The people we love are the sum of countless parts. A calm steadiness, outsized laugh, ready wit, meticulous aesthetic: it can be hard to recall every trait that draws us in. And yet these traits are never more obvious than when they disappear, bit by bit, as they do in people with behavioral variant frontotemporal dementia (bvFTD). In its punishing trajectory, the disease tears away at all we associate with identity, rendering someone a fragment of his or her former self.
Radical changes in personality happen along bvFTD’s destructive course, which runs the better part of a decade. Lifelong Republicans become Democrats or vice versa; agnostics find religion; aggressive types grow placid and apathetic; sensitive souls become callous or tactless. Empathy and social skills deteriorate until, ultimately, patients with bvFTD are unrecognizable to their loved ones, a heartbreaking transformation that can make caretaking profoundly difficult.
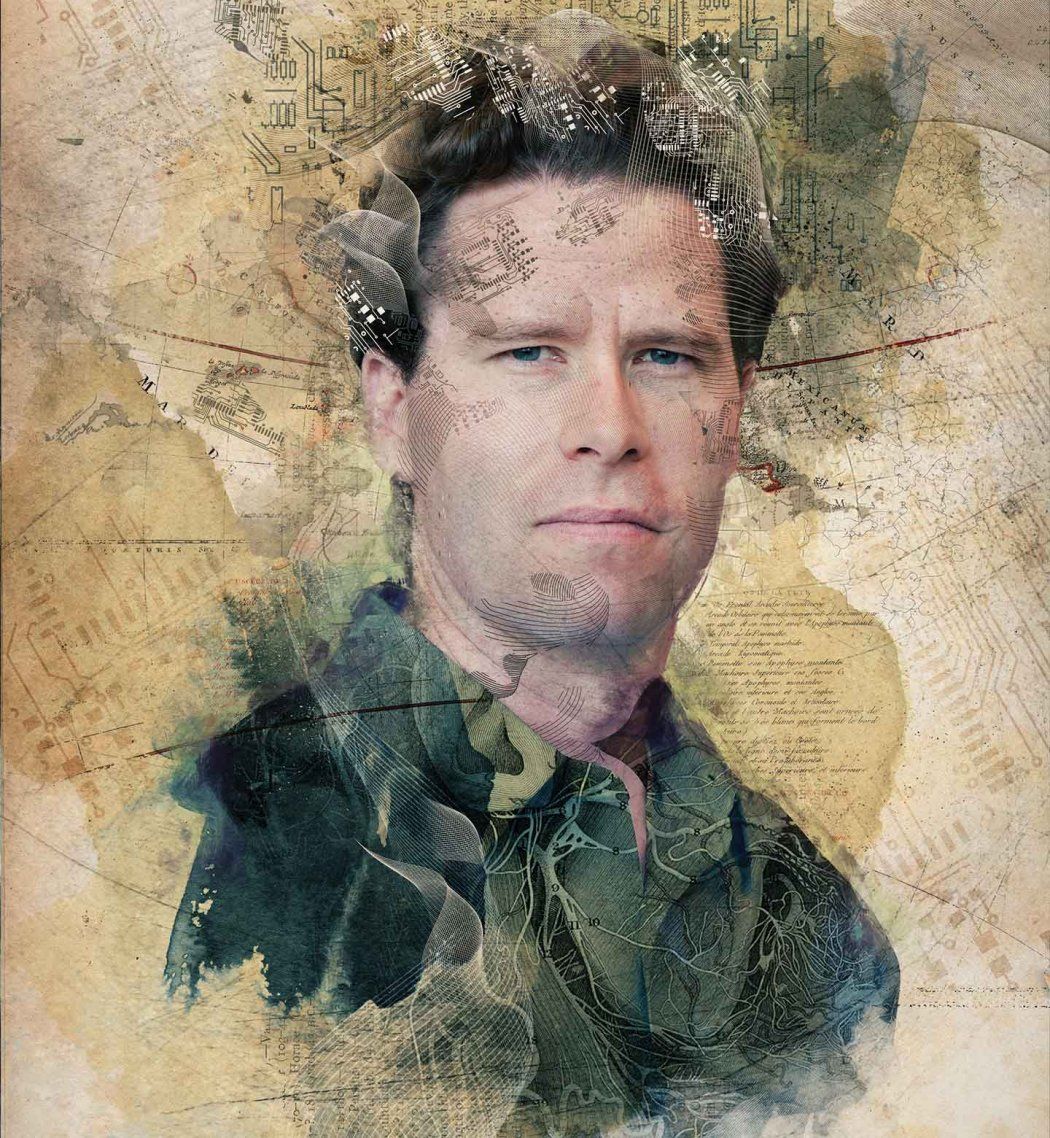
William Seeley, MD, a neurologist at UCSF’s Memory and Aging Center, documents each stage of bvFTD – part of a neurodegenerative disease family that’s the leading cause of dementia in people under 65 – with painstaking precision, seeking a way to stave off his patients’ disappearance. These patients are a focus of the center’s multidisciplinary teams, in which neurologists, psychiatrists, geriatricians, neuropsychologists, nurses, speech pathologists, social workers, genetic counselors, and pharmacists work together to combat a broad range of diseases that cause cognitive impairment.
