Cindy was cradling her 9-month-old son, Elias, against her chest when she and a room full of family simultaneously yelled “Surprise!” to an unsuspecting aunt on her birthday. The outburst shot like a bolt of electricity through Elias. He cried for an hour.
Xander, while growing up in the perpetual sensory assault of Manhattan, had to get off the train any time someone with a guitar entered his subway car to play for small change.
Cal had a more enigmatic reaction to stimuli. His mother, Jennifer, points to the floor-to-ceiling windows in her hilltop living room. Rooftops, forests, and the San Francisco Bay spool out for miles. Cal was 2 when they moved here from a small, contained apartment. “We got here and Cal was always running away from me,” recalls Jennifer. “He suddenly had all this space and stimulation. He was in sensory overload.”

When Cal (with his mom, Jennifer) first moved to the suburbs from the city, “he was in sensory overload,” she says. The treatment framework for SPD developed by UCSF neurologist Elysa Marco is helping parents control their children’s arousal levels. Photo: Gabriela Hasbun
Beyond Nails-On-A-Chalkboard
Elias, Xander, and Cal all experience extreme reactivity to tactile, auditory, or visual stimulation – a condition known as sensory processing disorder (SPD). Tactile triggers that torment kids with SPD include tags in shirts, wooly sweaters, socks, or an accidental shoulder brush during preschool circle time. Auditory offenses include coffee grinders, the birthday song – surprise or not – and noisy, erratically moving toys. Visual provocations that can set kids off include IMAX movies, crowded stadiums, parking lots, even bikes and tents hanging from the ceiling of a camping store. Whether seen, heard, or felt, what all these sensory inputs have in common is their sudden onset and unpredictability.
For an SPD kid, these experiences are beyond a nails-on-a-chalkboard annoyance. “As soon as these kids can move themselves, they will run screaming from the room when these stimuli reach their world,” says Elysa Marco, MD ’00, a cognitive and behavioral pediatric neurologist at UCSF Benioff Children’s Hospital San Francisco and a member of the UCSF Weill Institute for Neurosciences. Take Xander, who is now 14. He would rather be kicked in his hapkido martial arts class than receive a friendly hug. “It physically hurts when people hug me,” he says. This makes his mom, Judy, who is a hugger, think twice before reflexively going in for a hug. And Elias, at age 2, would hold his breath and sit at the bottom of the pool – the silence and water pressure his only solace.
Living in a state of perpetual flight, fight, or freeze in reaction to stimuli – or in constant fear of those reactions’ onset – takes a toll on SPD children and their parents alike. The disorder can be profoundly disruptive on every level. As a parent, how do you diaper a child who feels abraded by even a cloth diaper? And if you can’t diaper a child, how do you leave the house, much less go to work? As a preschool teacher, how do you manage a student who falls apart every time a block falls or a tambourine is tapped? And as that student, how do you connect with your classmates when you feel compelled to dart under a table to save yourself from that tumbling block or terrifying tambourine?
But as life-altering as SPD is for the children and families affected by it, the disorder isn’t included in the Diagnostic and Statistical Manual (DSM), clinicians’ touchstone for diagnosing psychiatric conditions. Marco’s professional quest is to build a better understanding of the genetics and the neural underpinnings of sensory-processing differences. It’s clear that sensory overresponsivity is shared by many children with genetic or psychological conditions like autism and attention-deficit/hyperactivity disorder (ADHD). Indeed, kids with SPD often struggle with more than hypersensitivity: Some 40 percent of kids with an SPD diagnosis also have dysgraphia, meaning they have such poor fine-motor coordination that they have difficulty writing, and 40 percent also have ADHD (these are not necessarily the same 40 percent). While Marco isn’t hung up on labels, she is committed to achieving better understanding and better therapeutic support for children with sensory-based challenges. She’s encouraged by signs that the field is moving past the DSM debate to a more genetic and symptom-based approach to caring for such kids – in their homes, schools, and communities.
