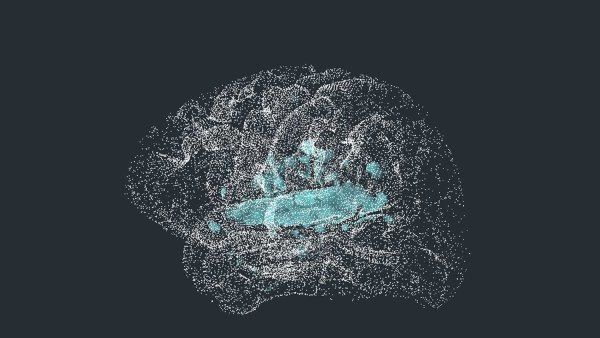
When Daniel Gibbs, MD, enrolled in an Alzheimer’s study at UC San Francisco almost a decade ago, researchers needed access to a secure government facility just to confirm that he had the disease. They summoned Gibbs to the Lawrence Berkeley National Laboratory, hooked him up to an IV, and wheeled him into a donut-shaped machine called a PET (positron emission tomography) scanner. Then they waited.
In a building next door, radiochemists fired up a cyclotron, a huge contraption equipped with powerful magnets. The magnets spun tiny particles faster and faster, ultimately creating a nuclear reaction that produced radioactive molecules known as tracers. The tracers were designed to safely detect markers of Alzheimer’s in the brain. But soon after they were created, the molecules would begin to decay. So they had to be transported to Gibbs immediately.
The radiochemists placed the time-sensitive cargo in a plastic cylinder the size of a large soda bottle and sent it hurtling through a network of pneumatic tubes. The cylinder arrived in Gibbs’ room with a loud “woosh” and a “thud.” The UCSF researchers quickly extracted the tracers and transferred them into his IV tube. “It was timed down to the second,” recalls Gibbs, a retired neurologist who, ironically, had spent his career caring for patients with Alzheimer’s. “They had stopwatches running.”
The tracers traveled through Gibbs’ bloodstream into his brain, where they latched onto abnormal proteins that are characteristic of Alzheimer’s disease. Only then, using the PET scanner, could the researchers peer inside the black box of his brain. On the scans, clusters of the tracers lit up like constellations.
At the time, the test Gibbs received was cutting edge – and heralded by many in the field as a tantalizing glimpse of the future of Alzheimer’s diagnostics. For decades, the only way for a family to know for sure if their loved one had the disease was by having their brain autopsied after they died. PET scans allowed physicians to bring certainty to patients during their lives.
But even today, few people suspected of having Alzheimer’s ever receive such testing. Although longer-lasting and more convenient tracers exist today, PET scans still come with financial and logistical hurdles. Neither Medicare nor Medicaid will pay for Alzheimer’s scans, which cost upward of $5,000 a pop. And patients often must travel to major cities to get them. (Biomarkers of Alzheimer’s can also be detected in spinal fluid – a less expensive test but one that requires a lumbar puncture, which is uncomfortable and invasive, so many patients choose not to get one.)
Scientists may have finally found a way to overcome these limitations. In 2020, researchers at UCSF and elsewhere unveiled several groundbreaking studies of a new, highly sensitive blood test developed in the labs of the pharmaceutical company Eli Lilly. The studies demonstrated that the test could detect tiny concentrations of Alzheimer’s-associated proteins in patients’ blood with remarkable accuracy, even before the onset of cognitive symptoms. Since then, other research groups have announced additional promising blood tests for the disease. Experts say the U.S. Food and Drug Administration (FDA) could approve the first of these tests by the end of the year.
Blood tests are less expensive than PET, less invasive than a lumbar puncture, and easy to use, which means they likely will become far more widely used than the other diagnostic options. The early versions now go for around $1,200 to $1,500, about a quarter the price of a PET scan, and the cost should fall as the market expands. Many experts are optimistic that a boom in accessible Alzheimer’s tests could enable new insights into the disease, speed the development of new treatments, and radically improve patient care. More patients could learn – as Gibbs did – that their brains harbor signs of Alzheimer’s disease as early as 20 years before cognitive troubles start.
But these advances also raise vexing questions. What does it mean if you test positive for Alzheimer’s biomarkers but have no symptoms? How certain is it that you will develop the disease? Should you try new medications that could slow its progression but might also cause serious side effects? Would you want to know that you could one day face a devastating illness for which there is currently no cure?
