As the parent of a bone marrow transplant patient, there are a few milestones that you long for your child to reach. Katie and Julian Drake were told that if their son Harry made it to six weeks post-transplant, he was in good shape. If he made it to six months, he was in really good shape. And if he made it to a year, well, he was golden.
Four years later, the Pediatric Blood and Marrow Transplant team at UCSF Benioff Children’s Hospital calls Harry a miracle.
The team is widely known for making miracles happen: their efforts have helped Benioff Children’s Hospital rank among the top pediatric centers in the country for higher-than-expected patient survival following bone marrow transplants. In a recent review of 156 transplant centers nationwide, the Center for International Blood and Marrow Transplant Research estimated that the median chance for survival at one year post-transplant is 63.4 percent – compared to 87.6 percent at UCSF.
Knowing Your Child Has Cancer
On Nov. 27, 2007, Harry Drake came into the world. The much-anticipated second child of Katie and Julian, Harry was so easygoing that his somewhat reserved English parents went so far as to call him an angel.
In June 2008, the Drakes felt they had finally set a foot on the ladder to the good life. They were the owners of a new home and car, and had jobs they enjoyed. Their elder son, Jack, was an energetic 3-year-old. And at 6 months, Harry was starting to sleep through the night. The Drakes celebrated one Sunday with an outing to a nearby lake, stopping at their favorite ice cream shop on the way home.
But as Katie uploaded photos from the day to her computer that night, one picture in particular caught her eye: a shot of Harry with an odd bump on his head, about the size of a quarter and shaped like a horseshoe.
Bumps and bruises on Harry weren’t new. The day he was born, they noticed a bruise on his face and another on his forehead, but his doctors thought they were birthmarks. Over the next few months, he developed other bruises. A dermatologist diagnosed him with a harmless skin disorder that would likely clear up by the time he reached his first birthday.
The picture from that Sunday told an undeniably different story, however. Katie emailed it to her new pediatrician, who asked her to bring Harry in the next day. After a week of appointments and tests, on Friday, June 13, the Drakes received his official diagnosis: acute myelogenous leukemia, or AML.
“Knowing your child has cancer is bad enough,” says Katie. “Then finding out it’s a rare type, then an aggressive type. Then learning it has spread into his cerebrospinal fluid, he has a 50/50 chance of survival, and the treatment you’re about to put him through is very toxic. It was devastating news.”
Harry started chemotherapy that day.
When the pediatrician told Katie to pack her bag for the hospital, she brought enough for one night. “I had to laugh because I packed just a toothbrush and a pair of underwear for me, but for Harry, I packed all these baby clothes. The irony was that he spent the next six months in mostly a hospital gown.”
After five weeks at the hospital where the Drake boys were born, California Pacific Medical Center (CPMC), Harry finished what became his first round of chemotherapy. Two days later, the Drakes learned that although the cancer in Harry’s blood was in remission, cancer cells remained in his spinal fluid. He was classified as a relapse, and his chances of survival decreased to 20 percent. The only way he might make it was by receiving a bone marrow transplant – and there was no better place than UCSF.
Factors for Success for Bone Marrow Transplants
A bone marrow transplant can be a lifesaving treatment for children with cancer, like Harry, as well as diseases of the immune system, aplastic anemia, inherited diseases of the bone marrow, and some metabolic diseases.
Bone marrow is the spongy substance found in the center of bones. It manufactures bone marrow stem cells, which produce red blood cells, platelets, and white blood cells. Red blood cells carry oxygen to tissues in the body, platelets help blood to clot, and white blood cells fight infections.
