When UCSF Magazine asked me to moderate a panel discussion about race in medicine, I reflected on how far our field has come. Physicians didn’t talk much about this topic when I was in medical school.
Thankfully, that’s no longer the case. Race is now at the forefront of conversations at academic health centers across the country. Faculty members, staff, and students alike are wrestling with difficult questions about the role that racial categories play in biomedical science and the delivery of care. Is our knowledge about human illness and how to treat it based on biased studies or assumptions? Should race factor into our clinical decisions and the tools we use to guide our care? How can we ensure that the disparities exposed by the COVID-19 pandemic, which has disproportionately harmed and killed people of color, do not continue?
The following discussion (which has been edited for length and clarity) offers a window into this complex – and sometimes contentious – debate. I learned a lot, and I hope that you will too.
Panelists

Moderator
Megha Garg, MD, MPH, is an assistant professor and course director for the curriculum covering social justice and racism at the UCSF School of Medicine. She is also the associate chief of hospital medicine at the San Francisco VA Medical Center.

Jennifer James, PhD ’16, MSW, MSSP, is a medical sociologist and bioethicist at the UCSF Institute for Health and Aging in the UCSF School of Nursing and an assistant professor of social and behavioral sciences. She studies the relationship between patients and health care providers and how people make decisions about their care.

Phuoc Le, MD, MPH, is an associate professor of medicine and pediatrics. He co-founded the Health, Equity, Action, and Leadership (HEAL) initiative, a fellowship program that trains health professionals to serve low-resource communities around the world.

Akinyemi Oni-Orisan, PharmD, PhD, is a geneticist at the UCSF Institute for Human Genetics and an assistant professor of clinical pharmacy. His research illuminates how genetic variation affects medication response in diverse populations.

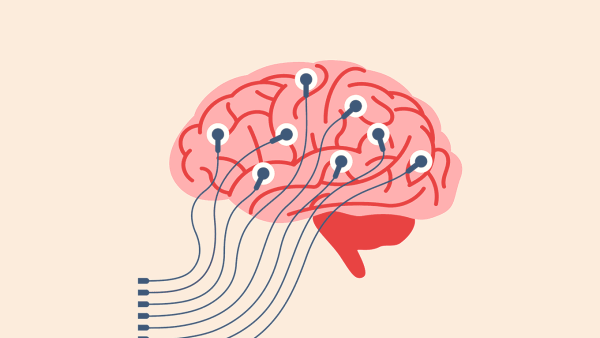
Katherine Possin, PhD, is a neuropsychologist and associate professor of neurology at the UCSF Weill Institute for Neurosciences. She focuses on Alzheimer’s disease and related disorders and holds the John Douglas French Alzheimer’s Foundation Professorship.

Neil Powe, MD, MPH, MBA, is a clinical epidemiologist and outcomes researcher, the Constance B. Wofsy Distinguished Professor, and chief of the Department of Medicine at Zuckerberg San Francisco General Hospital. He also co-chairs a joint task force of the National Kidney Foundation and the American Society of Nephrology assessing the use of race in diagnosing kidney disease.
Should Doctors Ignore Race?
Megha Garg: Do you believe that racial categories should be used in clinical practice and research?
Jennifer James: This question, to me, feels overly simplistic. There’s a straw-man idea out there that the word “race” should never be uttered within 50 feet of a hospital, but I know of very few people who actually think that.
However, I do think that the way we’re using race now is essentialist: We often assume that differences in disease incidence or outcomes between racial groups boil down to inherent biological differences, which is scientifically untrue –and often harms people of color. Historically, medicine and science have advanced racism and systemic oppression through the identification of these supposed biological “differences.” And the legacies of this are still seen in our clinical care.
Phuoc Le: When I was in medical school in the early 2000s, we were taught to put race in the one‑liner.1 We couldn’t just say the patient was a 55-year-old person coming in with chest pain. We were taught to put “55-year-old African American male.” The way I train medical students now, and the way I think about race in my own practice, is I ask myself: “What is the purpose of using race?” When you put race in the one-liner, all you’re doing is – excuse me for the pun – coloring somebody else’s thoughts about the patient. You’re perpetuating implicit bias. In that case, let’s not use race.