Worth a Thousand Words
In 1901, a 51-year-old woman named Auguste Deter walked into a German asylum with a variety of strange symptoms, including memory loss, paranoid delusions, agitation, problems with sleep, and mental confusion. “I’ve lost myself,” she remarked before she died four years later, according to the records of her doctor, Alois Alzheimer, MD.
After Deter’s death, Alzheimer autopsied her brain. He noticed that the thin outer layer, or cortex, was shrunken. And when he examined slices of it under a microscope, he saw dark clumps of sticky “plaques” and stringy “tangles” in and among the nerve cells. These plaques and tangles would come to be recognized as the hallmarks of Alzheimer’s disease.
But the problem of how to spot them in living patients stymied the field for almost a century. Without definitive diagnostic tests, the elderly were condemned to maddening uncertainty: Were flashes of forgetfulness or confusion just “senior moments” or signs of impending precipitous decline?
Even patients clearly suffering from dementia were often misdiagnosed. Clinicians had trouble distinguishing between Alzheimer’s and other brain disorders with similar cognitive symptoms, such as frontotemporal dementia and atypical parkinsonism. This made it difficult for doctors to adequately advise families and likely confounded the results of many early drug trials. (Between 1998 and 2017, pharmaceutical companies made 146 unsuccessful attempts to develop Alzheimer’s medicines.)
In the early 1980s, scientists identified the key proteins comprising plaques and tangles: amyloid beta and tau, respectively. By the next decade, they had shown that these compounds were detectable in spinal fluid using a lumbar puncture, also known as a spinal tap. And in 2004, radioactive tracers like those used on Gibbs, which made it possible to see Alzheimer’s proteins on a PET scan, made their debut.
Gil Rabinovici, MD, who began a fellowship in memory disorders at UCSF’s Memory and Aging Center a year later, recalls how exciting it was to observe the brain “at a molecular level” in order to diagnose a disease that, according to what he’d learned in medical school, could only be revealed after death. The Memory and Aging Center, which was then emerging as a national leader in research and care of Alzheimer’s disease and other causes of dementia, was one of the first places in the country to adopt PET technologies. In the clinic, Rabinovici saw how valuable these tests could be for patients.

“They say a picture is worth a thousand words,” he says. “As much as patients respected our expert opinions, seeing the scan results with their own eyes really made all the difference in the world. It ended their quest for a diagnosis and allowed them to move toward thinking about next steps.”
That was certainly true for Gibbs. Before undergoing the PET scan, he had taken a genetic test and learned he was carrying two copies of a gene that placed him at extremely high risk of developing Alzheimer’s disease. Suddenly, every misplaced key, forgotten name, or other mental stumble began to take on dark undertones. He found the ambiguity maddening. But then, at age 63, he found himself staring at his own brain on a conference room screen. The tissue, rendered in black and white, was shot through with clusters of red and yellow, highlighting areas where the radioactive tracers had found and bound to amyloid plaques.
Receiving a clear-cut answer was a life-changing relief. “The diagnosis gave me some certainty about what I was dealing with and going to have to deal with more in the future,” says Gibbs, who detailed his experience in a 2021 book, A Tattoo on my Brain: A Neurologist’s Personal Battle against Alzheimer’s Disease. “It allowed me to focus on the disease and how I could lower the impact of it and plan for the rest of my life.”
The diagnosis gave me some certainty about what I was dealing with.”
In 2016, Rabinovici, who now specializes in PET imaging and is UCSF’s Fein and Landrith Distinguished Professor of Memory and Aging, helped launch a massive study of PET tests called Imaging Dementia: Evidence for Amyloid Scanning (IDEAS). Still ongoing, the study aims to enroll 25,000 Medicare beneficiaries with mild cognitive impairment or dementia at hundreds of clinical sites across the country to determine whether amyloid PET scans improve patient care and outcomes. The results to date, Rabinovici says, are unequivocal: The scans have had a “profound impact on diagnosis and patient management.”
In an analysis of 11,000 IDEAS participants published in 2019, Rabinovici’s team found that about a third of patients who got PET scans had previously received wrong diagnoses; after the tests, clinicians switched their diagnosis from Alzheimer’s disease to a non-Alzheimer’s cause, or vice versa. For more than 60% of patients, the tests also led to changes in care, such as new drug prescriptions or counseling. Unpublished data from IDEAS has even demonstrated a modest impact on medical outcomes, including a 4.5% reduction in hospitalizations, Rabinovici says.