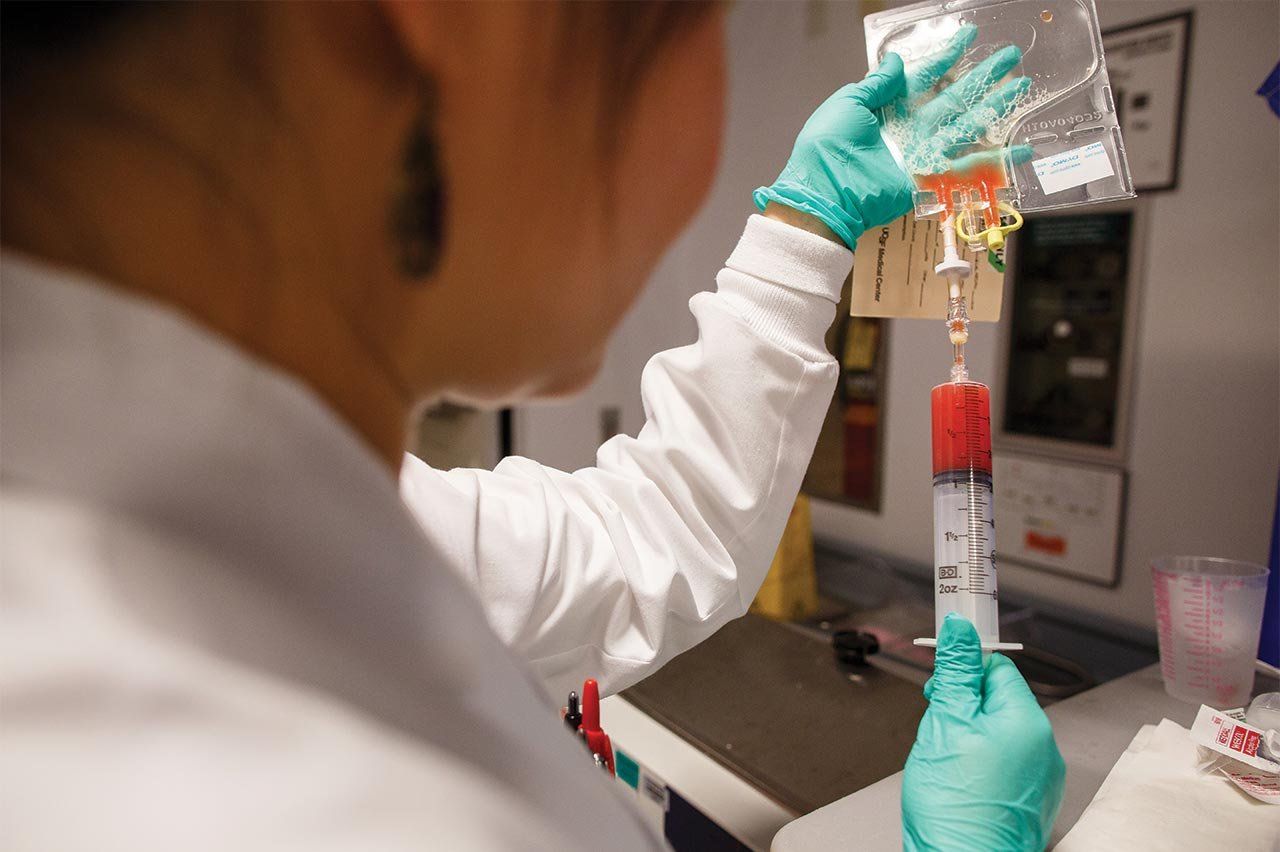
Unlike solid organs, which can be transplanted in their entirety, it’s not possible to extract all of the marrow from every bone in a patient’s body. Instead, the existing marrow is killed with extremely high doses of chemotherapy, often followed by radiation. It’s then replaced with healthy marrow, injected into the bloodstream through an intravenous tube. Within two to three weeks, the new marrow begins to grow inside the recipient’s bones.
The Pediatric Blood and Marrow Transplant Program at UCSF was established in 1982 by immunologist Mort Cowan, MD, now the chief of the Allergy, Immunology, and Blood and Marrow Transplant Division. Since then, nearly 1,000 bone marrow transplants have been performed at UCSF, at an average of 50 to 60 per year.
Cowan attributes the program’s 87.6 percent one-year survival rate to three main factors: a multidisciplinary team, dedicated to bone marrow transplant; the team’s ability to be highly selective with donor matching; and their constant influx of research and clinical innovations.