At the same time, I absolutely do not believe in a “color-blind” approach to medicine. In law, decades of so-called color-blind policies have clearly failed to achieve racial equity. It’s the same in medicine: If we simply ignore race, we will fail to call out inequities in our health care system.
Garg: I, too, learned to write the patient’s race in the one-liner. And that was some years after you, Dr. Le. So things are slow-changing in medicine.
Neil Powe: In a perfect world, we would not use race. But we don’t have a perfect world. Therefore, we have used race as a proxy, or what clinical researchers sometimes call a surrogate marker, for biologic and social factors that we may not completely understand or have good data for. It’s not unusual that we use surrogates in research and medicine. Cholesterol is a surrogate marker for heart disease. Education or occupation is a surrogate for socioeconomic status.
Katherine Possin: When it comes to brain health, neuropsychologists like myself consider race or ethnicity to be a crude proxy for lifelong social experience. If you look at the history of cognitive testing, for example, what we’ve seen is that it’s the most socially disadvantaged groups2 that get the lowest scores. These disparities are not inherent. They are caused by inequalities – in income, education, stress, etc. – that can advantage some groups over others, starting in early childhood. So what we need to do is unpack that social experience and measure it systematically so that we can understand the true factors that predict somebody’s baseline cognitive function.
Akinyemi Oni-Orisan: I agree that there is a strong social component to race, but there is also a genetic component. And genetic variants have biological consequences. So, in addition to social factors, our research studies need to account for as much genetic variation as possible. One way we do this is making sure our studies include participants from diverse genetic ancestries, and we often use race to approximate ancestry.
Powe: I’m sure that Dr. Oni-Orisan knows the work that [UCSF professor] Neil Risch has done with the GERA3 study, where researchers asked people for their self-identified race and then determined their ancestry through genetic testing. And they found there is a good correlation between race and genetic ancestry. Somebody recently gave me a 23andMe kit. When I got my results back, I knew what they were going to show, and that’s what they showed. I didn’t need to pay somebody to tell me that.
Oni-Orisan: Right. I think many geneticists ultimately want to replace race with genetic ancestry, which is a more precise estimation of genetic variation, plus the social determinants that Dr. Possin described. But we’re not yet at a point where ancestry data are readily available. The solution for that is simply more research, particularly in underrepresented populations, which for now requires taking race into account.
Can Using Race Solve Inequities?
Garg: What counts as a “good” use of race versus a “bad” one?
Oni-Orisan: When I go to my favorite barbershop in Oakland, I know people are there not just to get their hair cut. I know there’s going to be a long line, but no one is in a hurry. I know I’m going to be entertained with animated conversation. This is how Black barbershops are.
Recently, clinicians and researchers at UCSF have taken advantage of this cultural aspect of Black-owned barbershops to provide health counseling and care to Black men with hypertension. The evidence shows that this intervention greatly improves outcomes for these men. This is an example of how race can be used – not to stereotype, but to provide more effective care – because a one-size-fits-all approach is often not the best way to care for a patient.
Le: For me, as a pediatrician working at UCSF Benioff Children’s Hospital San Francisco, I often see diseases that predominantly impact the privileged class. Cystic fibrosis is a classic example. One out of about every 3,000 white children is afflicted by this awful disease. Meanwhile, 1 out of every 300 Black children is afflicted with sickle cell disease. That’s a 10 times greater rate than for cystic fibrosis.
And yet the National Institutes of Health provides three times as much funding for the disease that afflicts mostly white children. Similarly, the amount of philanthropic dollars raised for cystic fibrosis is an order of magnitude more than for sickle cell disease, even though the amount of suffering is disproportionate in the opposite direction. This is where I think race can be used to identify and address inequity.
Should Doctors Ignore Race?
Megha Garg: Do you believe that racial categories should be used in clinical practice and research?
Jennifer James: This question, to me, feels overly simplistic. There’s a straw-man idea out there that the word “race” should never be uttered within 50 feet of a hospital, but I know of very few people who actually think that.
However, I do think that the way we’re using race now is essentialist: We often assume that differences in disease incidence or outcomes between racial groups boil down to inherent biological differences, which is scientifically untrue –and often harms people of color. Historically, medicine and science have advanced racism and systemic oppression through the identification of these supposed biological “differences.” And the legacies of this are still seen in our clinical care.
