On January 25, a man vacationing in Cambodia with his family went swimming in their hotel pool. After toweling off, he spiked a fever and was sent to a local hospital, where his nose and throat were swabbed and the samples were tested for a deadly virus ascendant in his hometown of Wuhan, China. By the following afternoon, the diagnosis was delivered: Cambodia’s first case of COVID-19.
Officials whisked the samples off to scientists in Phnom Penh for further analysis. The hospital test had provided simple confirmation: The virus is here. But to understand its path and contain its spread, health experts needed details. How had the virus arrived? Was it the same as the strain storming across China? Or was it a related but different virus that had emerged independently?
Months earlier, before anyone had heard of COVID-19, the Phnom Penh lab had begun using a new system, introduced by researchers from the San Francisco-based Chan Zuckerberg Biohub, to answer those very questions. It consisted essentially of a commercial gene sequencer and sophisticated cloud-based software called IDseq, which identifies a virus or other pathogen from its genetic sequence. The Cambodian group was one of 11 international infectious disease laboratories using the technology to study diseases like dengue and malaria. But in late January, the Cambodian scientists turned their attention to sequencing the novel coronavirus newly landed at their door.
The sequencing data confirmed what everyone had suspected: The virus had indeed originated from the initial outbreak in Wuhan, having hitched a ride in the unsuspecting tourist. More profoundly, though, the speed and success with which the Cambodian lab executed the analysis revealed to the Biohub team the power of their IDseq technology. Here was a tool that could minutely track – and thus help combat – what was quickly becoming a global pandemic.
“At that point, I thought that’s what our priority would be – turning our eyes to other parts of the world to try to contain the fires there,” says biochemist Joe DeRisi, PhD, UC San Francisco’s Tomkins Professor and co-president of the Biohub.
“And then the fires came here.”
Timeline legend:
National or global events
UCSF events
12/31/19:
A pneumonia “of unknown cause” is identified in Wuhan, China
1/12/20:
China shares the genetic sequence of the novel coronavirus with the world
1/26:
California confirms its first case of COVID-19, the third in the U.S.
1/30:
Scientists in Cambodia track the burgeoning outbreak using the Biohub’s IDseq technology
1/30:
The virus spreads to 18 countries outside China; WHO declares a global health emergency
1/31:
The U.S. government issues a policy discouraging clinical labs from developing in-house COVID tests, eventually leading to widespread testing delays and shortages
2/6:
The U.S. CDC begins distributing its own test kits to state-run health labs; the kits are later found to be defective

UCSF biochemist Joe DeRisi, PhD, helped identify the original SARS virus in 2003. Now co-president of the Chan Zuckerberg Biohub, he led the charge in converting a portion of the research center to COVID testing.
By late February, the Bay Area had begun bracing for its own surge of COVID cases. DeRisi was texting daily with Priscilla Chan, MD ’12, mulling the right problem to tackle. Chan had met DeRisi during her student days at UCSF and had been impressed by his knack for rooting out the causes of mysterious infections – including the 2003 SARS epidemic and scourges that kill boa constrictors, cockatiels, and honeybees. So, in 2016, when Chan and her husband, Facebook founder Mark Zuckerberg, made a $600 million gift to create the Biohub, with the goal of eradicating infectious diseases, they asked DeRisi to lead it. Now they wondered how they might help thwart the burgeoning COVID pandemic.
DeRisi assembled a small task force to brainstorm ideas. Then, out of the blue, his cell phone rang. “I almost didn’t answer it because I thought it was a telemarketer,” he recalls. It was actually Gavin Newsom, the governor of California. He wanted to know what DeRisi thought the state should do to avoid mistakes in its COVID response. More testing, DeRisi said, without missing a beat. If you want to make smart decisions about quarantining people or locking down parts of the economy, he told Newsom, you need to know where the virus is and who’s infected. In other words, you need to be able to test a lot of people. “Otherwise you’re flying blind,” he told the governor.
The conversation got DeRisi thinking. Who was going to do all this testing? It was becoming clear that the federal government wasn’t up to the task. The U.S. Centers for Disease Control and Prevention (CDC) already had a testing backlog, plus many of the test kits it was sending to states were proving defective. “The stark realization for me was there was no cavalry coming,” DeRisi says. “The CDC wasn’t going to ride in and provide tens of thousands of tests to Californians. Neither were the local health departments – they weren’t powered to do it.”
