School of Nursing
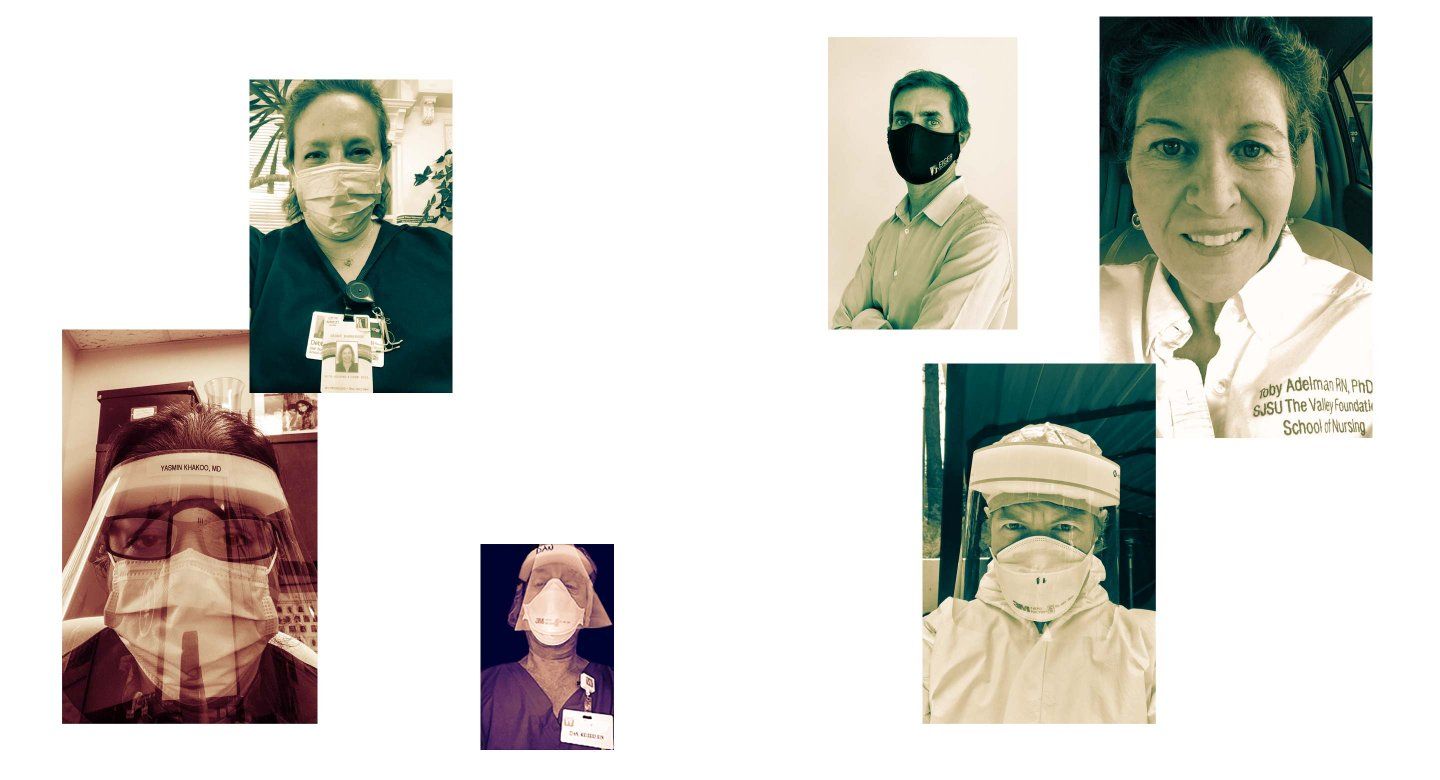
Toby Adelman, MS ’93, RN, PhD ’07
After 40 years in nursing, including a decade at UCSF in neurosurgery, and most recently having taught community and public health nursing at the San Jose State University School of Nursing, I retired last year and moved from California back to my home state of Maine. Wanting to contribute, I recently took the contact tracing certificate program offered by the Johns Hopkins Bloomberg School of Public Health and am registered with Maine Responds to be a volunteer contact tracer. Maine has the oldest population in the US; Aroostook County, the largest and northernmost in Maine, is home to Maine’s oldest and most vulnerable population to COVID-19. I am hoping to be part of mitigating the pandemic here in my neck of the woods.

