Joy Littlesunday is an irresistible kid with a gravitational pull that triggers a hug from every person who crosses her path. She has boundless energy and an insatiable desire to connect. Though only 4 years old, Joy is making up for lost time. She was born with a genetic disorder that left her without an immune system – which meant that merely brushing against someone with a cold could have been life-threatening for her.
A bone marrow transplant performed at UC San Francisco when she was 2 months old saved her life.

Joy Littlesunday hams it up with her parents, Jarvison and Christina, on a visit back to UCSF Benioff Children’s Hospital San Francisco, where she received a life-saving bone marrow transplant at age 2 months.
Her condition, severe combined immunodeficiency (SCID), if undetected can be lethal by the time a child turns 1 year old. It’s a disease that haunts Navajo families like Joy’s, who are at a far higher risk of SCID than the rest of the population. But now all babies born in the Navajo Nation are screened for SCID using a test that the tribe played a crucial role in making possible.
Babies born with SCID, a group of rare disorders, lack the capacity to produce functional forms of the immune system’s big guns – B and T cells. B cells and T cells collaborate to detect and attack invaders and to identify and kill infected cells. Together, they insulate us from life’s daily insult of infection and disease.
But havoc can be wrought in this precisely calibrated process by a mutation in a single gene. Joy’s mutation was in the DCLRE1C gene, giving her an unusual form of SCID, known as SCIDA, which occurs with greater frequency among Athabascan speakers, in particular Navajo and Apache Indians. Joy was 2 weeks old when she screened positive for SCID.
The results initially seemed inconclusive, however, and the reservation doctor, an expert on SCID, was out of town when the test results came in. So the clinic staff instructed Joy’s mother, Christina, to head home and keep her baby isolated until they could verify the results.