The study is now in a second phase called New IDEAS, which focuses on reaching populations, such as Black and Latinx communities, that have been historically underrepresented in Alzheimer’s research. Initial data suggest that patients from these groups are less likely than white patients to test positive for amyloid plaques on PET scans. This implies that for such patients, conditions other than Alzheimer’s, such as cerebrovascular diseases, may play a larger role in the development of dementia.
“In dementia care, we’ve been diagnosing people based on symptoms of memory loss or other cognitive changes,” Rabinovici says. “But if we’re going to make progress in treatment and prevention, we need to understand the biological underpinnings that are driving their symptoms.”
Bloodwork Breakthroughs
For early adopters like Rabinovici, the advent of PET scans underscored the importance of biomarker testing for Alzheimer’s disease. But experts were unable to solve the technology’s accessibility problem.
Blood tests have always been an obvious answer. Scientists long suspected that modified forms of amyloid beta and tau could be found circulating in the blood of Alzheimer’s patients. A handful of studies published between 2007 and 2014 showed it might be possible to detect these proteins in blood samples, but the studies could not be replicated. Until recently, blood tests simply were not sensitive enough to measure the tiny concentrations of blood proteins with sufficient accuracy and consistency.

In the late 2010s, researchers at Eli Lilly created the first breakthrough product. Its innovation was a proprietary antibody – a large, Y-shaped protein that attaches to a form of tau called P-tau217, making the tau molecules easier to see and measure. The test immediately caught the attention of Adam Boxer, MD, PhD, a UCSF neurologist and the Endowed Professor of Memory and Aging.

Boxer directs clinical trials for Alzheimer’s disease and frontotemporal degeneration at the Memory and Aging Center. When he heard about Eli Lilly’s test, he was studying a rare neurodegenerative disorder called progressive supranuclear palsy (PSP), which is often misdiagnosed as Parkinson’s disease. Searching for better diagnostic tools, Boxer had become fascinated by a strange phenomenon: Like Alzheimer’s, PSP is marked by a toxic proliferation of tau in the brain, but researchers could find surprisingly little tau in the spinal fluid of PSP patients. Maybe, Boxer thought, the tau proteins were leaking into their blood instead.
Elisabeth Thijssen, PhD, then a doctoral fellow in his lab, set out to explore this hypothesis using Eli Lilly’s powerful new test. Initially, the results were disappointing. Thijssen could find no more tau in the blood of PSP patients than in the blood of people with other conditions, including Alzheimer’s. But when she and Boxer looked more closely at the data, they noticed there was far more tau in the blood of the Alzheimer’s patients than in any other group’s blood. If they could replicate this finding in a larger study, it would be big news.
Tapping into Boxer’s clinical research network, Thijssen and her collaborators tested the blood of hundreds of patients with Alzheimer’s disease and frontotemporal degeneration, one of the diseases most commonly misdiagnosed as Alzheimer’s. They were pleased to find that blood concentrations of tau were 3.5 times higher in the Alzheimer’s patients than in the other participants in the trial. Although half of the patients with frontotemporal degeneration also had tau in their brains, the Eli Lilly test could distinguish between the two populations with 96% of the accuracy of an autopsy.
Thijssen, who now works in consulting in her native Netherlands, presented the results at the Alzheimer’s Association International Conference in July 2019 (and later published them in Nature Medicine). At the same conference, two other research groups reported similar observations. One study, in people with a genetic mutation that causes early-onset Alzheimer’s, showed that the blood test was just as capable as a spinal tap or PET scan at detecting early biological signs of the disease, which can emerge 20 years before cognitive symptoms do. The studies generated worldwide headlines and inspired the development of other promising blood tests.
Researchers still need to better understand the potential limitations of the new tests, Boxer says. It’s possible, for instance, that medications or co-existing medical conditions affect their performance. But he expects that those final hurdles will soon be cleared and that blood tests could start being offered in clinics later this year. The biggest beneficiaries, he predicts, will be “people who have trouble accessing health care,” including underserved populations in the United States and abroad.
An Emerging Debate
As they await the FDA’s approval of the new blood tests, experts have begun to debate how they should be used – and what exactly the results mean. For instance: When does a positive test indicate that a patient has or will develop Alzheimer’s disease?

