Helping People Die from 3,000 Miles Away
Palliative care expert Alex Smith has guided the families of COVID-19 patients in New York through the hardest decisions of their lives – by phone from San Francisco.
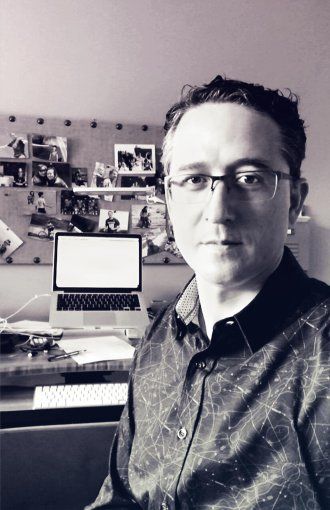
Alex Smith, captured via FaceTime in his home office in Mill Valley, Calif., on June 10 at noon by photographer Steve Babuljak
Hearing the stories coming out of Italy – the scarce resources, the confusion, the lonely deaths – geriatrician and palliative care physician Alex Smith, MD ’02, MPH, MS, could sense a tsunami headed for the U.S. In March, he and his UCSF colleague Eric Widera, MD ’02, began interviewing palliative care leaders in early coronavirus hot spots like Seattle. How should they and others prepare?
As the virus barreled into New York City, Boston, and other cities, they also interviewed the palliative care clinicians confronting those onslaughts. The wrenching challenges faced by the doctors at NewYork-Presbyterian Hospital haunted Smith. When they later called to ask for help, he and other palliative care experts at UCSF quickly said yes.
In his own words, Smith shares his virtual journey into the epicenter of the pandemic and the surprising lesson he learned about delivering care by phone.
The NewYork-Presbyterian team includes five palliative care physicians, plus social workers and nurse practitioners – a relatively small service for a large hospital. Normally, they care for about 20 patients. During the worst of the surge, their count hit 90.
First, the emergency department called their team and said, “We need a palliative care physician embedded in the ED.” Then the ICU called with the same urgent request. So many patients were on ventilators doing poorly, their kidneys and other organs failing. The ED needed help talking with patients’ families. The hospital went from fewer than 100 ICU patients to 250 at its peak.
Their palliative team asked us if we could manage the patients who were dying, where the focus is on comfort. “UCSF does that best,” they said, “and this will free us to care for other patients.”
Several of us stepped in and started doing telephone palliative care consults from San Francisco. We felt a lot of anxiety up front. Usually when I do a consult, the family comes in, and they can see how sick their loved one is. “Tell me what they were like before,” I will say. Maybe they enjoyed singing, dancing, cooking. Then I can explain that we hope they’ll get back to that place, but we need to prepare in case things don’t go the way we hope.
But these families could not go into the hospital. They couldn’t see their loved ones, and we couldn’t read the family members’ facial expressions, their body language.
As soon as I started doing these calls, however, I realized, “Hey, I can do this.” These are like the conversations I’m used to having: challenging, but also very meaningful. You build a relationship by asking how they are coping, and then you talk about prognosis. We were like a lifeline to these families, who wanted to talk about their loved ones, their rich lives before COVID, and their hopes and fears for what lay ahead.
We would often talk to families through a translator because many of the patients were Latino, and the families primarily spoke Spanish. We would use the words that the ICU physicians used with us: We’d explain that their loved one was dying. We’d explain how they were being cared for as they were dying.
Sometimes those conversations led to patients moving to the dedicated palliative care unit, the only place in the hospital where family members could come in. We had one instance where it was very important to a daughter to hold her mother’s hand at the end of her mother’s life. Her mom was on a ventilator and blood pressure support medicines. Normally, these drugs are administered only in the ICU, but we knew she would die there if they were stopped before she was moved to the palliative care unit. We were able to arrange an exception so we could move her while she was still on the drugs. When they took her off the ventilator, her daughter was there to hold her hand as she was dying. It meant so much to her.
Other families have said, “We want to do everything for our mother.” We got to a point with one family where we had to say, “You should feel like you’ve done everything, because you have, and she’s still dying. Now we feel we should shift the focus to keeping her comfortable.” They could never have said those words to us, but they were able to agree when we made that strong recommendation. I think they felt some relief at having the burden of the decision lifted off of them. That was a powerful experience.
More recently, we’ve had a wave of consults for people who are coming off of ventilators but are not waking up or are really physically disabled. There’s a huge amount of uncertainty and concern that they’ll never get back to being the person they were before all of this.
Families are so grateful to have somebody who can talk with them, who gives them daily updates. Providers in New York are so busy, it’s tough for them to reach out to families regularly or to answer all of their questions. We have time to do that because San Francisco hasn’t been hit hard by COVID-19. It’s been a privilege to help.
It’s hard work being exposed to all the challenges the families are going through, the raw emotions. At the same time, we can feel that we’re doing important work when family members are so appreciative of us walking along on this difficult journey with them.

More from this Series
Call navigator Monique Posey fields questions about the pandemic. She shares her story – and some of her strategies for coping with stress.