Joy has severe combined immunodeficiency (SCID), a condition that undetected can be lethal by the time a child turns 1 year old.
Home was on the reservation, in a house with no electricity or running water (though with a view of the sacred San Francisco Mountains, which are part of the Navajo story of origin). The Littlesundays – whose surname derives from the fact that Joy’s great-grandfather picked up goods at a trading post on Saturdays, a day referred to in Navajo as “little Sunday” – had to haul in water from eight miles away. The water was fine for washing and showers, but not for drinking. “I took her home and bathed her in this water,” Christina recalls. “When I think about it now…”
Her guilt is as visceral as it is undeserved for a woman who, soon thereafter, tore herself away from all she knew to get her daughter the bone marrow transplant that would spawn her a new immune system.
“I was not ready for San Francisco or for anything medical,” says Christina, recalling her first trip to UCSF. “I just remember looking out the airplane window, thinking, ‘Wow, that’s a lot of water and a lot of lights,’” as she gazed down at the city she would call home for the next two and a half years – a city a thousand miles from the reservation.
On that day some four years ago, Christina carried Joy tightly swaddled to a papoose board – a sacred crisscross of wood and ornaments – like a care package from a different place in time.
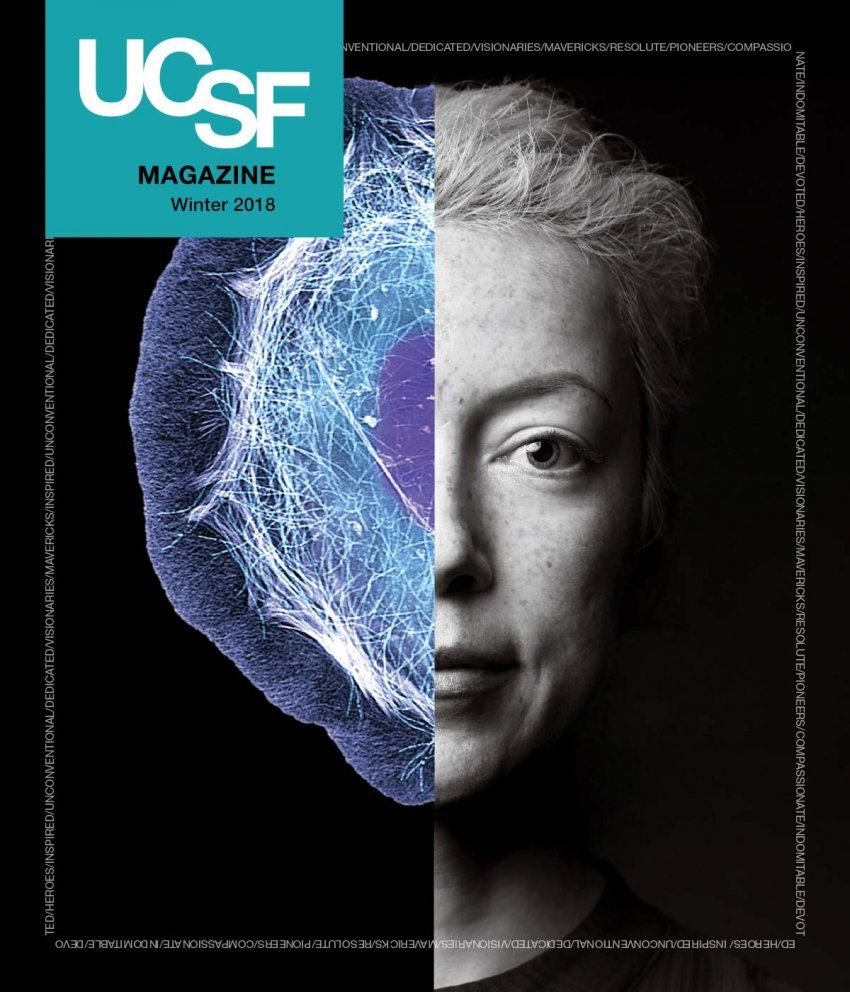
Mort Cowan, MD
Mort Cowan, MD, performed Joy’s bone marrow transplant in a sterile hospital room just three miles from the Pacific Ocean. Cowan, a resident alumnus and the founder of UCSF’s bone marrow transplant program, had been working with Navajo families for decades by the time he did Joy’s transplant, as a drawer full of patient family photos attests. His UCSF colleague Jennifer Puck, MD, a pediatric immunologist, created the screening test that triggered Joy’s transplant.
Through the decades, Puck has met countless families from all over the country who have lost a first child to SCID but caught the illness in a second child before it was too late.
“Grandmothers talk about how a baby was sick all the time, or about how a pediatrician questioned whether they sterilized their bottles,” recalls Puck. “Why should you have to have a tragedy with the loss of one affected baby to save the life of a second baby?”
That agonizing question compelled her to create a screening test for SCID. She and Cowan worked with the Navajo Nation to test the validity of the screen.
Then, in 2009, they started screening infants born in two Navajo hospitals. By the end of 2017, 48 states will be screening all infants for SCID, accounting for over 90 percent of all births nationwide. In a 2014 study involving data from 11 newborn screening programs that had tested over 3 million babies, Puck and Cowan showed that SCID has an incidence of 1 in 58,000 births, nearly double what was previously thought. And SCID is more frequent still among the Navajo people, at 1 in 2,000 births.
Why should you have to have a tragedy with the loss of one affected baby to save the life of a second baby?
A Power Tool
SCID’s path out of obscurity tells a captivating story about the ascent of genetics and technology in medicine over the last few decades. Cells from patients with several forms of SCID will soon be used as a platform for an extraordinary technology – CRISPR. Discovered by Jennifer Doudna, PhD, a professor of chemistry and of molecular cell biology at UC Berkeley, CRISPR is a tool that enables scientists to edit the genome. While many bioethicists and scientists are wringing their hands with worry about potential rogue uses of the tool to edit human embryos, many of those same scientists, as well as clinicians and patients, are excited and hopeful about possible applications of CRISPR for correcting genetic defects within somatic cells, such as the cells that form the immune system.

Jennifer Doudna, PhD
Doudna and Puck, for example, use CRISPR to edit DNA sequences in blood-forming stem cells so that they can correct immune defects. “Jennifer Puck was my first clinical partnership,” says Doudna. “She and I bring to the table very different expertise – I am a basic scientist, and she is a clinician. But together, we will do something potentially transformative for diseases with single mutations.”
Studying diseases with single mutations, like SCID or sickle cell anemia, is particularly compelling because the target and the potential cause and effect of manipulating it are so clear. Yet SCID does pose a unique problem: People with SCID don’t have any T lymphocytes to begin with.
“How do you study or treat a type of cell that isn’t there in the first place?” asks Puck. So the researchers must start with the stem cells that give rise to the mature T cells that are missing in SCID patients – bone marrow stem cells.
Puck and Doudna isolate blood-forming stem cells and, using CRISPR, edit the genes that encode the mutations that they find in affected patients. They grow the stem cells in cultures in a lab setting.
“Even if you only have a few cells,” explains Puck, “you can make edits and recreate in a cell system the genetic problem that we seek to correct in a human. Then we can watch those cells and make them differentiate in tissue culture to see where they get stuck.” If some cells don’t get beyond a certain point, then that shows the researchers which gene is malfunctioning and needs to be corrected.
Old School
Mutations in any of at least 16 different genes can lead to SCID. Puck identified the gene for X-linked SCID, the most common form of the condition, back in 1993. Soon after that, Cowan identified the mutation in SCIDA. In the 1990s, the genome had not even been sequenced yet (that came a decade later, in 2003, and Puck was part of that effort, too, during a stint at the National Institutes of Health).