The stark realization for me was there was no cavalry coming.”

UCSF biochemist Joe DeRisi, PhD, helped identify the original SARS virus in 2003. Now co-president of the Chan Zuckerberg Biohub, he led the charge in converting a portion of the research center to COVID testing.
By late February, the Bay Area had begun bracing for its own surge of COVID cases. DeRisi was texting daily with Priscilla Chan, MD ’12, mulling the right problem to tackle. Chan had met DeRisi during her student days at UCSF and had been impressed by his knack for rooting out the causes of mysterious infections – including the 2003 SARS epidemic and scourges that kill boa constrictors, cockatiels, and honeybees. So, in 2016, when Chan and her husband, Facebook founder Mark Zuckerberg, made a $600 million gift to create the Biohub, with the goal of eradicating infectious diseases, they asked DeRisi to lead it. Now they wondered how they might help thwart the burgeoning COVID pandemic.
DeRisi assembled a small task force to brainstorm ideas. Then, out of the blue, his cell phone rang. “I almost didn’t answer it because I thought it was a telemarketer,” he recalls. It was actually Gavin Newsom, the governor of California. He wanted to know what DeRisi thought the state should do to avoid mistakes in its COVID response. More testing, DeRisi said, without missing a beat. If you want to make smart decisions about quarantining people or locking down parts of the economy, he told Newsom, you need to know where the virus is and who’s infected. In other words, you need to be able to test a lot of people. “Otherwise you’re flying blind,” he told the governor.
The conversation got DeRisi thinking. Who was going to do all this testing? It was becoming clear that the federal government wasn’t up to the task. The U.S. Centers for Disease Control and Prevention (CDC) already had a testing backlog, plus many of the test kits it was sending to states were proving defective. “The stark realization for me was there was no cavalry coming,” DeRisi says. “The CDC wasn’t going to ride in and provide tens of thousands of tests to Californians. Neither were the local health departments – they weren’t powered to do it.”
The stark realization for me was there was no cavalry coming.”
2/23:
Cases surge in Italy, eventually shutting down the world’s main nasal swab factory
2/29:
The U.S. FDA announces a new policy enabling clinical laboratories to develop their own tests
2/29:
UCSF laboratory scientists begin working on a test in-house
But what about the Biohub? They had the space to set up a lab, the scientists and engineers to get it going, a line of volunteers willing to do the work, and even a donor offering to pay for it. “What could we be doing that would be more important?” DeRisi asked himself. “Nothing.”
There was just one problem. The Biohub didn’t have a license to run a clinical lab. As a research center studying the biology of human diseases, the Biohub used tools and techniques similar to those of diagnostic labs. But while research labs are designed to foster innovation and experimentation, clinical labs prioritize consistency and regulation. Quality must be tightly controlled, documentation systems established, and tests validated. Converting a portion of the Biohub’s research team into a clinical one wouldn’t be trivial.
“We were trying to think outside of the box about what they could do,” says Steve Miller, MD, PhD, the director of UCSF’s clinical microbiology lab, which often partners with the Biohub on research projects. When COVID hit, Miller and his staff had started working around the clock to develop a viable diagnostic test and to gather the necessary equipment and supplies in preparation for the hordes of patients expected to start flocking to UCSF hospitals. His team had the means to do maybe a few hundred tests per day – likely not enough to meet UCSF’s needs, let alone the Bay Area’s.
The Biohub team calculated they could easily achieve a per-day rate in the thousands, they told Miller, significantly boosting California’s testing capacity – which, in the absence of national leadership, was (and still is) being filled by a patchwork system of commercial and public labs. But the team was hamstrung by the state’s clinical licensing laws. So what to do? Maybe they could test people as part of a research study? No, because then study participants couldn’t legally get their results. Maybe they could send positive samples to UCSF for validation? No, that would be a logistical nightmare. Well, then, what if the Biohub simply got certified as a clinical lab?
“My original response was ‘Oh, hell no,’” says Ed Thornborrow, MD, PhD, Miller’s boss and the medical director for all UCSF clinical labs. California’s licensing rules, he knew, were even stricter than federal guidelines. Meeting them under normal circumstances could take months, possibly a year – an unacceptable timeline. But he agreed to look into the possibility and concluded it was doable under two conditions.