School of Medicine
Catherine Forest, MD ’90, MPH
When the shortage of personal protective equipment (PPE) became apparent in my county, I formed a collaboration with the maker community, local medical societies, a print shop, and nonprofits to match donated, certified PPE with essential workers not in the standard “surge” network of hospitals and also in the nonprofit world for residential care, Meals on Wheels, nursing homes, etc. When none was available, I started a GoFundMe account and worked on innovation for an N95-inspired mask and a model to pay unemployed local seamstresses to make them to outfit essential workers with cloth masks. Now ppe4cc.org has distributed close to 45,000 donated and locally sewn masks to Central Coast agricultural workers. In conjunction with a partner, Idea Fab Lab, we have distributed locally designed plastic desk tops and free-standing barriers to serve at test sites when full PPE has not been available. In addition, we have developed an infographic on putting on and removing PPE and the care of face coverings, as well as concepts of physical distancing, face coverings, and safer-in-place for use where literacy and multiple languages affect education about COVID-19. Lastly, in my role as chair of a large nonprofit with many residential care sites, even before any of the safer-in-place regulations, we closed to new admissions and began using masks and social distancing, and we have had zero cases in our residential sites.
School of Nursing
Laurie Flaherty, MS ’92
For the past 15 years, I have been the coordinator of the National 911 Program, a federal program established to support the people who answer 911 calls. After 25 years “at the bedside,” as mostly an emergency nurse and a clinical nurse specialist, I decided that helping people is not confined to clinical care, nor is it limited to one-on-one interaction. I honed the required skills for this position as a clinical nurse, through my involvement in the Emergency Nurses Association and during my graduate studies at UCSF while earning an MS in emergency and trauma nursing. Earlier this year, 911 Program was tapped to provide 911 subject-matter expertise to FEMA’s national COVID-19 Supply Chain Task Force, and I have had the opportunity to provide a population-based approach to [pandemic-related] issues brought to the task force. During this experience, I have been grateful to have my UCSF education to fall back on, and more than that, my UCSF perspective – to think with great imagination but always with the patient’s – in this case, the 911 caller’s – needs as my first priority. Thanks, from a proud UC alum.
Graduate Division
Dan Keller, RN, MS ’83
Keller wrote that he has been volunteering in a Bay Area skilled nursing facility (SNF) in a unit in which all the residents have tested positive for COVID-19. He’s written about his experiences on his blog, including this post from May 2020:
SNFs have been getting a bad rap lately.
Their residents suffer a disproportionate share of COVID-19 deaths. The implication in a recent spate of articles in the press is that these institutions have delivered substandard care or worse, driven by rapacious administrators and capitalistic owners to cut corners and let patients sicken and die.
While such abuses have surely occurred, I maintain that these are a vanishingly small minority and that very nearly all such institutions have performed well, even in the face of daunting odds. What are those odds?
First, SNF residents are by definition the most vulnerable demographic: elderly, beset by numerous comorbidities, often surviving by the merest thread, sustained only by, well, skilled nursing. Throw a deadly virus into this mix, and the outcomes are inevitably poor.
Second, the designs of these places are commonly outmoded. If we were to redesign them today (and many have; for example: the New York Times: As Death Toll in Nursing Homes Climbs, Calls to Redesign Them Grow), each resident would have a private room. The HVAC/ventilation systems would exhaust to the outdoors instead of recirculating. Shared spaces would support social distancing. The number of residents in a nursing unit (“pod”) would be perhaps a half dozen instead of the two or even three dozen common in today’s SNFs, most of which were designed many decades ago.
So today the odds are against us. What can we do? Bulldoze and rebuild? Where’s the money for that?
In practical terms, let’s do what’s possible within the constraints of reality, and point fingers only when the malfeasance is real, which it rarely is. In defense of SNFs, please understand the realities. And go (skilled) nurses!