Jennifer Puck, MD
“Back then, to identify mutations, we would gather many families to do what we called linkage analyses,” Puck explains. Cowan did that on the Navajo Nation.
The process involved contacting members of families with multiple affected individuals and studying which portions of their DNA were co-inherited with the trait leading to SCID. It took 20 years from the time they started SCIDA studies to when they identified the gene and sequenced the Navajo mutation.
“If we were starting today, it would probably take six months, because now we have the human genome sequenced and whole exome sequencing,” says Cowan, a professor emeritus and former chief of the Allergy, Immunology and Blood and Marrow Transplant Division at UCSF Benioff Children’s Hospital San Francisco.
The exome refers to the 1.5 percent of the genome that encodes the proteins that form the building blocks of all of our cells, including cells of the immune system. So if there’s a functional flaw in a baby’s immune system, it will often show up there. “If we’d had whole exome sequencing, we could have found it just like that,” says Cowan, snapping his fingers.
The Promise of Gene Therapy
Cowan and Puck are now ramping up for a new clinical trial of gene therapy for SCIDA, the form of the disease that most affects the Navajo people. They will take blood-forming stem cells out of patients with SCIDA and will use what’s known as a lentivirus to insert a correct copy of the gene into the DNA of these cells. When the cells divide and differentiate into blood cells, the correct gene copy will persist, allowing maturation of functional T and B cells that will last throughout the life of the patient. Prior to receiving the gene-corrected cells back, patients will receive a very low dose of chemotherapy to clear out spaces in their bone marrow, giving the corrected stem cells a place to land and populate after being injected back into the patients.
“The gene-corrected, blood-forming stem cells will become rooted in the bone marrow and grow an immune system for the patient,” says Puck.
SCIDA is the most difficult type of SCID to cure with standard bone marrow transplant therapy. Cowan and Puck will enroll both newborns and older patients with SCIDA in whom an initial bone marrow transplant was not fully successful. Many patients with SCIDA, including Joy, recover only T cell immunity after a standard transplant, making regular intravenous infusions of gamma globulin necessary. These infusions make up for the missing B cells that typically don’t recover in SCIDA patients even after a transplant.
“The immune system is composed of single cells, unlike a solid organ,” explains Puck. And the immune system is portable, making it ideal for the planned gene-addition therapy. The stem cells that give rise to the immune system can be removed, modified, and replaced. “And the immune system remakes itself every day,” she adds. Hopefully the new gene therapy will give patients a second chance at a fully functioning immune system, allowing them to be free of gamma globulin infusions.
While Puck and Cowan are optimistic about the SCIDA trial – the use of a lentivirus to carry a correct copy of the gene into blood-forming stem cells – there are likely to be still more improvements in the future. The next step for SCID may be gene editing – taking out blood-forming stem cells from the marrow, correcting their mutation with CRISPR, and returning the corrected cells to the patient. But that still leaves the issue of having to create space for the corrected marrow.
“The ultimate goal,” says Cowan, “would be to correct the defect by gene editing directly in the patient’s stem cells, without having to first remove them. This would eliminate the need to give any space-creating chemotherapy beforehand.” With only one gene to correct, SCID is an ideal target for such a treatment. Puck and Doudna’s professional partnership may make that come to pass as the technology is further refined.

Grounding
But as heady as the science is, it’s the people who are preeminent. Puck and Cowan never fail to board a plane for Arizona to hold an annual clinic on the Navajo Nation for their previously treated patients. They have known some of these patients for decades. After the clinic, all the patients and families and doctors get together for a barbecue to check in with one another.
That’s when I realized that Joy has a whole life ahead of her.
“I remember my first patient get-together with Joy,” recalls Christina. Joy was just shy of 3 years old and was finally home, though not yet on the reservation. Joy and her family now live in a little house with running water and electricity on a street serendipitously named San Francisco.
All the SCID families at the gathering, in a dusty garden outside the Navajo Indian Health Service Hospital, took turns telling their stories. “This one young lady stood up and introduced herself,” Christina says. “She was 20-something with twin baby girls. She had SCID. That’s when I realized that Joy has a whole life ahead of her.”
Illustrations: Stephanie Koch