Answering the Coronavirus Hotline
UCSF call navigator Monique Posey and her co-workers field hundreds of calls a day about the pandemic.

Monique Posey, captured via FaceTime in her home office in South San Francisco on June 10 at 9 a.m. by photographer Steve Babuljak
Monique Posey thought her job doing patient outreach at UCSF was fairly straightforward. Then came COVID-19. Suddenly, she was fielding questions about the new coronavirus from hundreds of UCSF employees, patients, and community members.
In her new role as a call navigator for UCSF’s impromptu COVID-19 hotline, Posey uses protocols established by clinical experts to assess callers’ symptoms and provide them with guidance. But she quickly found out that this role involved more than giving out information. She describes how she and her team members became voices of calm and reason during uncertain times and shares some of her strategies for coping with stress.
What was your job before COVID-19?
I’ve been working at UCSF for 13 years. A year ago, I joined the UCSF Office of Population Health and Accountable Care. Our group tries to ensure that patients across UCSF’s primary care clinics come in for important screening appointments and other preventive care visits. We don’t want anyone to fall through the cracks.
What happened when the pandemic hit the Bay Area?
UCSF leadership made our telephone number the coronavirus hotline in early February. At first, we continued with patient outreach as well as answering COVID calls. But we found out pretty quickly that was not going to work. In February, we were getting 75 to 100 calls a day, but by the middle of March, we had nearly 500 calls a day. The wait time for callers then was between 30 and 40 minutes. There were four of us answering phones at the beginning, and then one of our team members went on leave, so at that point, we were only three.
Who called the hotline, and what did they ask?
Everyone was calling: staff, faculty members, patients, and students. Somehow, the hotline number was released to the general public, and so we took non-UCSF-related calls as well. The questions were all over the place: Where can I get tested? Why aren’t all UCSF employees being tested for COVID? I think my symptoms will go away soon; why can’t I work? My child has a primary care doctor at UCSF; why aren’t you testing all family members?

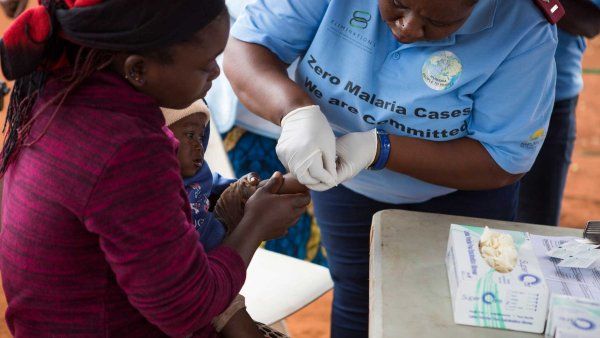
Monique Posey (bottom row, second from left) and her hotline team members served as calm voices of reason during the early days of the pandemic.
We got so many calls that we started working seven days a week. We were completely overwhelmed. For questions we couldn’t answer, we would take down the caller’s information and do the research. We gathered information from the San Francisco Department of Public Health, UCSF and Population Health leadership, human resources, and the State of California. We tried to get each caller an answer by the end of the day.
How did you handle the huge influx of calls?
Honestly, in the beginning, I had a lot of anxiety. I would see the news, and it scared me. I’m a mother. I am responsible for a home and a family. I’d have to go in to work and try to calm down the person on the phone when I wasn’t always calm myself. That was definitely a struggle.
But I learned that when I was feeling a lot of stress, I needed to take a moment and check in with myself. I would step away from what I was doing and write down how I was feeling or make time to meditate. Once I’d done that, I was open to putting myself in the next caller’s shoes. My team would also have daily huddles to talk about our feelings and work, and we had psychologists and doctors on hand whom we could ask for help.
What helped me through calls like that was empathy, finding common ground, and understanding we all were working toward the same goal of keeping everyone safe.”
What has been your most difficult call so far?
I had to tell a doctor, “Sorry, chief. You’re unable to go into that surgery with that patient because from what you’re telling me, you could be infected.” He had a hard time accepting what I was saying. He said, “What do you mean? I have to do the surgery – it’s happening in 10 minutes.” But I was just following the protocol, which said anyone who may have been in contact with another person who tested positive should stay home. What helped me through calls like that was empathy, finding common ground, and understanding we all were working toward the same goal of keeping everyone safe.
What is your work like now?
Calmer. We’ve started working remotely. And gradually, more and more people have joined our team. We now have about 35 navigators working the hotline, so we’ve been able to reduce the wait time to seconds. Our team is finally big enough that we can split up the work, take a step back, and breathe.
We’re prepared if things get worse. We know there may be a surge in the coming weeks or months. I hope not, but if there is, we’ll be here. And we’ll be here until there is no more COVID.
What motivates you?
Knowing that I work with exceptionally talented people and that we are doing our part to help. I’ve never experienced anything like this crisis. How will it end? What will the “new normal” look like? I just don’t know. Helping each other and showing compassion is the only way that we’re going to come out the other side. As for how I feel about working for UCSF, I’m definitely UCSF proud.

More from this Series
Pharmacist Katherine Yang, PharmD, raced to get a new, life-saving drug approved for emergency treatment of COVID-19.