School of Nursing
Jennifer Lang-Ree, MS ’99, PNP, CPNP
I am a pediatric nurse practitioner in Truckee, Calif. When COVID-19 hit our area, we scrambled to quickly set up an outside, drive-up clinic to keep potential COVID out of our indoor clinics. I volunteered, along with many other nurse practitioners and physician assistants, to be the providers for this clinic. I have been working there since March. In Truckee, our weather is unpredictable, so we’ve worked through days that it snowed 3 feet, through hail and rainstorms, and now in 80-degree heat. We see all patients who have respiratory or new gastrointestinal symptoms and evaluate them in their cars so we don’t have to expose anyone else in a clinic. I love the group of staff who all volunteered to run this clinic. I have developed friendships with other staff from all over the hospital that I would never have otherwise due to this crisis.
School of Medicine
Pradeep Natarajan, MD ’08, and Puja Kohli, MD ’08
Natarajan shared this Wall Street Journal article, which explores how “Puja Kohli and Pradeep Natarajan, 37-year-old physicians at Massachusetts General Hospital and Harvard Medical School, struggle to balance caring for their almost 4-year-old twins with demanding jobs that expose them to patients with COVID-19.”
School of Pharmacy
Marissa Horrigan, PharmD ’13
I am working at Cedars-Sinai Medical Center as an investigational drug services pharmacist, helping oversee numerous COVID-19 studies on a variety of different investigational products.
School of Pharmacy
Matt Bryant, PharmD ’02
Eiger BioPharmaceuticals (Eiger) is developing peginterferon lambda (Lambda) for hepatitis delta virus (HDV) infection. At the beginning of the COVID-19 pandemic, multiple independent published reviews by experts in the field advocated for exploring Lambda in COVID-19, both as a prophylaxis for exposure and treatment of mild disease. Overwhelming advocacy by investigators who were willing to fund and conduct Lambda trials, combined with a strong desire by Eiger management to support and advance the fight against the global COVID-19 pandemic, led us to collaborate with clinicians at key academic centers, which are now screening, enrolling, and dosing patients with Lambda across multiple U.S. and international sites, with a goal of proof of concept.
In total, there are six investigator-sponsored studies evaluating Lambda in COVID-19 at Stanford University, Johns Hopkins University, Massachusetts General Hospital, Mount Sinai Hospital, Toronto General Hospital, and Soroka University in Israel. Eiger has been involved in protocol development and regulatory agency interactions and is providing Lambda clinical drug supply. These are short duration studies, exploring one to two subcutaneous weekly injections of Lambda, and offer multiple opportunities to quickly prove concept of Lambda’s ability to reduce viral replication, reduce symptomatology, and limit virus transmission.

Lambda interferon plays a key role in the targeted innate immune response against viral pathogens that infect the respiratory tract. Upon infection of airway epithelial cells, type III IFNs, like lambda interferon, are produced first and act as the initial line of defense to limit virus spread at the epithelial barrier without triggering inflammation. A recent mouse-adapted SARS-CoV-2 model demonstrated Lambda’s ability to decrease viral replication in lung titers. The investigator-sponsored studies will investigate the hypothesis that Lambda may be most effective in patients who have confirmed infection with mild symptoms or prevention in patients with exposure to COVID-19.
Lambda has been administered to over 3,000 subjects in 19 clinical trials of viral hepatitis infection. It is an investigational agent and is not yet approved for any indication. Adverse events seen previously were mostly mild to moderate and included musculoskeletal and flu-like symptoms, transaminase elevations, and increased bilirubin.
A treatment for COVID-19 is desperately needed. We believe that Lambda could play a role in prevention and treatment of patients, health care providers, first responders, and caregivers who have been infected by or exposed to SARS-CoV-2. Stay tuned for our results.

School of Dentistry
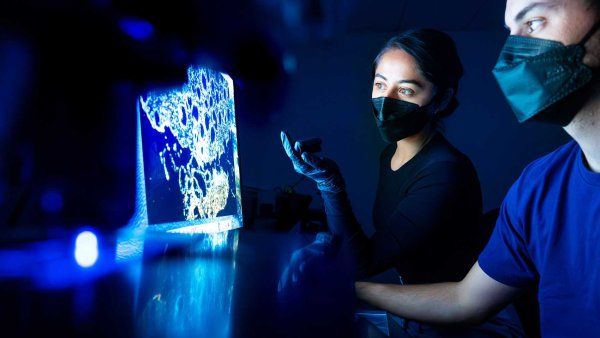
Yvonne Kapila, DDS ’90, PhD
The oral cavity is emerging as a critical entry point for the COVID-19 infection. My lab colleagues – Pachiyappan Kamarajan, PhD, and Allan Radaic, PhD – and I, in collaboration with Stuart Gansky, MS, DrPh; and Sepideh Banava, DDS, MBA, MPH, are conducting a study to evaluate the potential for oral rinses to decrease the viral load within the oral cavity.
