It was February 1985 when Jill Lawson suddenly found herself in labor, three months early. Baby Jeffrey was born at Columbia Hospital for Women in Washington, D.C., at 26 weeks’ gestation, weighing just 1½ pounds. He was alert and active but gravely ill.
Two weeks after his birth, Jeffrey’s health took a turn for the worse: He developed a heart defect common in premature infants – patent ductus arteriosus, or PDA. Jeffrey was scheduled for open-heart surgery and transferred to the nearest children’s hospital.
In those days, surgery for PDA was invasive. Holes were cut on either side of Jeffrey’s tiny neck and chest to insert a catheter into his jugular vein. His little body was opened from breastbone to backbone, his flesh lifted aside, ribs pried apart, and a blood vessel near his heart tied off, and then all the tissues were stitched back together.
Baby Jeffrey felt everything – every incision, every internal repair, every stitch. The medical team had not given their fragile patient any drugs, any comfort, anything to protect him from the excruciating pain of open-heart surgery – just a paralyzing agent to keep him still during the procedure.
Five weeks later, Jeffrey passed away.

In the days before her child’s death, Jill Lawson learned a shocking fact: Anesthetizing babies for surgery was not common practice. After Jeffrey died, Lawson called his doctor for reassurance. Surely, she thought, her child had been given something for the pain.
“The anesthesiologist informed me that she had not used any anesthesia or analgesia on Jeffrey,” Lawson wrote in an account of her son’s experience. The doctor told the grieving mother it hadn’t even occurred to her to do so because it had never been demonstrated that babies can feel pain.
Jeffrey’s experience was far from unique. When Lawson took her son’s story to the New York Times, the newspaper found that the vast majority (77%) of newborns who underwent surgery to repair PDA between 1954 and 1983 had received only muscle relaxants and nitrous oxide, an antianxiety medication and very weak anesthetic. For decades, physicians routinely operated on babies with little or no anesthesia, based on the widely held belief that infants are too primitive an organism to feel pain and that potent anesthetics might kill them.