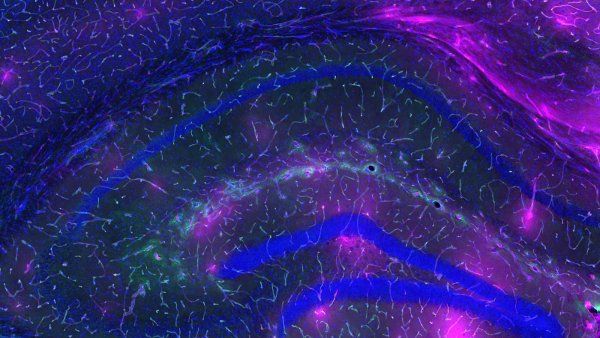
Seeley, a 1999 graduate of UCSF’s School of Medicine, hopes to correlate the behavioral changes he notes with subtypes of the disease, as well as to changes occurring in the brain. Using functional magnetic resonance imaging (fMRI) and tissue analyses, he has already made a critical discovery: bvFTD targets the von Economo neuron (VEN).
Romanian-born neurologist Constantin von Economo wrote with remarkable foresight about the spindly-shaped neurons that bear his name in his elaborate brain atlas, co-authored with George Koskinas and published in 1925. The trailblazing scientist identified VENs in two regions of the brain – the anterior cingulate gyrus and the frontoinsular cortex. Though a good distance apart, the regions are alike enough on a microscopic level that von Economo hypothesized they were functionally similar.
“In my favorite paper of all time, von Economo speculated that the frontoinsular cortex might be the part of the brain that receives all the incoming information from the body about its immediate condition – feelings we experience like the beating of our heart or butterflies in our stomach – an idea that is now becoming widely accepted in neuroscience,” says a grateful Seeley. “He was way ahead of his time.”
Evidently, so is Seeley. One hundred years after von Economo started his atlas, Seeley was named a MacArthur Fellow for his own multidimensional maps of the cerebral environs that VENs inhabit. Nicknamed “genius grants,” the fellowships are given to the approximately two dozen people across the United States who have demonstrated “extraordinary originality and dedication in their creative pursuits.”
Seeley’s genius status was cemented when news of his fellowship hit The New York Times in September 2011. He and his wife, Hilary, were on the maternity ward of UCSF’s Moffitt Hospital when the messages began flooding in.
“My daughter was seven hours old, and we had all just shared the pink light of her first sunrise when my phone lit up with messages from everyone I had ever known on the East Coast,” says Seeley. “I’m pretty sure I am the only MacArthur Fellow for whom the news came as the second best thing to happen that day.”
Surveillance: Three-Dimensional Mapping
Seeley’s maps cover uncharted territory by layering three dimensions on top of one another: behavioral, cellular, and neural networking. To build a patient map, he begins by collecting behavioral observations – directly and via anecdotes from family members. Then he scans the brain to track neural activity.