Ken Covinsky, MD ’88, MPH, a UCSF geriatrician who often works with Alzheimer’s patients and their families, notes that many people die with amyloid plaques in their brains but never develop dementia during their lifetimes. What if blood tests had revealed those plaques years before their deaths? Would that have caused them to worry unnecessarily or pursue harmful treatments they didn’t need?
Blood tests can measure tau tangles as well as amyloid plaques, and there is more evidence directly linking tangles to the onset of cognitive deficits. Still, warns Covinsky, UCSF’s Edmund G. Brown Sr. Distinguished Professor of Geriatrics, “we should proceed with extreme caution.” The widespread availability of biomarker tests, he concedes, will enable earlier diagnoses. “But what exactly are you diagnosing? It’s hard to know what to make of these biomarkers without knowing who is truly going to get dementia.”
Maria Glymour, ScD, a UCSF epidemiologist, says the key question when rolling out a new diagnostic tool should always be: Is this going to improve life for patients? “Fundamentally, what people care about is memory loss and cognitive impairment,” she says. “If you define a disease based on a biomarker, with no incorporation of patient perspectives, you can ‘cure’ the disease by removing the biomarker without improving anything that the patient experiences.”

These concerns are particularly salient now that new, controversial drugs designed to remove amyloid plaques are entering the market. So far, the FDA has approved two drugs in this class, aducanumab and lecanemab, through its accelerated approval program. While the drugs seem to modestly slow cognitive decline, neither comes close to curing the disease. Both also are expensive – now close to $30,000 a year – and can cause brain bleeds and other side effects whose long-term impacts have not yet been studied. Prescribing these drugs based solely on biomarker tests might not be in patients’ best interests, Covinsky cautions.
But others argue that for patients who wish to try all options, an early, biology-based diagnosis could allow them to benefit while their brains are still relatively healthy. Lecanemab, the more effective of the two drugs, can preserve the ability of some Alzheimer’s patients to function on their own for as much as a year and a half longer, Rabinovici says. The drugs’ side effects, he adds, are rarely severe and almost always resolve when patients stop taking the medications.
There is now strong evidence that some blood tests are very accurate predictors of who will develop symptoms of dementia over the next three to five years.”
“If you wait to initiate treatment until people develop full-blown dementia, treatments like lecanemab won’t work,” Boxer notes. “Many patients come into our clinic at a stage that is too advanced for them to benefit.” Blood tests, he maintains, could change that. “There is now strong evidence that some blood tests are very accurate predictors of who will develop symptoms of dementia over the next three to five years,” Boxer says. He points to a large clinical trial called AHEAD that is using the tests to help identify people with Alzheimer’s biomarkers before they show cognitive symptoms and assess whether lecanemab can delay memory loss. The trial, funded by the National Institutes of Health and Eisai Inc., a developer of the drug, is currently enrolling participants at UCSF and other sites across the U.S. and Canada.

And drugs aren’t the only option for patients who test positive for Alzheimer’s biomarkers. Lifestyle changes can make a big difference in outcomes, says neuropsychiatrist Kristine Yaffe, MD, director of UCSF’s Center for Population Brain Health and one of the world’s leading experts on cognitive decline and dementia. Yaffe, the Scola Professor of Psychiatry and Epstein Professor of Geriatric Pyschiatry, studies what she calls “modifiable risk factors.” Her research has shown, for instance, that getting sufficient high-quality sleep dramatically decreases the risk of developing Alzheimer’s disease. Healthy habits like staying physically active and eating a plant-based or Mediterranean diet are also protective, Yaffe says, because they help control other conditions that affect cognition, including hypertension, diabetes, obesity, and high cholesterol.
Recently, Yaffe led a two-year trial in a large group of healthy elderly volunteers to evaluate the effectiveness of prevention strategies. Each participant had at least two identifiable risk factors associated with cognitive decline, such as poor sleep, exercise, or diet. Half of the participants worked with a health coach to improve those factors; the other half served as controls and received only educational materials. The study demonstrated that the intervention worked. At the end of the trial, participants in the experimental group reduced their risk factors to a greater extent and performed 80% better on cognitive tests than those in the control group.
Daniel Gibbs, who was unaware of any family history of Alzheimer’s before his own tests, says his diagnosis inspired his whole family to take proactive measures. Because he has two copies of his Alzheimer’s risk gene, his children all inherited at least one copy. “They know they’re at risk,” he says, “and they’re cognizant of the things they need to do to reduce that risk going forward.”