Before 1846, surgery was a crude and brutal undertaking, typically performed on conscious patients lashed to their beds. Then a Boston dentist publicly demonstrated that the highly flammable chemical diethyl ether – commonly called ether – could render a patient unconscious and insensitive to pain. Overnight, surgery became a major player in modern medicine.
Surgery has advanced dramatically since then, incorporating laparoscopes and lasers, titanium joints and transplanted organs. Anesthesia has changed much less, with just a handful of better drugs emerging. Ether gave way to less flammable chemical cousins. Barbiturates and dexmedetomidine were found by accident. And an intentional, decade-long hunt for safer alternatives produced propofol, which was approved in 1989 and remains the most commonly used intravenous general anesthetic.
Propofol and the other drugs used in today’s operating rooms are safe when administered by specialists trained to manage their potentially life-threatening side effects. But anesthetics that don’t require such expertise would open a brave new world in which surgery would be less onerous and less expensive for patients. It would also be more accessible in under-resourced environments, including rural areas, developing countries, and war zones, where a lack of anesthesiologists and their monitoring and life-support equipment often limits patients’ access to needed procedures.
The prospect of portable surgery requiring fewer specialists and tools has motivated the Defense Advanced Research Projects Agency (DARPA) to fund a team of researchers based at the UCSF School of Pharmacy and UC San Diego who are seeking dramatically safer anesthetics. Pharmaceutical chemistry professors Brian Shoichet, PhD ’91, and Jason Sello, PhD, are leading a project that combines artificial intelligence, molecule design, and innovative animal models to evaluate 6 million small molecules for anesthetic properties. The massive search spans a broad range of chemicals, raising the possibility that some may act through undiscovered, potentially safer biological mechanisms. The researchers expect to put about 10 drugs on the path to clinical trials, which would open the floodgates in a field that has moved at a trickle.
“We’re at a moment where everything is coming together to accelerate progress. There is a consilience of multiple technologies,” says Sello. “And at UC, we have the right group of people with the right skills and the right interests to bring them together.”
A strange brew of methods working in sync
Computers using a technique developed by Shoichet will handle the largest swath of the 6 million chemicals. Large-library docking works like a high-speed virtual puzzle to determine which molecules in a vast library might interact with specific biological targets.
Most known anesthetics affect one of two biological mechanisms – propofol and benzodiazepines interact with the GABA-A ion channel, while dexmedetomidine interacts with alpha-2A adrenergic receptors. Shoichet is looking for other compounds that do the same. He starts with detailed models of these two cellular ports, including their shape and chemical properties. Then the computer program runs through similar models of millions of chemical compounds to identify which ones fit (or “dock”) in those ports. Those that do are likely to have anesthetic effects.
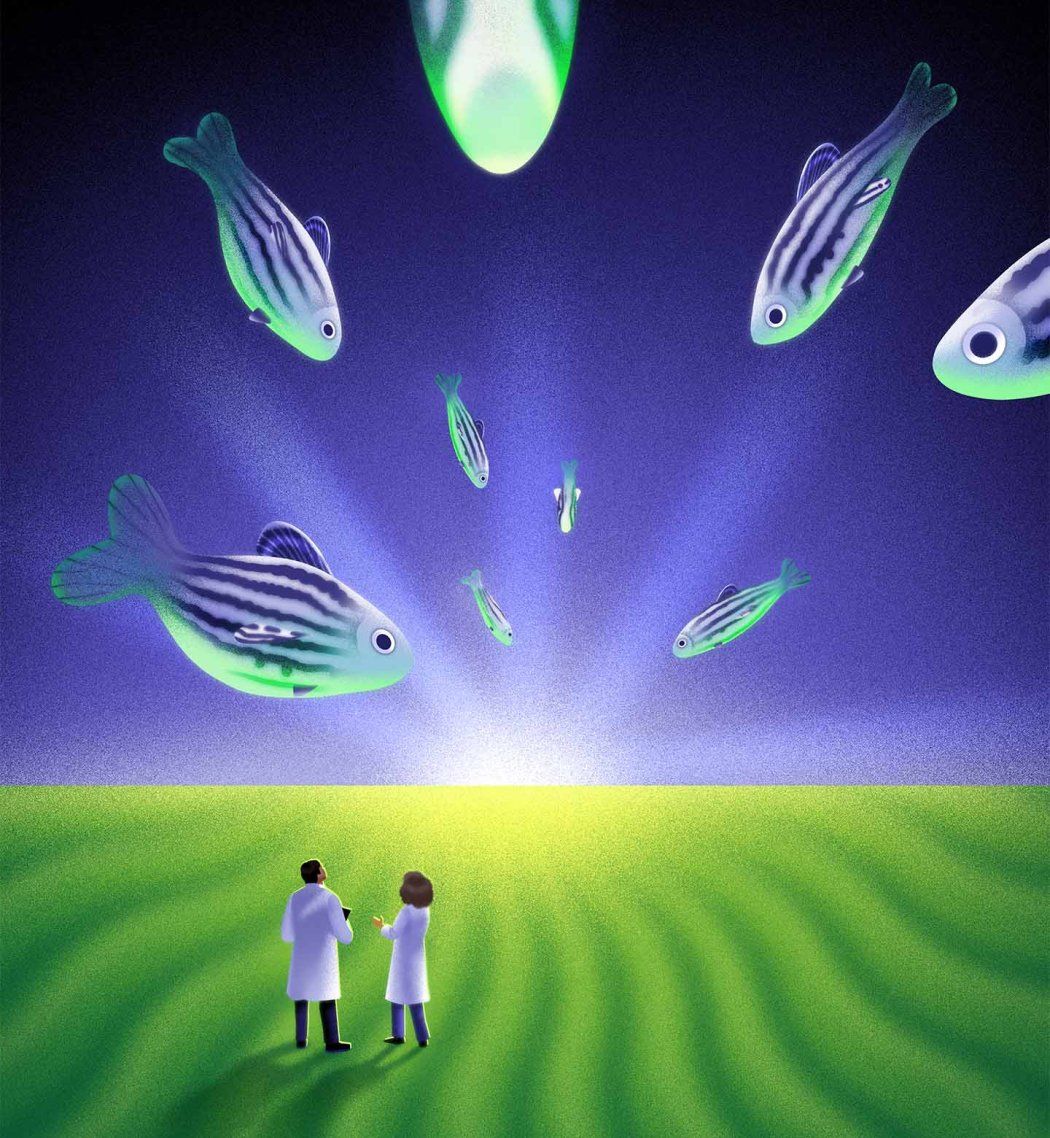
Shoichet flags these for Matthew McCarroll, PhD, an adjunct assistant professor of pharmaceutical chemistry whose scientific workhorses are zebrafish larvae. As vertebrates, the fish have neurotransmitters similar to those in humans. But they reproduce quickly and develop organs within five days of fertilization. McCarroll and others have shown that these fish can help clear one hurdle that has slowed the search for better anesthetics: You can’t start, as most research does, with fast-growing cells in petri dishes because cells aren’t conscious. But at five days old, the fish are small enough to support the kinds of experiments researchers would otherwise perform with cells.