UCSF’s Multidisciplinary, Dedicated Team
Cowan has built a team of more than 20, including physicians – a variety of hematologists, oncologists, and immunologists – nurses, nurse coordinators, social workers, child life specialists, nutritionists, pharmacists, a donor program coordinator, and lab technicians. All are dedicated to treating not only bone marrow transplant patients, but also their families.
“The family is so involved,” says Cowan. “You can’t take care of the patient without the family, without the parents. Over time, you become more and more sensitive to families’ concerns – and all the more committed to their care as a result.”
That commitment couldn’t have been more needed than it was by the Drakes. When they first met with Biljana Horn, MD, medical director of the Blood and Marrow Transplant Program, she told them Harry’s chances could be as low as 10 percent. Katie and Julian debated whether or not to proceed with a bone marrow transplant.
They sought a second opinion from an AML expert at Stanford. He confirmed their options: take Harry home and just love him until he passed away, or put him through further grueling rounds of chemotherapy and a bone marrow transplant.
Cowan, a member of the UCSF Helen Diller Family Comprehensive Cancer Center, told the Drakes he wouldn’t allow them to proceed with the transplant unless they were both in full agreement. After much agonizing discussion, they decided to go for it. “I didn’t want to look back and wonder: what if we had given him the transplant?” says Katie.
To prepare Harry, his cancer had to be in full remission, meaning more chemotherapy at CPMC, which thankfully proved successful. The Drakes checked into UCSF on Oct. 6, 2008, 10 days before transplant.

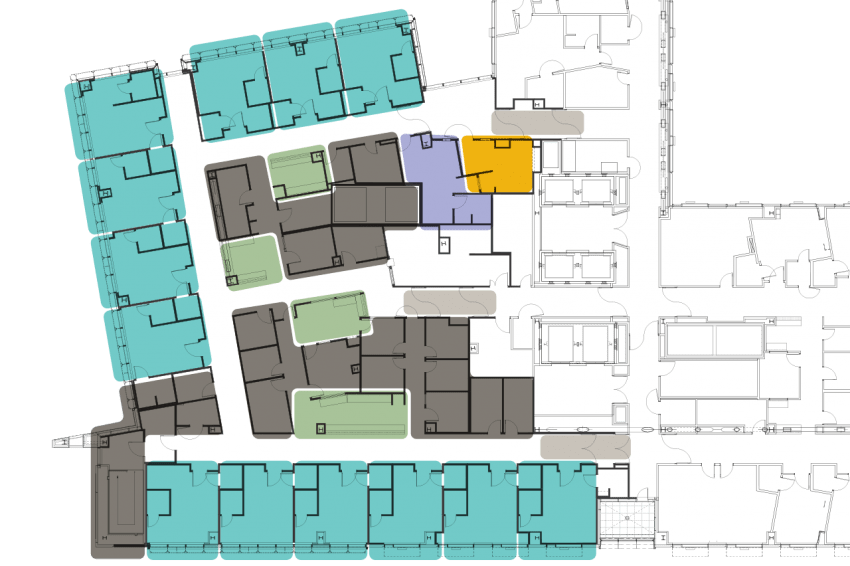
Future UCSF Benioff Children’s Hospital. Rendering: Stantec
The bone marrow transplant (BMT) unit at UCSF Benioff Children’s Hospital sits behind a set of double doors in a positive pressure, high-efficiency, particulate air-filtered environment. That means when a door opens, instead of air flowing into the room, air flows out. The design is crucial to kids like Harry, who lack immune systems when they’re in the unit.
Each of the patient rooms is located off of an anteroom, where doctors, nurses, parents, and visitors must scrub up before entering. Patients cannot leave their rooms during the bone marrow transplant process, except for an occasional scan in another part of the hospital. At that time, a nurse carefully covers the patient in a sheet and escorts him or her to an elevator shared with no one else.