Phuoc Le: When I was in medical school in the early 2000s, we were taught to put race in the one‑liner.1 We couldn’t just say the patient was a 55-year-old person coming in with chest pain. We were taught to put “55-year-old African American male.” The way I train medical students now, and the way I think about race in my own practice, is I ask myself: “What is the purpose of using race?” When you put race in the one-liner, all you’re doing is – excuse me for the pun – coloring somebody else’s thoughts about the patient. You’re perpetuating implicit bias. In that case, let’s not use race.
1 One-liner: the summary of a patient and their illness in their medical chart
At the same time, I absolutely do not believe in a “color-blind” approach to medicine. In law, decades of so-called color-blind policies have clearly failed to achieve racial equity. It’s the same in medicine: If we simply ignore race, we will fail to call out inequities in our health care system.
Garg: I, too, learned to write the patient’s race in the one-liner. And that was some years after you, Dr. Le. So things are slow-changing in medicine.
Neil Powe: In a perfect world, we would not use race. But we don’t have a perfect world. Therefore, we have used race as a proxy, or what clinical researchers sometimes call a surrogate marker, for biologic and social factors that we may not completely understand or have good data for. It’s not unusual that we use surrogates in research and medicine. Cholesterol is a surrogate marker for heart disease. Education or occupation is a surrogate for socioeconomic status.
Katherine Possin: When it comes to brain health, neuropsychologists like myself consider race or ethnicity to be a crude proxy for lifelong social experience. If you look at the history of cognitive testing, for example, what we’ve seen is that it’s the most socially disadvantaged groups2 that get the lowest scores. These disparities are not inherent. They are caused by inequalities – in income, education, stress, etc. – that can advantage some groups over others, starting in early childhood. So what we need to do is unpack that social experience and measure it systematically so that we can understand the true factors that predict somebody’s baseline cognitive function.
2 Socially disadvantaged groups: A century ago, such groups included Eastern Europeans and Italians; today, they include Blacks and other people of color.
Akinyemi Oni-Orisan: I agree that there is a strong social component to race, but there is also a genetic component. And genetic variants have biological consequences. So, in addition to social factors, our research studies need to account for as much genetic variation as possible. One way we do this is making sure our studies include participants from diverse genetic ancestries, and we often use race to approximate ancestry.
Powe: I’m sure that Dr. Oni-Orisan knows the work that [UCSF professor] Neil Risch has done with the GERA3 study, where researchers asked people for their self-identified race and then determined their ancestry through genetic testing. And they found there is a good correlation between race and genetic ancestry. Somebody recently gave me a 23andMe kit. When I got my results back, I knew what they were going to show, and that’s what they showed. I didn’t need to pay somebody to tell me that.
3 GERA: Genetic Epidemiology Research on Adult Health and Aging
Oni-Orisan: Right. I think many geneticists ultimately want to replace race with genetic ancestry, which is a more precise estimation of genetic variation, plus the social determinants that Dr. Possin described. But we’re not yet at a point where ancestry data are readily available. The solution for that is simply more research, particularly in underrepresented populations, which for now requires taking race into account.
Can Using Race Solve Inequities?
Garg: What counts as a “good” use of race versus a “bad” one?
Oni-Orisan: When I go to my favorite barbershop in Oakland, I know people are there not just to get their hair cut. I know there’s going to be a long line, but no one is in a hurry. I know I’m going to be entertained with animated conversation. This is how Black barbershops are.
Recently, clinicians and researchers at UCSF have taken advantage of this cultural aspect of Black-owned barbershops to provide health counseling and care to Black men with hypertension. The evidence shows that this intervention greatly improves outcomes for these men. This is an example of how race can be used – not to stereotype, but to provide more effective care – because a one-size-fits-all approach is often not the best way to care for a patient.
Le: For me, as a pediatrician working at UCSF Benioff Children’s Hospital San Francisco, I often see diseases that predominantly impact the privileged class. Cystic fibrosis is a classic example. One out of about every 3,000 white children is afflicted by this awful disease. Meanwhile, 1 out of every 300 Black children is afflicted with sickle cell disease. That’s a 10 times greater rate than for cystic fibrosis.