According to Marco, who is also an associate professor of neurology at UCSF and a resident alumna, many SPD kids acquire an autism label along the way, which helps with insurance coverage. And there is overlap in the disorders. Nearly 90 percent of kids with autism also have sensory processing differences – some underresponsivity and some overresponsivity. However, kids with SPD do not usually exhibit the fixated interests, repetitive motions, and social indifference that are hallmarks of autism. “Kids with SPD are wanting to socially engage, they just can’t tolerate it,” explains Marco.
Diagnostic Debate
Early in her practice, Marco kept seeing kids with what were described as developmental delays; they often had autism diagnoses, too. “I would want to ask these parents about seizures, walking, and language development, but they wanted to know how they were supposed to wash their kids’ hair when they couldn’t touch their head, or how they could just get them clothed and out the door,” recalls Marco.

Elysa Marco, MD ’00. Photo: Elena Zhukova
A distinct SPD diagnosis is not without controversy. Some neurologists and pediatricians think SPD is listed exactly where it should be – under autism. Others argue that the condition doesn’t exist at all; for years, clinicians attributed SPD to inadequate parenting. Indeed, every parent of an SPD child has stories of being judged for their parenting by clinicians, loved ones, and strangers alike. “I take Cal to places like a restaurant or party where the volume rises. He just loses it – both imploding and exploding. Or in parking lots, he’ll just sit down,” says Jennifer. “In these scenarios, we always get comments basically indicating that we are obviously not doing this whole parenting thing very well and that with more discipline and authority, his behavior would change. Honestly, I thought that initially, too. And my confidence as a parent went way downhill.”
Instead, Marco believes, sensory differences should be regarded as a function of brain structure and brain activity that’s guided by both genetic and environmental influences.
Indisputable Evidence
Marco’s practice is now spilling over with SPD kids like Elias, Xander, and Cal. She also has a significant social media presence on a Facebook page devoted to sensory processing disorders. Her contributions there resonate with the page’s 85,000 members, who are desperate for answers about their children’s seemingly bizarre reactivity. And in her lab, she is scientifically validating the life experience of SPD patients by identifying their brains’ unique structure and function and their distinct genetic profiles. Marco and her team have done so with great success by leveraging leaps in imaging technology and cross-disciplinary partnerships.
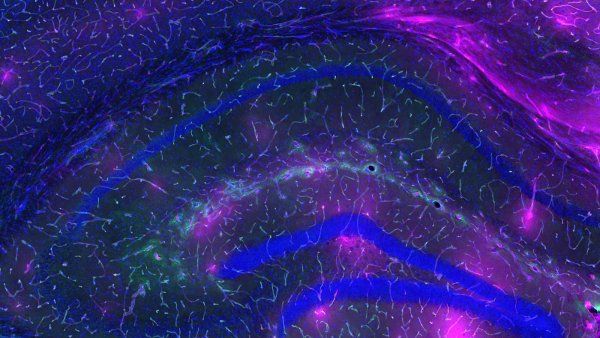
Her lab’s first research breakthroughs were back-to-back papers, published in 2013 and 2014 with UCSF radiologist Pratik Mukherjee, MD, PhD. In the first one, Marco and Mukherjee performed brain-imaging studies on kids with SPD, primarily boys, and compared them against typically developing boys. In the SPD kids, they found abnormal tracts in their white matter, a part of the brain that’s essential for perceiving, thinking, and learning. These tracts connect the auditory, visual, and tactile systems involved in sensory processing. It was the first time researchers had identified a biological basis for SPD.
In the second study, they compared structural communications in the brains of boys with SPD and boys with autism. They visualized connections among neurons by tracking water moving through the brain’s white matter. When water molecules move in the same direction, connections are thought to be directional and strong, while water going against the flow is a sign of faulty connections.
These kids are not breaking down in school because their parents are doing a bad job or because they are bad kids. Their brains are wired differently.