First, California’s health department would have to approve the Biohub as a temporary extension of one of UCSF’s clinical labs. Check.
Second, the Biohub-turned-testing lab would have to be staffed by clinical laboratory scientists, licensed specialists who had completed months of postgraduate coursework and had passed an exam. “That wasn’t going to happen,” Thornborrow says. “These people are in short supply. You can’t just go hire dozens of them on the spot; they’re not out there.” But hundreds of UCSF graduate students and fellows trained to do laboratory science were offering their labor. “If we were going to get the Biohub lab off the ground, we would first have to get California to change the law,” Thornborrow says.
And so, with help from the UC Office of Legal Affairs, they did. On March 12, the day after the World Health Organization officially declared a pandemic, Governor Newsom issued an executive order nixing the staffing restriction. Check, check.
Suddenly, the road to certifying the Biohub’s COVID testing lab was clear. Now DeRisi and his team just had to build it.
But what about the Biohub? They had the space to set up a lab, the scientists and engineers to get it going, a line of volunteers willing to do the work, and even a donor offering to pay for it. “What could we be doing that would be more important?” DeRisi asked himself. “Nothing.”
There was just one problem. The Biohub didn’t have a license to run a clinical lab. As a research center studying the biology of human diseases, the Biohub used tools and techniques similar to those of diagnostic labs. But while research labs are designed to foster innovation and experimentation, clinical labs prioritize consistency and regulation. Quality must be tightly controlled, documentation systems established, and tests validated. Converting a portion of the Biohub’s research team into a clinical one wouldn’t be trivial.
“We were trying to think outside of the box about what they could do,” says Steve Miller, MD, PhD, the director of UCSF’s clinical microbiology lab, which often partners with the Biohub on research projects. When COVID hit, Miller and his staff had started working around the clock to develop a viable diagnostic test and to gather the necessary equipment and supplies in preparation for the hordes of patients expected to start flocking to UCSF hospitals. His team had the means to do maybe a few hundred tests per day – likely not enough to meet UCSF’s needs, let alone the Bay Area’s.
The Biohub team calculated they could easily achieve a per-day rate in the thousands, they told Miller, significantly boosting California’s testing capacity – which, in the absence of national leadership, was (and still is) being filled by a patchwork system of commercial and public labs. But the team was hamstrung by the state’s clinical licensing laws. So what to do? Maybe they could test people as part of a research study? No, because then study participants couldn’t legally get their results. Maybe they could send positive samples to UCSF for validation? No, that would be a logistical nightmare. Well, then, what if the Biohub simply got certified as a clinical lab?
“My original response was ‘Oh, hell no,’” says Ed Thornborrow, MD, PhD, Miller’s boss and the medical director for all UCSF clinical labs. California’s licensing rules, he knew, were even stricter than federal guidelines. Meeting them under normal circumstances could take months, possibly a year – an unacceptable timeline. But he agreed to look into the possibility and concluded it was doable under two conditions.
First, California’s health department would have to approve the Biohub as a temporary extension of one of UCSF’s clinical labs. Check.
Second, the Biohub-turned-testing lab would have to be staffed by clinical laboratory scientists, licensed specialists who had completed months of postgraduate coursework and had passed an exam. “That wasn’t going to happen,” Thornborrow says. “These people are in short supply. You can’t just go hire dozens of them on the spot; they’re not out there.” But hundreds of UCSF graduate students and fellows trained to do laboratory science were offering their labor. “If we were going to get the Biohub lab off the ground, we would first have to get California to change the law,” Thornborrow says.
And so, with help from the UC Office of Legal Affairs, they did. On March 12, the day after the World Health Organization officially declared a pandemic, Governor Newsom issued an executive order nixing the staffing restriction. Check, check.
Suddenly, the road to certifying the Biohub’s COVID testing lab was clear. Now DeRisi and his team just had to build it.