Jeffrey’s death marked a turning point. In 1987, the American Academy of Pediatrics declared it unethical to operate on newborns without anesthetics. But even today, 35 years later, disturbing echoes of Jeffrey’s experience remain: Hospitals consistently fail to fully ease the pain of their young patients.
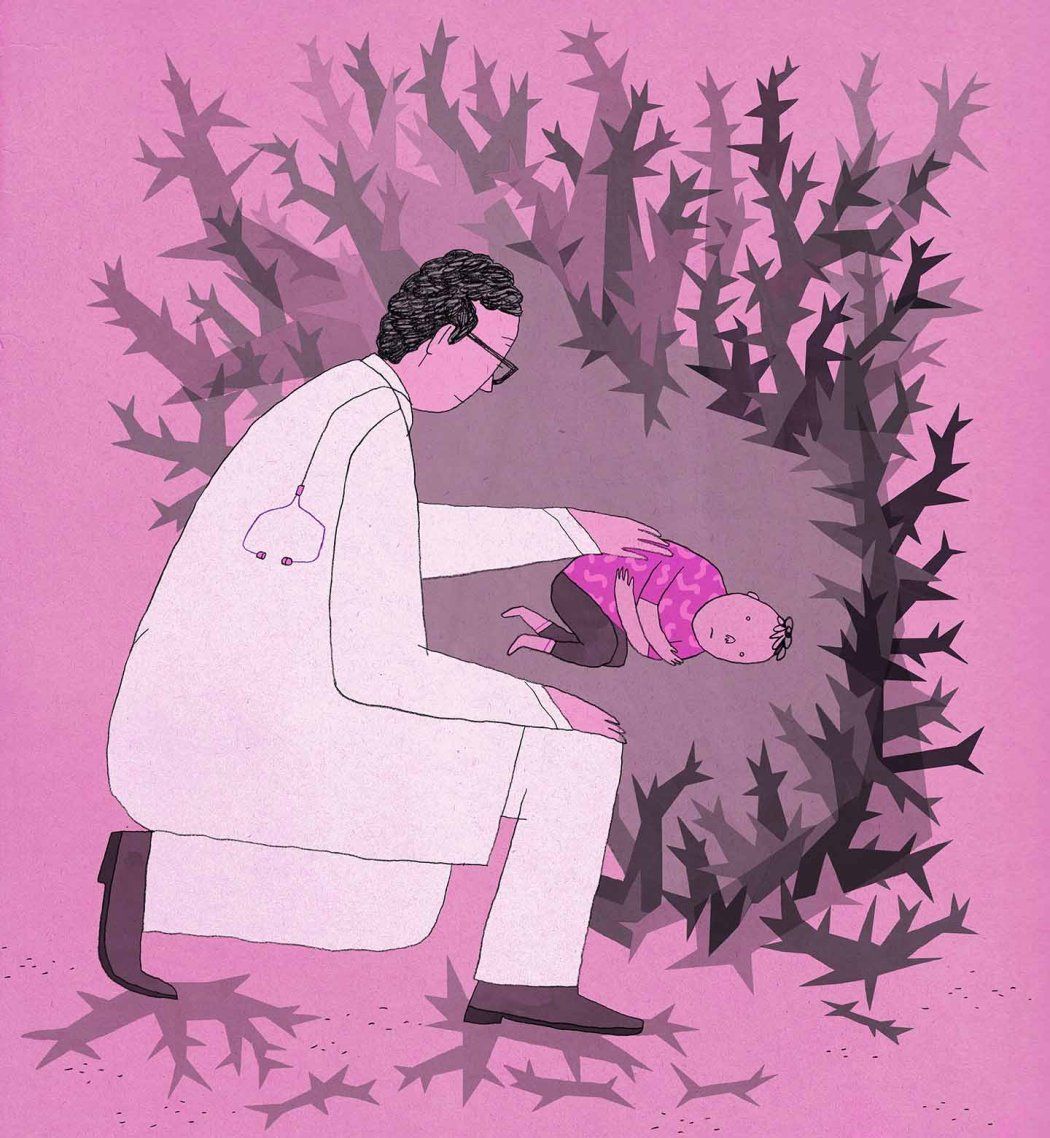
“Study after study shows that children’s pain – whether it’s related to a procedure or an injury, chronic or acute – is vastly underrecognized and undertreated in children’s hospitals worldwide,” says Stefan Friedrichsdorf, MD, UCSF’s Stad Professor of Pediatric Pain Medicine, Palliative Care, and Integrative Medicine. “And the younger the child, the less likely they are to get the pain relief they need – whether through medications or other proven approaches to pain management.”
The implications are profound: For children, lack of pain care can lead to anxiety and depression, heightened sensitivity to pain later in life, and avoidance of health care in adulthood, including lifesaving vaccinations.
In 2010, two UCSF pediatricians – Stephen Wilson, MD, PhD, and Karen Sun, MD – began exploring what it would take to tackle this problem head-on, for every hospitalized child in pain at UCSF. They wanted to combine a range of techniques – from conventional medicines to complementary integrative therapies, such as acupuncture and massage. They consulted with Friedrichsdorf, then-director of the country’s first pediatric pain program, at Children’s Minnesota, and the world’s foremost expert on children’s pain.

“We realized that our patients needed more, that we needed to broaden our view of what pain management means and incorporate a whole spectrum of therapies,” says Sun. “We started out small, but we have been able to transform how this hospital thinks about children in pain. Our vision was to build a program that would become a destination center.”
A dozen years later, thanks to a $3 million investment from Elisa and Marc Stad, their vision has become a reality. In 2021, UCSF launched the Stad Center for Pediatric Pain, Palliative, and Integrative Medicine, one of the most comprehensive and innovative pediatric pain programs in the country. The center brings together multiple approaches, including advanced and safe drugs, with integrative medicine, psychology, and physical therapy, to care for patients. Friedrichsdorf was recruited as the center’s inaugural medical director and chief of the Division of Pediatric Pain, Palliative, and Integrative Medicine.