“The data was so clear. Kids with sensory processing differences just have different degrees of connection efficiency, particularly in the back part of the brain,” says Marco. This study was the first to show that kids with SPD have quantifiable and distinct differences in brain function. “These kids are not breaking down in school because their parents are doing a bad job or because they are bad kids,” says Marco. “Their brains are wired differently.”
Marco’s research and social media outreach is now arming parents, teachers, and clinicians all over the country – many of whom had never heard of SPD before – with the tools to diagnose and deliver help to kids earlier. The papers are also a wake-up call for neurologists, pediatricians, family, and friends who have questioned the disorder’s existence – a bittersweet validation of what parents of SPD kids already knew. A diagnosis that stands on hard scientific ground gives parents authority to explain rather than apologize for their kids’ behavior. But more importantly, it gives them license to forgive themselves – to say “I am not crazy,” as Elias’s mom, Cindy, puts it. “And this is not my fault.”
A Four-Part Framework
That scientific confirmation has shifted the conversation to finding viable treatments. Marco has developed a four-part framework for building a safe, positive world in which SPD kids can thrive. The first two elements – controlling kids’ environment and arousal – help parents figure out how best to structure their children’s physical and emotional surroundings. The third helps kids master healthier reactivity behaviors through brain training. The last helps kids achieve calmness through medications that soften the blows of overstimulation.
“First, I encourage parents to get an occupational therapist,” recommends Marco, “to help them figure out both at home and at school what environmental changes need to be done to make their lives quiet and consistent. Because it’s the novel stuff that unseats them.” At home, that can be as simple as organizing their room. At school, it can mean putting tennis balls on the legs of chairs so they don’t make sudden sounds as kindergarteners squirm.
Some schools are more accommodating than others, and parents may find that out the hard way. Kids might be asked to leave a school, or parents might pull them out. “About 25 percent of the kids in my clinic end up in independent schools,” says Marco. Cal is in a small and very structured early intervention program, offered through the public school system, that has been incredibly effective in helping him understand the expectations of a school environment. Other SPD kids, like Xander and Elias, are schooled at home, either online or by teachers who come to them. Marco’s biggest takeaway on school choice is this: You don’t want your child to have post-traumatic stress from a school environment that can’t accommodate them. “Whether your kid is 3, 12, or 18, you need their self-esteem intact,” she says.
Her treatment plan also calls for a healthy diet free of simple sugars and simple carbs, a regular bedtime, and consistent exercise, all of which help control the arousal levels of kids – and parents. “If parents are out of control, their kids will be. As a simple start, I suggest they take 10 deep breaths if their kids start to escalate.”
Brain Training
Typically, kids with SPD have weekly occupational therapy sessions that focus on gross motor skills, as well as fine motor skills for those with dysgraphia.
“It is amazing to me to see how really smart kids with terrible handwriting get crushed by school,” says Marco. “On a short-answer test you may know volumes but fail because writing a single sentence is torture.”
The Neuroscape Lab is developing video games to treat a wide range of conditions, including ADHD, Autism, and Sensory Processing Disorders.
Programs that work on cognitive control or attention are also critical for SPD kids who have ADHD in addition. Marco has partnered on this front with Joaquin Anguera, PhD, director of the clinical program at Neuroscape, UCSF’s translational neuroscience center. They are addressing cognitive control deficiencies with a new video gaming platform called Project EVO (developed by Akili Interactive Labs, a UCSF startup). On EVO, kids navigate a character along a winding path, avoiding obstacles and responding to variously colored targets. It’s designed to strengthen the brain’s ability to process and prioritize thoughts and external stimuli, and the game gets harder as a player gets better at it. “Playing EVO actually made a difference in issues of inattention that we measured in the lab and that were reported by parents,” says Anguera, who is also an assistant professor of neurology and psychiatry. “We showed a significant change in the kids’ neural activity. These changes were really deep, and they persisted for nine months beyond the eight-week intervention.”