In the BMT unit at the new Benioff Children’s Hospital at Mission Bay – part of a state-of-the-art hospitals complex that will include women’s and cancer hospitals – a sophisticated design will allow patients to leave their rooms and walk unit floors. The new UCSF Medical Center at Mission Bay complex will open its doors in 2015.
New Bone Marrow Transplant Unit
In the BMT unit at the new UCSF Benioff Children’s Hospital, opening in 2015:
Special entries will protect filtered air, letting patients walk unit floors
Patient rooms (with two bathrooms) will be big enough for families
Specialized play therapy space will let patients and siblings interact
A family lounge will give parents a nearby place to unwind
Nurses will be stationed around every corner
Consult rooms and more support space will be on hand
Katie and Julian took turns spending 24 hours a day, seven days a week in Harry’s hospital room. “We couldn’t leave because of the need for isolation,” Julian reflects. “We had a beautiful view of the bay, and I watched the Blue Angels air show through the window. I remember looking down and seeing all the mountain bikers meeting at the corner of the street, ready to go for a ride. Life was going on without us.”
The parent not at the hospital stayed home to care for 3-year-old Jack, who couldn’t understand what was happening to his younger brother. Katie and Julian hadn’t even had a chance to explain it to him. “I was afraid of crumbling in front of Jack,” remembers Katie. “So I just put on a happy face for him, even though my thoughts were also with Harry.”
Because Jack was under age 12, he wasn’t allowed to visit Harry in the hospital. On one or two occasions, he came just to wave to his brother through the window on the door of the anteroom. “It was heartbreaking to see how much joy Jack brought to Harry, even through the glass,” says Katie.
Selective Donor Matching
Bone marrow transplant patients spend the 10 days from check-in to transplant undergoing a conditioning regimen: chemotherapy and possibly radiation therapy to kill their existing bone marrow cells and immune system, preparing their bodies to receive and accept the healthy donor marrow.
This acceptance is based largely on whether the donor and recipient cells think they’re the same – the likelihood of which can be gauged by comparing 10 genetic markers, known as human leukocyte antigens (HLAs), in the donor and patient. In general, the better these markers match up, the better the chance of marrow acceptance.
For Harry and every other child who receives a bone marrow transplant, there are several possible donor options. Allogenic transplant – cells from another person – is the option used most frequently to treat diseases requiring transplant in children. Siblings are usually the best allogenic donors, since they have a 25 percent chance of being identically matched with the patient for all 10 HLA genetic markers.
When an HLA-matched sibling isn’t available, alternative donors are sought, typically from among unrelated volunteers or the umbilical cord blood units of healthy babies that have been stored in special cord blood banks. While this option is used for an average 40 percent of children, it’s not without obstacles: the search for these donors can take many months to complete and not everyone will have a match.
Cowan’s team specializes in another, less common type of alternative donor – a relative (often a parent) who’s only a half-match with the patient. To achieve success in these transplants, Cowan’s lab enriches the donor’s marrow stem cells while removing potentially harmful T lymphocyte cells that can cause a fatal reaction in the recipient called graft versus host disease.
For a minority of cancers, an autologous transplant can be performed, in which the patient’s own bone marrow stem cells are extracted before a final round of marrow-killing chemotherapy and are then re-infused at the time of transplant. Since his was a cancer of the bone marrow itself, Harry was unable to have an autologous transplant; his brother wasn’t a match, either. But a match was found – in an unrelated 25-year-old German miller who chops wood and raises sheep and goats for a living.
Transplant day fell on Oct. 16. At 1:32 p.m., the donor’s peripheral blood stem cells trickled into Harry. “It was such a small amount of fluid,” Katie remembers. “But so beautiful – a watermelon pink color.”
The transplant lasted just 28 minutes. Katie recalls, “When it was over, I was like, ‘That’s it?’” – a very common reaction for families, according to BMT social worker Anu Sood. The day after the transplant, Katie says, she and Julian thought: “Oh my God, we’ve done it. Now we have to live with what we’ve done.”