Seven years before Jeffrey Lawson was born, Friedrichsdorf was 9 years old and playing outside his home in Germany when he suddenly became sick and spiked a fever. His parents took him to the local hospital, where doctors discovered a severe infection in one of his fingers. His body was going into sepsis.
At the hospital, Friedrichsdorf was separated from his parents and brought to a surgical room. Without warning or explanation, a nurse held him down while doctors cut into both sides of his finger to drain the pus that had accumulated in it. “I was alone. I was anxious. And it was so painful. I was screaming at the top of my lungs,” he says. “And I remember to this day, that one surgeon said to the other, ‘Do you think he can feel any pain?’ and the other one said, ‘No, he can’t.’”
Friedrichsdorf developed a lifelong fear of needles and anxiety related to medical procedures, which is why his eventual decision to pursue medical school was unexpected. He experimented with a long list of other career paths before settling on life as a doctor: newspaper carrier, tour guide, factory worker, actor, journalist, children’s theater director, camp counselor, and paramedic.
It was during his time as a camp counselor that Friedrichsdorf first noticed the calming effects of mind-body techniques on children. At the end of a long day in the wilderness, his campers having been energized by hours in the elements, Friedrichsdorf used guided imagery – storytelling designed to evoke a relaxed, peaceful mental state – to help the kids calm down, snuggle into their sleeping bags, and fall asleep around the campfire. As a paramedic, he employed guided imagery again, as well as distraction and aromatherapy, to relax children in severe pain and distress.
But when Friedrichsdorf started medical school in the 1990s, he was shocked to find that children’s pain, as well as all the distress and anxiety associated with pain, was rarely prioritized in pediatric hospitals, whether through drugs, mind-body techniques, or a combination of the two.
“Pain control in children’s hospitals was still new,” he says. “I was working with children with cancer, but their pain was not being managed well. I saw kids being held down and screaming. Hospitals and clinics claim that they never have enough staff to provide appropriate pain control to children, but they always seem to have enough staff to hold children down. I thought to myself, ‘I can do this better.’”
I saw kids being held down and screaming. ... I thought to myself, ‘I can do this better.’”
Stefan Friedrichsdorf, MD
Friedrichsdorf sought out training but found no coursework, no medical specialty, anywhere in Europe, devoted to pediatric pain. “Then I learned that the first fellowship for pediatric pain and palliative care was being offered at the University of Sydney, Australia, and I went for it,” he says. “It was life-changing. I worked with every single pain patient in the children’s hospital, and I realized ‘This is not rocket science. We can do this in children’s hospitals.’”
It may not be rocket science, but the science of pediatric pain is more complex than one might think.
From a biological standpoint, the basic idea is this: When a tissue injury occurs, sensory receptors in our tissues send a message to the brain, where the sensation is registered, the information is processed, and the pain is perceived. But that biological process is just one piece of the puzzle.
Friedrichsdorf likes to use a hypothetical example involving 100 children jumping on a trampoline. If all 100 sprain their ankles, why do 98 of them go on to become pain-free, but one or two of the children experience debilitating and prolonged ankle pain?
The answer is, because pain is complicated. “The severity of the injury or infection does not necessarily correspond to the personal experience of pain,” says Cristina Benki, PhD, a UCSF pediatric pain psychologist who works closely with Friedrichsdorf. “What we have to ask is ‘What are the other factors that influence that individual experience?’”
In fact, the biological aspect of the pain – the tissue damage itself – is interacting with psychological and social factors that also influence how pain is perceived. For children, feelings of pain can be deepened by anxiety and depression, as well as by social factors like how they were taught to think about pain and by family trauma like financial instability, divorce, or domestic violence.
Research shows that everything is connected when it comes to pain. “So much about pain is psychological,” says Benki. “How we experience pain is about the environment that your brain and body are raised in. How we learned to cope with stress. How our minds work – whether we tend toward more negative or positive thinking. All these factors contribute to the pain experience. But the bottom line is that the pain is very real.”