3/2:
The Biohub creates a COVID-19 task force
3/4:
California declares a state of emergency
3/9:
UCSF begins providing in-house testing but has only enough capacity to test its own patients
3/11:
WHO declares a pandemic
3/12:
Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, calls the U.S.’s testing response “a failing”
3/12:
California Governor Gavin Newsom relaxes the certification requirements for clinical testing labs, giving the Biohub team the green light to begin building an extension of UCSF’s clinical lab
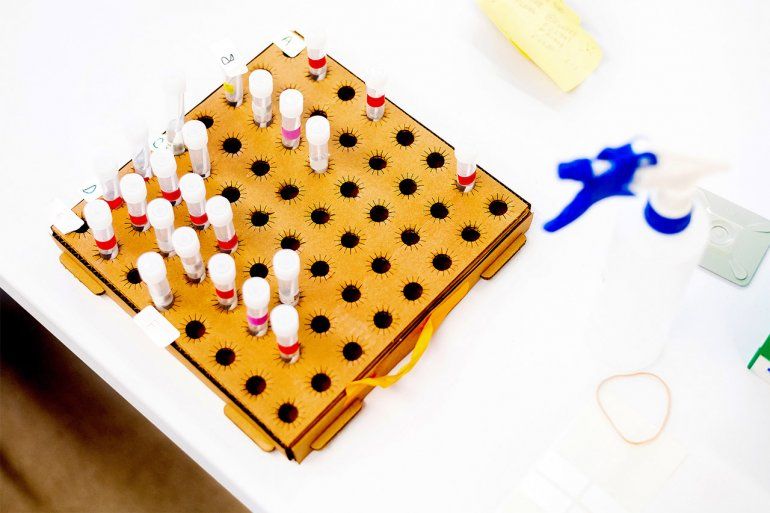
The COVID testing lab at the Biohub, an extension of UCSF's clinical lab, has the capacity to process more than 2,500 patient samples a day. UCSF offers testing free of charge to all California county public health departments thanks to this additional capacity and support from the Chan Zuckerberg Initiative.

Elizabeth McCarthy, an MD/PhD student at UCSF, handles patient samples. When the pandemic hit, more than 200 students and fellows volunteered to work in the testing lab.
As soon as DeRisi heard about Newsom’s order, he relayed the news to his task force. Its members were huddled in a conference room, still planning research projects. “Joe came in and said, ‘OK, this is happening. We’re going to transition over and do testing,’” recalls Emily Crawford, PhD ’12, whom DeRisi and the other Biohub brass had appointed as the task-force lead. “I was shocked,” she says. “I remember calling my mom late at night and being like, ‘This is totally insane.’” Then she thought, Bring it on.
“The first thing I did was understand I could not be in charge of everything, because it’s overwhelming and no one can do that,” Crawford says. She asked Vida Ahyong, PhD ’15, a research scientist at the Biohub who had spearheaded the IDseq project in Cambodia, to be her co-lead. Together, they recruited dozens of volunteers and organized them into subteams. One team would source supplies, another would oversee equipment, another would deal with patient samples, another would design the data system, another would manage lab waste, and so on. There were 13 teams in all. Everyone worked in pairs; that way, if someone contracted the virus, their partner could take over.

Joe DeRisi poses with Vida Ahyong, PhD (left), and Emily Crawford, PhD, research scientists at the Biohub who co-led the building of the testing lab.
The teams jumped into action. “It was a mad push,” DeRisi recalls. “Literally the lab was empty on March 12, and on March 13 we began carting in equipment from labs down the street at UCSF. It was raining, and there we were, hauling $80,000 robots down the 16th Street bike lane.”
By March 16, most of the pieces were in place. Under Miller and Thornborrow’s guidance, the teams had worked out a protocol for handling patient samples. They had bought, borrowed, or built themselves machines for processing the samples – and had named them Batman, Woody, Milo, Nico, Cat, Beyoncé, J-Lo, and Shakira. They had stockpiled supplies for running the machines: gloves, masks, vials, trays, and chemical reagents. They figured they would need another week or two to make sure everything was working smoothly and get the paperwork off to the U.S. Food and Drug Administration (FDA) for certification. And then UCSF’s chancellor called.
Since the start of the pandemic, Sam Hawgood, MBBS, had kept in close touch with DeRisi and the Biohub team, cheering them on and helping remove political obstacles. But as cases of COVID outside China swelled – first in Italy; then in Iran, South Korea, and Japan – Hawgood worried a wave would hit San Francisco before the testing lab was ready. “It was clear we were headed into trouble,” he recalls. “I had an intense sense of urgency that we needed to do everything we could not to get overwhelmed; days mattered, even hours.” Hawgood, UCSF’s Arthur and Toni Rembe Rock Professor as well as its chancellor, urged DeRisi to speed up the timeline.