Research and Clinical Innovations
Perhaps the hardest part is what loomed next: side effects of chemotherapy and the transplant.
Chemotherapy targets rapidly dividing cancer cells, but because the cells in hair, mouths, and intestinal tracts also divide quickly, chemotherapy tends to kill them as well. The result can be hair loss, stomach sensitivity, and mouth sores.
Harry suffered from the latter while receiving his second round of chemotherapy. With a bad case of mucositis, he was on so much pain medication that he lived in a deep sleep for his entire eighth month. When he did come to, he threw up mucus so long and thick that Katie could wrap it around her hand multiple times.
Following his transplant, Harry’s side effects once again included mucositis – although fortunately not to the same degree – fevers, a staph infection, a strep infection, and a whole host of other issues. He also had to endure multiple blood transfusions.
Cowan and Horn have long been troubled by how the toxic effects of transplant regimens impact patients like Harry, and have spent the past 15 years studying ways to reduce them. Along with hematologist/oncologist Chris Dvorak, MD, they recently completed a trial using a combination of chemotherapy drugs that were less toxic and yet still effective. The trial was quite successful, benefiting multiple patients (including Harry).
Yet for recipients of less compatible, unrelated-donor grafts, the reduced toxicity of these drugs was associated with an increased chance of rejection. Dvorak has since developed a new approach, currently in trials, that will maintain reduced toxicity while overcoming the risk of rejection. In another trial, Horn is working to augment the chemo regimen by detecting the risk of relapse and harnessing the patient’s own immune system to attack the malignancy.

June 8, 2008: Family outing. Five days later, Harry would be diagnosed with leukemia. Photo: courtesy of the Drake family

August 2008: Receiving chemotherapy. Surrounded with baby toys, Harry preferred to fiddle with medical equipment. Photo: courtesy of the Drake family

September 2008: At their weekly meeting, Mort Cowan and the pediatric BMT team discussed Harry’s case. Photo: Steve Babuljak
October 16, 2008: Transplant day. Two years later, the Drakes asked the donor why he did it. He replied, “To save someone’s life.” Photo: Steve Babuljak

November 2008: “I kept thinking, one in 10 survive AML,” says Katie. “My mom said, “Somebody has to be the one in 10. Why not Harry?’” Photo: courtesy of the Drake family

December 2008: Harry leaves his room for a quick drive through the BMT unit. “To be able to leave that room was such a blessing,” says Katie. Photo: courtesy of the Drake family

March 2009: The dressings for Harry’s broviac catheter, which he wore from the day of his diagnosis until seven months post-transplant, had to be changed daily. Photo: courtesy of the Drake family

June 2012: The Drake family at home three-and-a-half years post-transplant. “At this stage, I am not worried,” says Katie. “We know that we have other issues, but the fact that he is here is more than enough and will always be.” Photo: Steve Babuljak
Life Post-Transplant
A typical stay in the BMT unit lasts six to eight weeks. When the Drakes weren’t released in time for Harry’s first birthday on Thanksgiving Day, Katie prayed they’d be home for Christmas to see Jack open his presents in front of the tree. They finally checked out on Dec. 23, 11 weeks after checking in.
Four years later, the only residual sign of Harry’s ordeal is that he resists feeding himself, a frequent problem for children who undergo a bone marrow transplant at such a young age. Harry had received nourishment through an IV or feeding tube from the time he was six-and-a-half months, so by the time he was released at more than a year old, he’d forgotten how to swallow and hadn’t yet learned to chew. He has since learned to do both.
Two days a month, a cognitive behavioral therapist visits the Drake home to help Harry learn to eat. It’s a slow process, but Katie and Julian have set a goal that seems easy to reach considering all they’ve achieved: they hope to see Harry feed himself when he enters kindergarten next year.
Aside from his eating challenges, Harry is a happy, active, carefree boy. Watching him splash through the creek at the neighborhood park, you’d never guess that he once had a 10 percent chance of survival. That his life was saved with a bone marrow transplant at UCSF. That he is a miracle.