So much about pain is psychological. ... But the bottom line is that the pain is very real.”
In other words, it’s possible that those children with debilitating ankle pain were going through something else in their psychology or home life – heightened stress at home, a family history of chronic pain, an anxiety disorder, or other such issues – that triggered an additional stress response in the brain that, in turn, worsened the physical sensation.
“Stress, anxiety, depression, perceived injustice, even disturbed sleep, are what we call facilitatory ascending inputs,” says Friedrichsdorf. “These are pathways in our brains – all the way from the thalamus to the prefrontal cortex – that can actually increase the perception of pain.”
The good news: “We can interrupt this process,” says Benki. “We can intervene and either change the environment or the internal experience through a combination of safe pain medications, psychotherapy, mind-body techniques like hypnosis and guided imagery, and other interventions. We can change the pain experience and help these kids get better.”

Friedrichsdorf first began using hypnosis with children in pain during his fellowship in Australia. Today, it’s an integral part of his practice at the Stad Center.
“When people think of hypnosis, they imagine I say a few magic words and snap my fingers and you then give me all your chocolate,” Friedrichsdorf says. “That’s not how it works. In my practice, hypnosis is about guiding a subject through an alternative state of awareness with the expressed, explicit purpose of reducing discomfort.”

Take Jimmy, a 17-year-old patient who has been in and out of the hospital for years with a painful gastrointestinal condition so severe that pain medications offered little relief. Friedrichsdorf met with Jimmy to learn more about his discomfort and offered hypnosis. During Jimmy’s first session, Friedrichsdorf asked him to imagine a safe and favorite place. “Are you alone?” he asked. “What do you hear? Can you smell anything? Do you feel the sun on your face?”
Having been bed-bound for weeks, Jimmy chose to go to an amusement park. He felt the wind in his hair as he wandered among the attractions. He heard children’s voices rise and fall in collective excitement as a roller coaster gained speed in the distance. He breathed in the smell of popcorn and sweet treats.
With Jimmy relaxed and enjoying the park, Friedrichsdorf dug deeper. “What do you want to get rid of?” he asked. “My pain,” Jimmy answered. So Friedrichsdorf asked Jimmy to imagine a trash can, put his pain into it, and destroy it. Jimmy gathered up and detonated his pain. “How do you feel?” Friedrichsdorf asked. The pain had lessened, Jimmy said, from a 10 out of 10 to a 6.
Mind-body techniques like hypnosis, guided imagery, and meditation activate the same part of the brain – known as the periaqueductal gray – that pain medications like morphine and fentanyl target. “If you have severe pain because you just burnt your leg with hot coffee and I give you some morphine, the pain goes away,” says Friedrichsdorf. “If I look at what’s happening in your brain at that moment, the periaqueductal gray is lighting up and decreasing the pain signals reaching your brain. If you practice hypnosis, if you do guided imagery, if you do meditation, the same part of the brain that is activated by opioids is activated by those techniques.”
Friedrichsdorf acknowledges that the fear of overmedicating a small child is a legitimate concern. “But if a child has pain, it’s not just about giving them medications anymore. It’s about combining a lot of different modalities at the same time to provide the best possible pain control with far fewer side effects.”
At UCSF, Friedrichsdorf’s team of clinicians treats children in pain using a unique combination of pain medications (including analgesics and anesthesia), integrative therapies (such as mind-body techniques like hypnosis and massage), psychotherapy (such as cognitive behavioral therapy), and rehabilitation (including physical therapy).
Their approach has yielded profound results for children, from infancy to young adulthood.
UCSF integrative medicine specialists explain the power techniques like acutherapy to help heal pain. Video: Lawrence Rickford
Dylan is one such patient. Dylan had been in severe abdominal pain from the time they were 2 years old. It had taken the joy out of birthday parties, family outings, play dates, and school. When a fun event approached, little Dylan grew anxious that their pain would flare and cause a scene – like the time they couldn’t resist a bite of pizza at a mini-golf birthday party and ended up vomiting into a trash can while the other children looked on.