There we were, hauling $80,000 robots down the 16th Street bike lane.”
“At that point, we were all thinking we still had over a week left,” Ahyong recalls. “Then it was, ‘Just kidding, you have 48 hours.’” The next two days, she says, “were a very big blur. It was all adrenaline. Everyone was like, ‘Who cares about sleep anymore? Let’s get this done.’”
It was nearing midnight on Wednesday, March 18 – only six days after they got the go-ahead to start building the testing facility – when they ran the final validation check to prove the lab met the FDA’s criteria for certification. “We were sitting around with our fingers crossed,” Ahyong says. “When the experiment finished and we saw the report, we literally jumped for joy.” Two days later, they ran their first patient samples. “We were so tired. We were so happy.... We were live.”
The jubilation didn’t last for long. By April, the Biohub team had scaled up their operation and trained enough student workers to handle more than 2,500 tests a day. But hardly anyone was sending in samples. It was a busy day if they got more than 250. “For a few weeks, we were like, ‘Well, we’ve built this, and nobody came,’” Miller says.
As soon as DeRisi heard about Newsom’s order, he relayed the news to his task force. Its members were huddled in a conference room, still planning research projects. “Joe came in and said, ‘OK, this is happening. We’re going to transition over and do testing,’” recalls Emily Crawford, PhD ’12, whom DeRisi and the other Biohub brass had appointed as the task-force lead. “I was shocked,” she says. “I remember calling my mom late at night and being like, ‘This is totally insane.’” Then she thought, Bring it on.
“The first thing I did was understand I could not be in charge of everything, because it’s overwhelming and no one can do that,” Crawford says. She asked Vida Ahyong, PhD ’15, a research scientist at the Biohub who had spearheaded the IDseq project in Cambodia, to be her co-lead. Together, they recruited dozens of volunteers and organized them into subteams. One team would source supplies, another would oversee equipment, another would deal with patient samples, another would design the data system, another would manage lab waste, and so on. There were 13 teams in all. Everyone worked in pairs; that way, if someone contracted the virus, their partner could take over.

Joe DeRisi poses with Vida Ahyong, PhD (left), and Emily Crawford, PhD, research scientists at the Biohub who co-led the building of the testing lab.
The teams jumped into action. “It was a mad push,” DeRisi recalls. “Literally the lab was empty on March 12, and on March 13 we began carting in equipment from labs down the street at UCSF. It was raining, and there we were, hauling $80,000 robots down the 16th Street bike lane.”
By March 16, most of the pieces were in place. Under Miller and Thornborrow’s guidance, the teams had worked out a protocol for handling patient samples. They had bought, borrowed, or built themselves machines for processing the samples – and had named them Batman, Woody, Milo, Nico, Cat, Beyoncé, J-Lo, and Shakira. They had stockpiled supplies for running the machines: gloves, masks, vials, trays, and chemical reagents. They figured they would need another week or two to make sure everything was working smoothly and get the paperwork off to the U.S. Food and Drug Administration (FDA) for certification. And then UCSF’s chancellor called.
Since the start of the pandemic, Sam Hawgood, MBBS, had kept in close touch with DeRisi and the Biohub team, cheering them on and helping remove political obstacles. But as cases of COVID outside China swelled – first in Italy; then in Iran, South Korea, and Japan – Hawgood worried a wave would hit San Francisco before the testing lab was ready. “It was clear we were headed into trouble,” he recalls. “I had an intense sense of urgency that we needed to do everything we could not to get overwhelmed; days mattered, even hours.” Hawgood, UCSF’s Arthur and Toni Rembe Rock Professor as well as its chancellor, urged DeRisi to speed up the timeline.
There we were, hauling $80,000 robots down the 16th Street bike lane.”
“At that point, we were all thinking we still had over a week left,” Ahyong recalls. “Then it was, ‘Just kidding, you have 48 hours.’” The next two days, she says, “were a very big blur. It was all adrenaline. Everyone was like, ‘Who cares about sleep anymore? Let’s get this done.’”
It was nearing midnight on Wednesday, March 18 – only six days after they got the go-ahead to start building the testing facility – when they ran the final validation check to prove the lab met the FDA’s criteria for certification. “We were sitting around with our fingers crossed,” Ahyong says. “When the experiment finished and we saw the report, we literally jumped for joy.” Two days later, they ran their first patient samples. “We were so tired. We were so happy.... We were live.”