And yet the National Institutes of Health provides three times as much funding for the disease that afflicts mostly white children. Similarly, the amount of philanthropic dollars raised for cystic fibrosis is an order of magnitude more than for sickle cell disease, even though the amount of suffering is disproportionate in the opposite direction. This is where I think race can be used to identify and address inequity.
Possin: On the other hand, using race too often creates inequities by directing more attention or resources to whites. I recently wrote about a class action lawsuit against the National Football League filed by retired Black players. These are people who played for many years in the NFL and then later in life developed dementia. Research suggests such a diagnosis is linked to the head impacts they sustained during games. If retired players can prove they have dementia, they’re entitled to substantial monetary awards under the landmark 2013 concussion settlement.4
The current lawsuit accuses the NFL of requiring that clinicians use race as a factor in determining dementia. If you’re Black, you need to score lower on the same tests to be considered impaired enough for a dementia diagnosis. This is called race norming. It’s meant to “correct” for the average statistical difference in test scores between Blacks and whites. But I think it’s a very concerning practice because it makes it harder for a Black player than for a white player to qualify for a settlement award.
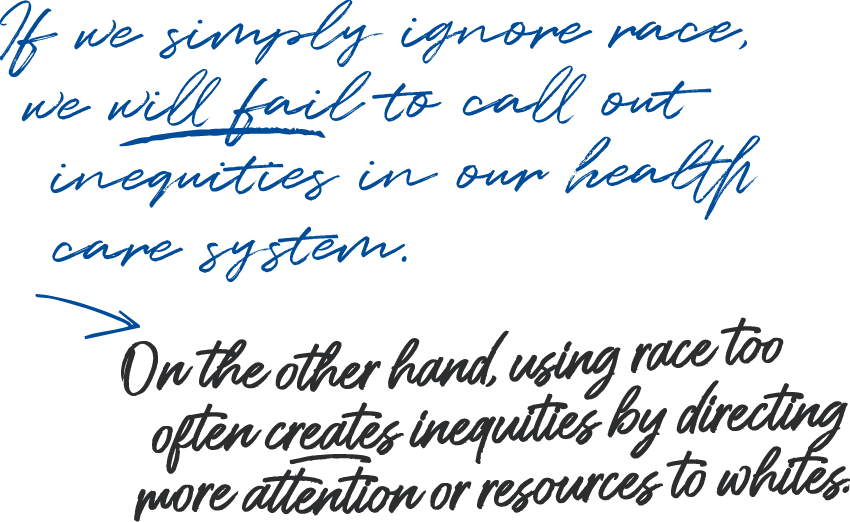
Possin: On the other hand, using race too often creates inequities by directing more attention or resources to whites. I recently wrote about a class action lawsuit against the National Football League filed by retired Black players. These are people who played for many years in the NFL and then later in life developed dementia. Research suggests such a diagnosis is linked to the head impacts they sustained during games. If retired players can prove they have dementia, they’re entitled to substantial monetary awards under the landmark 2013 concussion settlement.4
4 2013 concussion settlement: the resolution of a high-profile lawsuit in which the NFL agreed to pay retirees up to $5 million each if they have certain neurological conditions
The current lawsuit accuses the NFL of requiring that clinicians use race as a factor in determining dementia. If you’re Black, you need to score lower on the same tests to be considered impaired enough for a dementia diagnosis. This is called race norming. It’s meant to “correct” for the average statistical difference in test scores between Blacks and whites. But I think it’s a very concerning practice because it makes it harder for a Black player than for a white player to qualify for a settlement award.
Powe: But suppose you didn’t use race norming. If you just take at face value the fact that African Americans, on average, score less well on cognitive tests – which, by the way, are developed mostly from data on white Americans – you might conclude, “A lot of African Americans have some cognitive dysfunction.” That is the danger of just removing race.
I’m currently embroiled in a similar issue with how race is used in eGFR,5 an estimate of kidney function based on a patient’s age, gender, race, and level of creatinine6 in their blood. There is a well-intentioned movement to eliminate race from this calculation, but I think what’s lacking in the debate is an appreciation of the history. There’s this myth that race was brought into the eGFR calculation because of the racist idea that African Americans have more muscle mass. But that’s not quite true.