Dylan was finally diagnosed with Crohn’s disease at 13 and put on opioids to control their discomfort. Whenever pain erupted, doctors either upped Dylan’s dosage to alarming levels or dismissed their concerns. By the time Dylan was transferred to UCSF Benioff Children’s Hospital San Francisco at 19, they were in debilitating pain, dependent on opioids, unable to walk, and deeply traumatized by a lifetime of distressing hospital experiences.
The UCSF team told Dylan the pain could be controlled without opioids, but it would take work. Dylan dove in. They committed to physical therapy despite their discomfort and came to embrace a new exercise routine. They tried acutherapy (an umbrella term that encompasses acupuncture and acupressure), massage, and art therapy, and learned how to use drawing to distract them from the pain. And they unpacked their trauma with Benki in therapy, where they practiced techniques like deep breathing and guided meditation that they could take forward on their own.
Six months later, Dylan was off opioids, managing their pain effectively, walking with assistance, and immersed in a creative practice. “I incorporate all of it into my daily life – the techniques I did in psychotherapy, the exercises I did in physical therapy, the art, acupuncture. I don’t think I’d be able to function without that experience.”
The Stad Center’s pain specialists love sharing stories like Dylan’s: real-life evidence that their teamwork can have a life-changing impact on their young patients. But their passion is often accompanied by a sense of urgency: The demand for comprehensive pain care is enormous, and the center’s capacity to meet those needs is falling short.
In part, the challenges are structural. The health care industry has been slow to catch up to Friedrichsdorf’s vision for modern integrative pain care. Insurance companies do not reimburse for most of the Stad Center’s services, and the pool of specialists is limited due to persistent gaps in medical education focused on children’s pain. The center relies largely on private support to provide the care that gave Jimmy and Dylan relief and to conduct the training and research that advance the field. But that support is barely scratching the surface when it comes to the urgent needs of current patients.
“Like any other medicine, you want to make sure you’re giving the right dose,” says Robyn Adcock, director of integrative medicine and a pediatric acupuncturist. “But I have a limited service, so it’s always a balance: How do we share these services equitably? If you spread them too thin, they’re not effective for anyone. It’s like you don’t have enough insulin and everyone needs it. You’re only going to be able to help a few patients get better.”
Adcock and her colleagues are advocating for changes to insurance policies on the state and national levels. The team is also finding creative ways of expanding access to integrative therapies within the hospital system itself, particularly for patients who would otherwise be unable to afford such services.

Integrative medicine specialist Jenifer Matthews, MD, is based at UCSF Benioff Children’s Hospital Oakland. Matthews and her team secured a grant to offer acupuncture at the hospital’s community clinic, where 92% of patients fall below the poverty line. “It was immensely popular and helpful,” she says. But when the grant ran out, they lost their acupuncturist. “Now I offer acupuncture as much as I can … but it’s not enough. We want to do more.”
Friedrichsdorf acknowledges that the establishment of the Stad Center as the nation’s first standalone medical division devoted to pediatric pain was groundbreaking and has the potential to transform how children in pain are cared for. But he has his work cut out for him. Reaching every patient in need with comprehensive care will take time, philanthropy, and a significant shift in national health care policy.
“In pediatric medicine, the number-one priority, of course, is still ‘Can I make this child survive?’” says Friedrichsdorf. “Comfort and pain are usually not the priority. They are certainly not a priority for insurance companies. Most of these services are not reimbursable.
“UCSF Benioff Children’s Hospitals are amazing children’s hospitals. We have thousands of clinicians and researchers who get up every morning to eradicate disease. Our team gets up every day to eradicate pain and suffering. But the only way we can do that – the only way our patients can see this team, see a psychologist, get acupuncture or massage – is through community support.
“The establishment of the Stad Center is huge, and I am so excited to be here. Things are really starting to change, but we do need community support to help our patients right now, today, and to show the world how incredibly valuable this work is.”