The jubilation didn’t last for long. By April, the Biohub team had scaled up their operation and trained enough student workers to handle more than 2,500 tests a day. But hardly anyone was sending in samples. It was a busy day if they got more than 250. “For a few weeks, we were like, ‘Well, we’ve built this, and nobody came,’” Miller says.
3/13:
President Trump declares a national emergency
3/16:
Bay Area counties issue the first shelter-in-place orders in the U.S.
3/18:
The Biohub’s testing assay passes the final validation check for FDA certification
3/20:
The Biohub lab processes its first patient samples

Elizabeth McCarthy (center) labels incoming samples with fellow UCSF students Allison Wong (left) and Valentina Garcia.

Valentina Garcia (right) examines patient sample tubes with Paula Hayakawa Serpa, a lab technician at UCSF.
One reason was that the surge of hospitalizations everyone had expected didn’t hit San Francisco, a fact that experts attributed to the city’s early shelter-in-place orders. Yet they knew the virus was still circulating. Hundreds of thousands of residents were waiting to know whether they could safely go back to school or work. So why weren’t they getting tested?
The answer, it turned out, was swabs. To test someone for COVID-19, you need a swab – basically, a long, sterile Q-tip – to sample their nasal passage for the presence of the virus. But swabs, the Biohub team learned, were in short supply. “We’re talking about a global pandemic,” Thornborrow says. “Every country in the world was having a mad rush on nasal swabs.” Making matters worse, the outbreak in Italy had shut down the world’s main swab factory.
“It was baffling,” says Madhura Raghavan, PhD, a UCSF postdoctoral fellow who helped build the testing lab at the Biohub. “We had all this expensive equipment, we had all this manpower, but we were limited by this tiny little swab.”
So the UCSF and Biohub teams went in search of more swabs. Chancellor Hawgood got in touch with Marc Benioff, a longtime UCSF donor who, as CEO of the cloud computing firm Salesforce, had extensive business contacts in China. “Salesforce had boots on the ground in China going from factory to factory,” Thornborrow says. “They’d send me pictures of package inserts or advertisements for swabs and ask me, ‘Will this work?’” Eventually, they found some reputable suppliers and ordered hundreds of thousands of swabs to be distributed to hospitals, county health departments, and whoever else needed them.
Meanwhile, UCSF and the Chan Zuckerberg Initiative (CZI), the couple’s philanthropic venture, announced that – thanks to the Biohub expansion – UCSF would provide free testing to all 58 county health departments in California. Fearing equipment shortages and backlogs at commercial labs, many health departments had issued restrictive testing guidelines and held back on community testing. After UCSF and CZI’s announcement, however, more and more patient samples began showing up at the Biohub – and not just from hospitals, but also from nursing homes, homeless shelters, jails, prisons, and research teams surveying underserved or especially vulnerable communities. [See “An Epidemic of Inequality”.] By early May, the lab was running at near capacity.
“They’re the real deal,” says Paul Bayard, MD ’90, MPH, the chief medical officer for La Clínica, a network of community clinics in Alameda, Contra Costa, and Solano counties. Bayard started sending samples to the Biohub after becoming fed up with waiting up to two weeks for test results from a commercial lab. “Every day a patient doesn’t get a result multiplies the opportunity for the virus to spread,” he says. But with the Biohub turning around quality tests within one to two days, La Clínica was able to offer drive-through testing and do contact tracing so that family members, roommates, and co-workers could know if they should get tested, too. And because the tests were free, people who were uninsured or undocumented didn’t have to worry about whether they could afford them.
Eliminating such barriers to testing has become a point of pride for the Biohub team. “We’ve managed to not only keep ahead of the volume at UCSF but also help expand testing for the entire state,” Thornborrow says. “I don’t think that would have been possible without the work and support of so many people. It was definitely one of those ‘it takes a village to test a village’ kind of things.”
One reason was that the surge of hospitalizations everyone had expected didn’t hit San Francisco, a fact that experts attributed to the city’s early shelter-in-place orders. Yet they knew the virus was still circulating. Hundreds of thousands of residents were waiting to know whether they could safely go back to school or work. So why weren’t they getting tested?