Though medication is the therapy of last resort, it can be crucial. Marco prescribes beta blockers, which dampen kids’ reactivity, particularly to touch. It’s been a game-changer for Xander. “It has really helped,” he says. “I don’t feel nearly as much pain if someone hugs me. But I’ll still never be a huggy person.” Judy is thrilled. “I remember Xander saying when he was little, ‘I wish I could get a jacket, like a bubble jacket, because then I could just walk around and people could hug or brush up against me and it wouldn’t hurt.’ Well, with this drug, he’s finally found that layer of protection.”
New Therapeutic Targets
Anguera and Marco are currently doing a feasibility study of Neuroscape’s Body-Brain Trainer (BBT), a video game for kids with ADHD, some of whom also have SPD. To play BBT, kids are hooked up to a heart monitor and put in front of a large-screen TV. They’re then directed to touch an image that flashes onto the screen. “We designed BBT to see if cognitive and physical training lead to synergistic effects on cognition, so that one plus one equals seven with respect to cognitive control abilities,” explains Anguera. They hope this will be the case for kids with SPD who struggle with attention issues.
Marco is also poised to publish a study with Elliott Sherr, MD, PhD, a fellow pediatric neurologist and resident alumnus. This study looked at whether the genes involved in SPD are the same as or different from those involved in autism; neurogeneticists have uncovered 76 genes that contribute to autism. Marco and Sherr found that kids in Marco’s clinic have an enhanced number of changes in these genes. “And so do their parents,” adds Marco, who was initially uncomfortable sharing that finding with the parents. But it turned out that few were surprised, given their own life experiences or observations of their spouses’. “We’ve also found that 18 percent of our kids have an identifiable genetic difference that is distinct from autism,” she says.
Knowing SPD’s structural, functional, and genetic underpinnings provides Marco and her team with both new therapeutic targets and new ways to measure the success of their therapies. Her goal is to understand the relationship between the differences in SPD kids’ brains and their autonomic nervous systems – the part of the nervous system that controls respiration, digestion, the heartbeat, and the fight-or-flight response, which, in SPD kids, can feel like their resting state.
“We’ve already shown that just eight weeks of training with EVO can change the ring of neurons in the brain,” says Marco. “These kids’ brains are continually changing through the course of their childhood. If we can keep them in positive environments and train their brains to change in positive ways, we can help them adapt.”
With a combination of medication, online schooling, and a deep sensitivity to Xander’s needs, Judy has helped him strike a balance between controlling his environment and integrating with society. He is educated at home, at a pace and in a space tailored to his needs, but he interacts with like-minded kids at large, organized meet-ups. He is now gearing up to apply to MIT.

“We are stuck in the heartbreak of what to expect and what to let go of,” says Jennifer. “Will he make friends? Does he want to? Will he be happy?” Photo: Gabriela Hasbun
Jennifer and Cindy – also exquisitely attuned to their sons’ sensitivities – are still in the thick of it, and their paths forward are less clear. Elias, like Xander, has found great relief from medication that calms his reactivity. He, too, is being taught at home, by teachers who come to him. He still seeks physical solace through near-perpetual motion. “One morning he woke up in a terrible mood,” says Cindy. Knowing he needed motion, she handed him a pogo stick and started counting. It took 413 jumps to calm him. Her advice to other parents is this: “The only way you are going to get through is to find other families – I say women, because for me it has been moms – who are going through the same thing. Because there is nothing like having a friendship with somebody who gets it.”
Cal is just three and a half and goes to two different schools – one very structured, the other a Montessori school and more experiential. The Montessori kids all know Cal’s name, but he doesn’t know theirs. They run toward him and he runs away, pretending he’s king. It’s a game he plays surrounded by other kids, but essentially alone. “We are stuck in the heartbreak of what to expect and what to let go of,” says Jennifer. “Will he make friends? Does he want to? Will he be happy?”