“Through fMRI, we’re developing brain imaging strategies for understanding the crosstalk among the brain regions,” says Seeley. “Over the course of an eight- to 10-minute scan, we can identify areas that are synced and wired up together into networks.”
Through fMRI, we’re developing brain imaging strategies for understanding the crosstalk among the brain regions.”
Seeley hopes his fMRI surveillance will allow him to monitor glitches or slowdowns in this crosstalk between intrinsically linked areas of the brain, even before he begins to detect their shrinkage (the conventional measure of degeneration). These communication breakdowns could be the tip-off to the VEN (cellular) disintegration that causes neural networks to fray and behavior to deteriorate – a three-dimensional corrosion.
What does this mean to the people who count the most, patients and their caregivers? For now, definition. By matching specific network failures to typical patient behaviors, Seeley’s maps can show the cascading patterns of network and behavioral declines that define not only bvFTD, but the other four FTD subtypes as well. With these paths of progression in hand, clinicians may be able to make faster diagnoses and, eventually, stage therapeutic interventions.
Disease Starts Early, Moves Fast
In contrast to Alzheimer’s, which hits later in life and launches a slow attack on memory, bvFTD starts early and moves fast, erasing not memories so much as self.
“My Alzheimer’s disease caregivers almost always say that their loved one is still there, to the end,” shares a noticeably moved Seeley. “This is not the case for my bvFTD caregivers.”
It’s as if the patient has simultaneously lost the gas pedal and the brakes.”
Digging deeper into the details of his map dimensions, Seeley combines anecdotes from various patients to describe the quintessential behaviors of someone early on in the disease. “Say the patient is walking in a mall and sees an 8-year-old girl standing alone, looking concerned,” says Seeley. “Normally, that would induce a little alarm signal: ‘Child in distress…take action to solve problem!’ But the patient passes right by. Now imagine the 8-year-old standing happily with her mom in the mall. The patient might go up to the girl, pat her on the head, and take a lick of her lollipop.”
“That’s the same patient showing a complete failure to act when action is needed,” says Seeley, “or a complete failure to suppress an unwanted action when stimuli are just attractive enough to draw the patient’s behavior toward the target, the little girl. It’s as if the patient has simultaneously lost the gas pedal and the brakes.”
Decade-Long Scourge of Degeneration
According to Seeley’s maps, both responses of the patient in the mall could be correlated to the same lesion in the brain – one that interrupts communication systems.
“At any given moment, we’re bringing potential actions into consciousness and weighing the emotional consequences of each action’s predicted outcome,” says Seeley. “We use those anticipated reactions to decide whether or not to act.” Patients with bvFTD have a break in that feedback loop, which quiets or silences the signals of the social and emotional navigation system that advises them whether to apply the gas or the brakes.
The regions involved are exactly those that intrigued von Economo: the frontoinsular cortex and the anterior cingulate gyrus. Just as von Economo speculated, the frontoinsular cortex receives all of the autonomic responses regarding the body’s condition – the quickening of our pulse that tells us we’re afraid, the goose bumps on our arms alerting us we’re cold – that we experience as feelings.
This region is intrinsically connected by critical communication corridors to the anterior cingulate gyrus – the output pathway driving behavior, which would normally compel the patient to help the lost girl after receiving a distress call from the frontoinsula.
The disease can be a decade-long scourge of degeneration in these regions. The frontoinsula and anterior cingulate deteriorate along with the communications between them, causing patients to veer far off the beaten social path. Tactless and impulsive acts can be as abundant as they are outrageous, including sexual deviance or verbal assaults on strangers. Some patients have been known to go out in 80-degree weather in a heavy parka and end up dehydrated in an emergency room. Others may eat and eat to the point of sickness and obesity.
“The heatstroke, overeating, and tactless behaviors can all be understood within this framework of the patient’s inability to represent the moment-to-moment state of the body and act based on those internal cues,” says Seeley.
For now, the only treatments Seeley can offer his patients and their families are antidepressants and anti-anxiety drugs to help control behaviors like overeating or compulsivity. Seeley also talks through behavioral strategies, such as placing locks on kitchen cabinets and passing out note cards in public explaining that the patient is struggling with an Alzheimer’s-like illness that affects behavior.