The answer, it turned out, was swabs. To test someone for COVID-19, you need a swab – basically, a long, sterile Q-tip – to sample their nasal passage for the presence of the virus. But swabs, the Biohub team learned, were in short supply. “We’re talking about a global pandemic,” Thornborrow says. “Every country in the world was having a mad rush on nasal swabs.” Making matters worse, the outbreak in Italy had shut down the world’s main swab factory.
“It was baffling,” says Madhura Raghavan, PhD, a UCSF postdoctoral fellow who helped build the testing lab at the Biohub. “We had all this expensive equipment, we had all this manpower, but we were limited by this tiny little swab.”
So the UCSF and Biohub teams went in search of more swabs. Chancellor Hawgood got in touch with Marc Benioff, a longtime UCSF donor who, as CEO of the cloud computing firm Salesforce, had extensive business contacts in China. “Salesforce had boots on the ground in China going from factory to factory,” Thornborrow says. “They’d send me pictures of package inserts or advertisements for swabs and ask me, ‘Will this work?’” Eventually, they found some reputable suppliers and ordered hundreds of thousands of swabs to be distributed to hospitals, county health departments, and whoever else needed them.
Meanwhile, UCSF and the Chan Zuckerberg Initiative (CZI), the couple’s philanthropic venture, announced that – thanks to the Biohub expansion – UCSF would provide free testing to all 58 county health departments in California. Fearing equipment shortages and backlogs at commercial labs, many health departments had issued restrictive testing guidelines and held back on community testing. After UCSF and CZI’s announcement, however, more and more patient samples began showing up at the Biohub – and not just from hospitals, but also from nursing homes, homeless shelters, jails, prisons, and research teams surveying underserved or especially vulnerable communities. [See “An Epidemic of Inequality”.] By early May, the lab was running at near capacity.
“They’re the real deal,” says Paul Bayard, MD ’90, MPH, the chief medical officer for La Clínica, a network of community clinics in Alameda, Contra Costa, and Solano counties. Bayard started sending samples to the Biohub after becoming fed up with waiting up to two weeks for test results from a commercial lab. “Every day a patient doesn’t get a result multiplies the opportunity for the virus to spread,” he says. But with the Biohub turning around quality tests within one to two days, La Clínica was able to offer drive-through testing and do contact tracing so that family members, roommates, and co-workers could know if they should get tested, too. And because the tests were free, people who were uninsured or undocumented didn’t have to worry about whether they could afford them.
Eliminating such barriers to testing has become a point of pride for the Biohub team. “We’ve managed to not only keep ahead of the volume at UCSF but also help expand testing for the entire state,” Thornborrow says. “I don’t think that would have been possible without the work and support of so many people. It was definitely one of those ‘it takes a village to test a village’ kind of things.”
3/22:
UCSF and other major Bay Area medical centers call for donations of masks, gowns, and nasal swabs, setting in motion an outpouring of community and private-sector help to solve equipment shortages
3/26:
The U.S. leads the world in COVID-19 cases, with more than 80,000
4/2:
The Biohub lab scales up its testing capacity to 2,688 tests per day
4/2:
The pandemic has sickened more than 1 million people in 171 countries
4/16:
UCSF offers free testing to all California county public health departments, thanks to the Biohub lab and support from the Chan Zuckerberg Initiative
4/24:
California averages 16,000 tests per day; Governor Newsom says the state will need at least 60,000 tests per day in order to reopen
4/26:
The global death toll surpasses 200,000

Joe DeRisi chats with Vida Ahyong and Emily Crawford in the Biohub testing lab. Their team bought, borrowed, or built themselves machines for processing samples and stockpiled equipment and supplies.
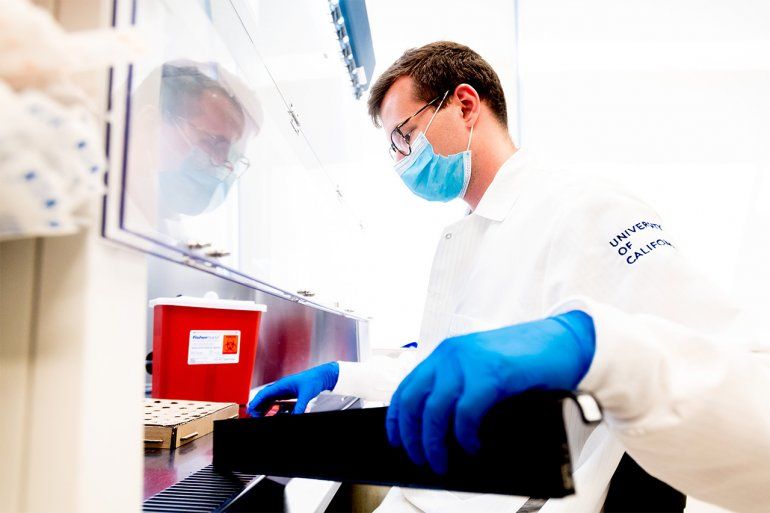
Alexander Merriman, a UCSF MD/PhD student, prepares sample tubes to be loaded into a processing machine.