A recent study revealed that the angiotensin-converting enzyme 2 (ACE2) receptor is thought to be the functional receptor for the virus that causes COVID-19. The ACE2 receptor is highly expressed in the nasal and oral mucosa, especially the tongue and gum tissues. The ACE2 is also highly expressed in other organ sites, including the colon, consistent with reports of GI involvement in COVID-19 infection; thus, a fecal-oral route of transmission might also be possible, in addition to the oral and respiratory route. Further, the reported altered sense of smell (anosmia) and taste (dysgeusia) in patients infected with COVID-19 may be explained by the presence of the ACE2 receptor on tongue and nasal epithelial cells that might help mediate neurotropic or neurovirulent mechanisms to modulate taste and smell pathways. Since COVID-19 may be more easily detected in saliva than on swabs from the nasopharynx, the oral cavity is a critical site for the study and prevention of COVID-19 infection.
School of Nursing
Debbie Bamberger, RNC, MS ’94, NP
I am a women’s health nurse practitioner, and I normally work for the City of Berkeley Public Health Clinic providing sexual and reproductive health care. The clinic is closed right now, so I’ve been redeployed to go out into Berkeley’s homeless encampments to screen and test people for COVID-19. Not exactly my skill set, but I am making it work and am feeling very appreciated. (I am also a current UCSF nursing student in the DNP program!)

School of Medicine
Nidia Payan, MD, Resident Alum
During the COVID-19 pandemic, I have the privilege of using my own small telemedicine company to provide free consultations to farm workers from rural underserved communities of the Central Valley. It was very rewarding to see how serving the underserved can make a huge impact. Applying my knowledge and educating them was a great experience that I will keep doing.
My company is a small, direct-to-consumer, telemedicine-only practice, focused on uninsured people in the Spanish-speaking community. We are still in the process of growing and educating about the benefits of virtual care in rural areas.
School of Nursing
Phoebe Montgomery, MS ’13, RN, CNM, WHNP
I am the principal investigator on a multi-facility study looking at the role of shared decision-making of new mothers in deciding to room in or separate from their newborn child, and longer-term health outcomes on birthing [mothers] and the infants they delivered while positive for COVID-19.
School of Medicine
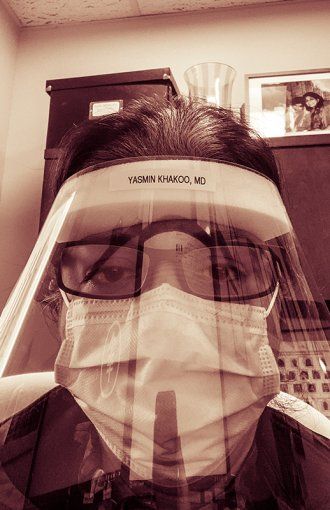
Yasmin Khakoo, MD, Resident Alum
Working as a physician in New York City, I felt guilty not being on the front lines of COVID-19. Then I realized that in non-COVID times, I take care of some of the most challenging cases: kids with brain tumors that might kill them in nine months. I felt guilty not putting my own life at stake during COVID-19, and then I realized I trained during the AIDS epidemic. I was a medical student in Harlem and accidentally stuck myself with a needle after drawing blood from a febrile woman. Too ashamed to report this, I walked around for years thinking I was a goner. During COVID-19, my own teenage daughter had fever and needed to be quarantined in our “luxurious” three-bedroom NYC apartment, and I left her meals at the door, just like we did during AIDS. She recovered and is fine, so I stopped feeling guilty and started thanking those people on the front lines, just like others did for me years ago.
PS: Since this note, I helped direct 500 N95 masks to a very underserved hospital in Harlem.