that same perspective to Baltimore, when I founded and led for 20 years an ongoing HIV study of injection drug users that led to the city’s first needle exchange. And I brought that perspective to our investigation of the wide reach of post-traumatic stress disorder after 9/11. Now, as dean, I am giving back to the profession by educating extraordinarily smart nurses who have a fire inside to advance nursing – at the bedside, in the clinic, and at the policy level.
David Vlahov, RN, PhD

DorAnne Donesky (right)
Palliative Care
I work with UCSF patients with severe pulmonary disease who are chronically short of breath. I give them tools to manage the fear and panic that can set in when a breath doesn’t come. I walk side by side with them so they can enjoy and optimize their lives. It’s a very intimate specialty, one nurses were doing long before it was called palliative care. I have two patients I’ve known for years as part of a multisite Internet-based study. One is local, the other from Arizona. These people have phenomenal self-management techniques. . . . Any other patients would have died within six months. We recently went out to lunch so the two could meet for the first time. Sitting at a table with them – talk about chills down your spine. It was just beautiful.
DorAnne Donesky, RN, PhD ’03