Proteins Misfold and Disrupt Neuronal Function
Seeley’s optimism is in the final, cellular layer of his maps, where he sees protein targets just begging for the right therapeutic weapon. Postmortem studies of bvFTD patients show they have one of three lethal proteins in their brains: tau, TDP-43, or FUS.
“Each of these proteins normally lives in nerve cells. In bvFTD, the proteins misfold, clump together, and disrupt neuronal function, including that of the VENs,” explains Seeley. While he hopes to create a behavioral profile that might match each offending protein, he fears that the differences might be too subtle, making it difficult to hone in on an individual protein. “What we really need is a blood, urine, or imaging test that tells us with 100 percent certainty which protein is present, so we can find a specific drug to target each one.”
Some patients have a clear family history of the disease, which can be pinpointed using a blood test for disease-causing genetic mutations. This patient subset represents 10 to 20 percent of the larger FTD population. “These families are our greatest hope,” says Seeley.
Patients with mutations in the tau gene will soon, Seeley explains, participate in clinical trials of tau-inhibiting therapies, which he hopes will prevent the disease from devastating yet another generation of each patient’s family. The drugs could also have enormous implications for patients with Alzheimer’s disease, whose brains are ravaged by both tau and another protein, amyloid beta.
The families of his patients are squarely behind Seeley, appreciative of all he’s done so far. In fact, many of the messages he received during his daughter’s first sunrise were congratulations from those families. “The most touching emails were from my former patients’ widows, widowers, and children, saying, ‘I remember our time with you, and it made a difference. Keep on doing what you do,’” he says with a long exhale.
Seeley speaks with urgency when describing the difficulty in treating people who can’t advocate for themselves. “Cancer docs have had to take on the idea that they will make their patients worse before they make them better,” he says. “Their patients willingly take the risk of enduring toxic blasts of chemo and radiation to save their lives.”
Yet asking his bvFTD patients to take such risks is inherently harder when Seeley can’t know if they even understand his question. But he can guess how the children of his patients might answer, if they knew bvFTD was their destiny. And he certainly knows what his own answer would be.
“If I knew ahead of time I would contract this disease, I’d want to take any risk to stop it. In the search for treatments, we have to push past that ingrained do-no-harm reticence,” he says. “Progress almost always involves risk.”
Channeling his oncology colleagues, Seeley is embracing risks well worth taking. “We are working with our industry partners to move promising treatments forward. There’s a lot to be hopeful about.”
Drawing Parallels With Autism
The blush of red corresponding to brain activity on Seeley’s fMRIs has cast new light on the social brain. He and others in the field are drawing parallels between the brains of his patients who become deaf to social cues and the brains of children with autism who struggle to learn them in the first place. “There’s a striking correlation between autistic spectrum traits and the cingulate’s connectivity with the insula,” says Seeley.
Some patients with FTD – primarily those with a form that attacks the language system – can also develop the savant-like behaviors similar to those on the autistic spectrum. In these patients, untapped parts of the brain light up as other regions degenerate, giving them new and extraordinary creative talents.
“One of our patients was a biologist who picked up a paintbrush for the first time about eight to 10 years before her first misspoken word,” says Seeley. He collaborated with Memory and Aging Center Director Bruce Miller, MD, to publish a paper about the woman. “Even when she had become mute, she was still creating beautiful paintings.”
Seeley believes a push-and-pull relationship between brain systems is at work within these patients. “I think of the woman’s drive to paint as an early indicator of her brain changing and pushing her toward that behavior,” he speculates. “As her frontal language system began to wither, its role in suppressing activity in her visual brain began to fail, creating a richer visual experience and compelling her to paint.”
Seeley sees opportunities like this – to think about the neural origins of creativity – as a bonus. “The fact that we get to think about self, creativity, emotion, sociality, and all those really fascinating things about the brain along the way…that’s gravy for me,” he says. “But we don’t ask these questions out of simple curiosity. Everything we do is meant to move us toward curing or preventing disease.”