What happened was the original equation for estimating kidney function was developed in 1976 from 249 Caucasian men and extrapolated to other groups. A couple decades later, investigators began noticing that African Americans in the U.S. had higher creatinine levels than whites. We don’t know why that is, but the increase doesn’t always reflect a kidney problem. So, in 1999, the equation was updated with new study data that included African Americans (and women) and confirmed the racial differences in creatinine levels. That’s when race was factored into eGFR to account for those differences.
Critics say this race adjustment overestimates kidney function in African Americans. But what’s the alternative? If we get rid of race, then we’re just giving Black people the “white” value, which may be an underestimate.7 In my mind, that kind of normalizing can be more racist.
Is Studying Genetics by Race Inherently Problematic?
Garg: Historically, scientists often looked for biological differences between racial groups to justify white supremacy. Now we know how unfounded – and incredibly harmful and racist – that research was. Some researchers today, particularly geneticists, still study biological differences along racial lines, but with an intention to understand how these differences affect health and improve patient care. Are there concerns with using race in this way, even though the intention is good?
James: COVID is a great example. I felt frustration seeing studies looking for genetic or biological differences between racial groups to explain COVID disparities, instead of focusing on solutions to the racism that led to these disparities. For example, people of color are more likely to be infected with COVID because they are more likely to be exposed to the coronavirus due to things like the kinds of jobs they hold and the kinds of housing they can afford. This is clearly due to racism, not race. People of color are also more likely to die of COVID because of a higher burden of chronic disease – which, again, is due to environmental exposures, lack of access to health care, and other forms of structural racism.
Oni-Orisan: If you look at the literature on COVID‑19, there are many more papers on the social determinants of these disparities than on genetic factors, and deservedly so. But why is it so offensive for people to study genetic variation in populations and look for factors that may be associated with susceptibility to or severity of COVID-19? I don’t look at data on the social determinants of health disparities and say, “Why are people publishing that?” Why can’t we do both?
Powe: It’s not either/or. We need to study both and understand the interrelationship between them. Some social variables are more imprecise or just as imprecise as biological variables, in my opinion.
Oni-Orisan: I’m one of only a few Black geneticists in this country. I worry that when nongeneticists discredit the entire field of population genetics as not important – or, even worse, as racist – then minority students and trainees will be less likely to go into this field.
Powe: But suppose you didn’t use race norming. If you just take at face value the fact that African Americans, on average, score less well on cognitive tests – which, by the way, are developed mostly from data on white Americans – you might conclude, “A lot of African Americans have some cognitive dysfunction.” That is the danger of just removing race.
I’m currently embroiled in a similar issue with how race is used in eGFR,5 an estimate of kidney function based on a patient’s age, gender, race, and level of creatinine6 in their blood. There is a well-intentioned movement to eliminate race from this calculation, but I think what’s lacking in the debate is an appreciation of the history. There’s this myth that race was brought into the eGFR calculation because of the racist idea that African Americans have more muscle mass. But that’s not quite true.
5 eGFR: estimated glomerular filtration rate
6 Creatinine: a waste product from muscle that gets filtered by the kidneys
What happened was the original equation for estimating kidney function was developed in 1976 from 249 Caucasian men and extrapolated to other groups. A couple decades later, investigators began noticing that African Americans in the U.S. had higher creatinine levels than whites. We don’t know why that is, but the increase doesn’t always reflect a kidney problem. So, in 1999, the equation was updated with new study data that included African Americans (and women) and confirmed the racial differences in creatinine levels. That’s when race was factored into eGFR to account for those differences.
Critics say this race adjustment overestimates kidney function in African Americans. But what’s the alternative? If we get rid of race, then we’re just giving Black people the “white” value, which may be an underestimate.7 In my mind, that kind of normalizing can be more racist.
7 Underestimating kidney function: Potential consequences of this include prescribing an ineffective dose of medication or disqualifying a patient for life insurance or certain treatments or clinical trials.
Is Studying Genetics by Race Inherently Problematic?