These days, the Biohub’s COVID testing lab hums from morning to night. Samples are barcoded, logged, and prepared for processing. Machines are loaded with test tubes and plates. Reagents are added. Data are checked and results reported.
The speed and ingenuity with which the Biohub team brought this enterprise to pass is truly extraordinary, and its success has served as a model for other U.S. research institutions to create their own diagnostic labs. “We showed UC Berkeley how to do it; we showed UC Santa Cruz how to do it; we advised many, many people across the country,” DeRisi says. Together, these academic-turned-service labs paved a path forward at a time when the country’s inadequate testing capacity had tragically hampered its early pandemic response. “What we’ve learned is that universities and research centers like the Biohub have incredible, untapped potential to respond to emergencies in ways I don’t think this country has seen before,” DeRisi says.
In the meantime, the pandemic continues to spread, straining even the additional testing capacity the U.S. has managed to build piecemeal. Without a national strategy, local governments and health providers continue to make decisions about testing in isolation, competing with each other for workers and supplies. Many of the same bottlenecks that plagued this fragmented system at the start of the pandemic are beginning to reemerge, including shifting supply chains, backlogs at commercial labs, and long lines at testing centers.
Eventually, when the dust of the COVID storm settles, the Biohub team will return to its original mission, which includes hunting down pathogens in California, Cambodia, and other corners of the globe near and far. The student volunteers will resume their thesis projects, the borrowed robots will be marched back up 16th Street, and the clinical lab will be shuttered. For now, though, the team will continue churning out tests for as long as their service is needed – which, from the look of things, could be a very long time.
These days, the Biohub’s COVID testing lab hums from morning to night. Samples are barcoded, logged, and prepared for processing. Machines are loaded with test tubes and plates. Reagents are added. Data are checked and results reported.
The speed and ingenuity with which the Biohub team brought this enterprise to pass is truly extraordinary, and its success has served as a model for other U.S. research institutions to create their own diagnostic labs. “We showed UC Berkeley how to do it; we showed UC Santa Cruz how to do it; we advised many, many people across the country,” DeRisi says. Together, these academic-turned-service labs paved a path forward at a time when the country’s inadequate testing capacity had tragically hampered its early pandemic response. “What we’ve learned is that universities and research centers like the Biohub have incredible, untapped potential to respond to emergencies in ways I don’t think this country has seen before,” DeRisi says.
In the meantime, the pandemic continues to spread, straining even the additional testing capacity the U.S. has managed to build piecemeal. Without a national strategy, local governments and health providers continue to make decisions about testing in isolation, competing with each other for workers and supplies. Many of the same bottlenecks that plagued this fragmented system at the start of the pandemic are beginning to reemerge, including shifting supply chains, backlogs at commercial labs, and long lines at testing centers.
Eventually, when the dust of the COVID storm settles, the Biohub team will return to its original mission, which includes hunting down pathogens in California, Cambodia, and other corners of the globe near and far. The student volunteers will resume their thesis projects, the borrowed robots will be marched back up 16th Street, and the clinical lab will be shuttered. For now, though, the team will continue churning out tests for as long as their service is needed – which, from the look of things, could be a very long time.
5/12:
California scales up its testing capacity to 35,000 tests per day
5/27:
U.S. deaths surpass 100,000, far higher than any other nation
6/4:
The number of known cases worldwide grows faster than ever, with more than 100,000 new infections every day
6/28:
COVID-19 has sickened 10 million people and killed more than 500,000
7/7:
The U.S. hits 3 million total cases; California breaks its daily record with more than 9,000 new cases
7/21:
Today, the pandemic continues to accelerate; testing bottlenecks still plague much of the U.S.