Larval zebrafish have another useful trait. They respond in specific ways to different types of neuroactive drugs, and McCarroll has uncovered a paradoxical reaction in anesthetized larvae: Knocked-out larvae whip their tails when they’re exposed to vibration, while their awake compatriots show no response.
“The anesthetized fish don’t react to any other stimuli, but they have this really robust acoustic startle response that we don’t see with any other type of drug,” McCarroll says. “It’s super strange.”
McCarroll has turned this curious behavior into a clever lab test: Put a small – and low-cost – amount of a test compound into 96 tiny wells, each one containing as many as eight larval zebrafish. Vibrate the tray and film the zebrafish. In every well with fish that twitch, you’ve got a potential anesthetic compound. McCarroll’s postcard-sized tray can test 80 compounds at a time, with 16 control specimens to boot.
So far, about half the compounds identified by Shoichet’s docking technique have caused McCarroll’s zebrafish larvae to twitch in their telltale way. McCarroll is also dosing the larvae with other, randomly chosen compounds, to fish for one that works through a new biological mechanism that triggers fewer side effects than propofol or dexmedetomidine. New targets would also invite other researchers to join the hunt for better anesthetics.
McCarroll shares his hits with Sello, who looks at the compounds’ chemistry, eliminating any with properties known to cause, for example, liver damage. Sello also adjusts some compounds’ chemical makeup – say, to make them biologically soluble or more potent. (Molecule editing has become more precise in the decades since propofol was first made.) Sello sends the modified molecules to McCarroll so he can dose the fish, test their organs for damage, and even peer into their transparent heads to see how the drugs affect their brains.
“It’s an iterative process,” Sello says. “We’ll try to create compounds that are more potent or that we would predict would have better pharmacological properties.”

Candidates that pass all these tests will ultimately be evaluated in mice, putting the compounds on a more conventional path toward clinical trials. Extensive safety testing would still have to happen before any drugs could be tried in humans, says Michael Bokoch, MD, PhD, an associate professor of anesthesia who is also part of the all-star research team.
Hopes of revolutionizing surgery
A pilot project using the same unconventional method has already borne fruit. After screening 12,000 compounds, the team identified a candidate molecule. Through Sello’s modifications, it became nidradine, a drug that has successfully anesthetized mice. Even more intriguing, it also has analgesic, or painkilling, properties. If nidradine makes it to the OR, it could reduce reliance on opioid painkillers.
“Its analgesic activity comes from binding to a sodium ion channel called NaV1.8, which is a hot target right now for the development of compounds to treat chronic pain,” Sello says. “And our molecule came out of a random screen!”
The pilot has fueled the researchers’ optimism that they may find as many as a dozen promising new drugs from the larger project.
The research’s most ambitious goal is to revolutionize surgery itself, untethering it from highly specialized anesthesiologists. Safer drugs would allow nurses and medics to put patients under, sometimes without the bulky, expensive equipment that monitors and supports patients’ vital functions in case of the depressed cardiorespiratory activity that many existing anesthetics can cause.
The ambition is grounded in a challenge: Anesthesiologists are in short supply in the military, in rural areas, and in lower-income countries. In war zones, wounded soldiers may wait precious minutes or hours for surgery while they are transported to a military medical center appointed with anesthesiologists and the tools they need. Similar situations arise in rural areas and lower-income countries. In fact, wait times in such locales can be indefinite, with millions of people going without needed surgeries every year.
There would be benefits even at top-tier medical centers like UCSF, where dramatically safer drugs would allow anesthesiologists to focus on the most specialized and high-risk cases. For lower-risk procedures, hospitals could reduce their reliance on highly trained specialists, potentially lowering costs and making care more accessible.
“If the drugs were much safer, you might not even need an anesthesiologist for procedures such as cataract surgeries and endoscopies,” Bokoch says. “That would extend our work-force and save patients money.”
But even if the search among the 6 million compounds finds just one that is incrementally safer than propofol, that improvement, extended across the hundreds of millions of patients worldwide who undergo surgery every year, would be substantial. Currently, anesthesia contributes to death in a couple hundred people in the United States each year.
“We don’t have to accept the status quo,” Sello says. “We can do better, so let’s try to do better.”