Garg: Historically, scientists often looked for biological differences between racial groups to justify white supremacy. Now we know how unfounded – and incredibly harmful and racist – that research was. Some researchers today, particularly geneticists, still study biological differences along racial lines, but with an intention to understand how these differences affect health and improve patient care. Are there concerns with using race in this way, even though the intention is good?
James: COVID is a great example. I felt frustration seeing studies looking for genetic or biological differences between racial groups to explain COVID disparities, instead of focusing on solutions to the racism that led to these disparities. For example, people of color are more likely to be infected with COVID because they are more likely to be exposed to the coronavirus due to things like the kinds of jobs they hold and the kinds of housing they can afford. This is clearly due to racism, not race. People of color are also more likely to die of COVID because of a higher burden of chronic disease – which, again, is due to environmental exposures, lack of access to health care, and other forms of structural racism.
Oni-Orisan: If you look at the literature on COVID‑19, there are many more papers on the social determinants of these disparities than on genetic factors, and deservedly so. But why is it so offensive for people to study genetic variation in populations and look for factors that may be associated with susceptibility to or severity of COVID-19? I don’t look at data on the social determinants of health disparities and say, “Why are people publishing that?” Why can’t we do both?
Powe: It’s not either/or. We need to study both and understand the interrelationship between them. Some social variables are more imprecise or just as imprecise as biological variables, in my opinion.
Oni-Orisan: I’m one of only a few Black geneticists in this country. I worry that when nongeneticists discredit the entire field of population genetics as not important – or, even worse, as racist – then minority students and trainees will be less likely to go into this field.
James: Absolutely, and I certainly didn’t intend to imply that your work is racist. In fact, I think the work you and other geneticists are doing to look at differences across diverse populations and identify genetic risks for disease is critically important. My point is that genetic diversity across populations is not the same as racial categorizations, and I get concerned when I see studies conflating the two.
We often take too narrow a view in medicine, thinking about health as being just biology and not thinking about health as being the entire social structure. For many people, the five racial categories8 that the National Institutes of Health uses don’t make sense. I identify as Black, but I’ve also identified as mixed. So do I count as Black, or do I count as not-Black? My children – who are half me and half white – are they Black? Where’s the line? These groups don’t have an inherent biological meaning.
Oni-Orisan: I would argue that racism is also not the same as racial categorizations. Race is complex and captures multiple components, including genetic ones. We have to acknowledge that genetic differences between racial groups do exist and can have clinical significance. So even though social factors play the largest role in racial health disparities, we also need to address other factors, including genetics. As a geneticist, I consider myself a health disparities researcher.
Where Do We Go From Here?
Garg: How do we use race appropriately – not to discriminate but to deliver equitable care?
Possin: We have to keep measuring race because that’s how we can identify disparities. We have to make sure that our care clinics are serving a diverse population that represents our region. If they’re not, then we need to do outreach to the communities that are not coming into our clinics. Because if we just wait for who makes it in our door, we’re going to get an advantaged slice of the population. We need to go out and find the patients who need our care.
James: We also need to be more consistent and transparent with how we talk about race in our studies. What do we mean by race? Is it patient-reported? Is it provider-reported? Is it whatever ended up in the electronic health record? Or is it something like ancestry?
And we need to have more nuanced conversations about race with our patients. If I’m asked to check a race box, no one’s saying, “This is what we’re going to do with this information; this is what it might mean for you.”
For instance, let’s say having darker skin puts you at greater risk for a certain disease. It would be useful for a patient from the Dominican Republic to know that and realize, “Oh, it’s important for me to articulate that I have dark skin in this answer.” Or maybe it’s ancestry, not skin color, that a clinician or researcher really needs to know. So if this patient has three white grandparents, they might decide it’s important to indicate the white part of their background even though they might identify as Black.
Oni-Orisan: One of the key issues, historically speaking, is the idea of hierarchy – that there’s one race that’s superior to others. This idea is unscientific; it’s not appropriate. What I’m advocating for is to celebrate and study differences between populations without the idea of hierarchy. I think that’s how we can make progress.
Le: Right now, every single institution in this country is reckoning with their own racist history, including UCSF. It’s an amazing time, but it’s also a tense time. I sense that tension even in this Zoom call.
My prescription for using race is to first acknowledge that in medical research and practice, we’ve had actions and policies that have been informed by structural racism. Then we need to ask ourselves, “What is the preferential option?” In the case of disproportionately low funding for sickle cell disease, the preferential option would be to dramatically increase it. Some people will call this a form of reparations. For me, it’s simply prioritizing the group that has been oppressed and has suffered the most.
James: In some ways, I feel like we’re arguing the same thing from different perspectives. Many of us think the way we’re using race now is inappropriate, and the ultimate goal is to do something different.
Powe: It’s health equity that we want, right? That’s what we’re all aiming for, no matter what it takes to get there.
Ariel Bleicher and Elizabeth Daube produced and edited this article.
Portrait Illustrations: Stephanie Koch
James: Absolutely, and I certainly didn’t intend to imply that your work is racist. In fact, I think the work you and other geneticists are doing to look at differences across diverse populations and identify genetic risks for disease is critically important. My point is that genetic diversity across populations is not the same as racial categorizations, and I get concerned when I see studies conflating the two.
We often take too narrow a view in medicine, thinking about health as being just biology and not thinking about health as being the entire social structure. For many people, the five racial categories8 that the National Institutes of Health uses don’t make sense. I identify as Black, but I’ve also identified as mixed. So do I count as Black, or do I count as not-Black? My children – who are half me and half white – are they Black? Where’s the line? These groups don’t have an inherent biological meaning.
8 NIH’s five racial categories: American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or other Pacific Islander, White (plus two categories for ethnicity: Hispanic or Latino and Not Hispanic or Latino)
Oni-Orisan: I would argue that racism is also not the same as racial categorizations. Race is complex and captures multiple components, including genetic ones. We have to acknowledge that genetic differences between racial groups do exist and can have clinical significance. So even though social factors play the largest role in racial health disparities, we also need to address other factors, including genetics. As a geneticist, I consider myself a health disparities researcher.
Where Do We Go From Here?
Garg: How do we use race appropriately – not to discriminate but to deliver equitable care?
Possin: We have to keep measuring race because that’s how we can identify disparities. We have to make sure that our care clinics are serving a diverse population that represents our region. If they’re not, then we need to do outreach to the communities that are not coming into our clinics. Because if we just wait for who makes it in our door, we’re going to get an advantaged slice of the population. We need to go out and find the patients who need our care.
James: We also need to be more consistent and transparent with how we talk about race in our studies. What do we mean by race? Is it patient-reported? Is it provider-reported? Is it whatever ended up in the electronic health record? Or is it something like ancestry?
And we need to have more nuanced conversations about race with our patients. If I’m asked to check a race box, no one’s saying, “This is what we’re going to do with this information; this is what it might mean for you.”
For instance, let’s say having darker skin puts you at greater risk for a certain disease. It would be useful for a patient from the Dominican Republic to know that and realize, “Oh, it’s important for me to articulate that I have dark skin in this answer.” Or maybe it’s ancestry, not skin color, that a clinician or researcher really needs to know. So if this patient has three white grandparents, they might decide it’s important to indicate the white part of their background even though they might identify as Black.
Oni-Orisan: One of the key issues, historically speaking, is the idea of hierarchy – that there’s one race that’s superior to others. This idea is unscientific; it’s not appropriate. What I’m advocating for is to celebrate and study differences between populations without the idea of hierarchy. I think that’s how we can make progress.
Le: Right now, every single institution in this country is reckoning with their own racist history, including UCSF. It’s an amazing time, but it’s also a tense time. I sense that tension even in this Zoom call.
My prescription for using race is to first acknowledge that in medical research and practice, we’ve had actions and policies that have been informed by structural racism. Then we need to ask ourselves, “What is the preferential option?” In the case of disproportionately low funding for sickle cell disease, the preferential option would be to dramatically increase it. Some people will call this a form of reparations. For me, it’s simply prioritizing the group that has been oppressed and has suffered the most.
James: In some ways, I feel like we’re arguing the same thing from different perspectives. Many of us think the way we’re using race now is inappropriate, and the ultimate goal is to do something different.
Powe: It’s health equity that we want, right? That’s what we’re all aiming for, no matter what it takes to get there.
Ariel Bleicher and Elizabeth Daube produced and edited this article.
Portrait Illustrations: Stephanie Koch