Erin Fusco loves to visit Disneyland. She’s had an annual pass since she was 18 years old and has visited hundreds of times. But there was a stretch when her regular trips to the happiest place on earth were put on hold. When Fusco, now 37, was in her 20s, she was living in the Bay Area with her boyfriend, Adam, and working as an artist in the video game industry while running her own design business.
Life was good.
But when she was 27, Fusco started experiencing symptoms that seemed abnormal, such as acute stomach pain after eating; severe nausea after one glass of wine; and floating, white stools. Something felt off, but the doctors she consulted told her not to worry.
In 2018, at age 31, Fusco finally found a doctor who took her symptoms seriously and ran a series of tests, culminating in an MRI the following year. The image showed a mass on her pancreas. It would have to be biopsied, and Fusco’s doctor sent her to UC San Francisco for the procedure.

As Fusco was waking up at UCSF Medical Center, Barry Tong, MS, MPH, a genetic counselor with the UCSF Cancer Genetics and Prevention Program, was standing next to her bed with Adam, who was by then her husband, and her parents. Tong was there to talk with Fusco about genetic testing, which he said needed to be done immediately. The testing could disclose if she had a genetic mutation that could impact her treatment.
The biopsy revealed that Fusco had pancreatic ductal adenocarcinoma (PDAC), the most common form of pancreatic cancer, which has an average five-year survival rate of 12%.
“The second the surgeons confirmed that it was pancreatic cancer, they messaged the oncology team, who then messaged us to say, ‘Hey, we need genetic testing as fast as possible,’” recalls Tong. “So her blood was drawn while she was in the recovery room. I got consent from her partner and her parents, and I literally walked the sample down the street to a genetic testing lab five blocks away.”
Genetic testing was required to meet national guidelines and, due to Fusco’s young age, to rule out a genetic mutation as the cause of her cancer. Fusco was on board with the testing from the moment she was fully awake and discussing it with Tong.
“I was actually really excited to participate in [the genetic testing] and see if [it was] going to make a difference in my treatment,” Fusco says.
Uncovering the mysteries in our genes
At its most basic, genetic testing looks for changes – referred to as variants or mutations – in a person’s DNA that may affect their health, but that simple definition belies the far-reaching and extraordinary impact such testing has on health care and health outcomes. It’s almost a magic key that can unlock the body’s secrets. Genetic testing, which is typically done on blood or saliva, can alert individuals to hidden health risks – knowledge that can help patients make better-informed decisions and that can guide clinicians as to what treatment approaches and medications will be most effective – and we are still in the early days of this medical revolution.
Genetic testing can be integrated into every aspect of health care, from preconception through senescence.”
“Genetic testing can be integrated into every aspect of health care, from preconception through senescence,” explains Aleks Rajkovic, MD, PhD, chief genomics officer at UCSF and a Lindsay Professor of Experimental Pathology. While genetic testing already plays a pivotal role in diagnostics, Rajkovic says, “we are definitely in the early stages of taking an individual’s genome into account and using it to make preventive decisions about their health needs.”

Rajkovic says the cost of such testing has dramatically decreased over the years and now ranges from a few hundred to a few thousand dollars, depending on the depth and breadth of the analysis. Insurance coverage varies widely, though, which is a barrier to large-scale genetic testing. Additionally, genetic testing is more likely to be available at academic medical centers like UCSF than at smaller or rural facilities.
Genetic testing can be beneficial across the entire life span, beginning even before conception. Many people choose to have carrier screening done before they become pregnant or during pregnancy to learn whether they carry a genetic mutation for hereditary diseases such as cystic fibrosis or spinal muscular atrophy. If both parents are carriers of the same genetic disease, there’s a 25% chance that their children will have the disorder.
Next comes genetic screening and diagnostic testing, which is available to anyone who is pregnant. These tests look for inherited disorders and chromosomal abnormalities in the fetus that can cause conditions such as Down syndrome. In the past, prenatal testing was often associated with finding out the health status of a fetus in order to decide whether to terminate a pregnancy, but innovations in neonatal care – including gene therapies, stem cell transplantation, and intrauterine surgery – give parents today a far larger range of options, says Mary Norton, MD, the Thorburn Professor of Perinatal Medicine and Genetics at UCSF’s Prenatal Diagnostic Center.

Newborn screening is now standard for certain genetic, endocrine, and metabolic disorders, as well as for hearing loss and serious congenital heart defects. However, in critically ill babies for whom current testing can’t yield a diagnosis, rapid whole-genome sequencing is becoming the standard of care at UCSF and other academic medical centers, Rajkovic says. UCSF Health is the only system in Northern California to provide this test for both fetal and newborn patients.
Then, throughout our lives, predictive and presymptomatic testing can be used to determine whether we are predisposed to certain hereditary conditions – like cardiovascular disease, diabetes, or cancer, as well as genetic abnormalities – and to diagnose adult-onset genetic conditions like heart disease or diabetes.
Joyce So, MD, PhD, UCSF’s Epstein Professor of Human Genetics, points out that the availability and types of genetic testing have changed significantly over the lifetimes of today’s adults. “Even if they were seen as a child for something that was thought to be genetic,” she says, “if they didn’t have a diagnosis and they came back now for genetic evaluation, there’s a much higher likelihood that we would find a diagnosis because the testing has changed so much over the last 15 to 20 years.”

So works in psychiatric genetics, looking at the impact of rare genetic conditions on psychiatric and neurogenetic patients: that is, patients who appear to have a primary psychiatric condition but actually have an underlying genetic condition (such as DiGeorge syndrome or porphyria) that’s causing their psychiatric symptoms.
The effectiveness of many drugs, including psychiatric drugs, depends on our underlying genetic makeup. That’s where the field of pharmacogenetics – which screens patients for adverse reactions to certain drugs, as well as for differences in how they metabolize drugs, to guide prescribing and dosing recommendations – comes in. UCSF is the first hospital system in California and one of the first in the country to provide drug-gene testing. This is fast becoming a crucial part of health care, because adverse drug reactions are the fourth-leading cause of death in the U.S.
Tumor testing is another kind of common genetic testing. It’s done with certain cancers to aid in diagnosis; identify variants susceptible to drugs; predict progression, recurrence, and metastasis; and guide oncology treatments and therapeutics.
A guide on our genetic journey
Fusco says she didn’t know much about genetic testing – or genetic counseling – before Tong spoke with her in the recovery room. She had heard of the BRCA mutation, which is often associated with breast cancer, but “until I got the testing, I wasn’t really aware of it impacting my life at all.”
Norton explains that “genetic counseling is really an opportunity for patients to find out more about genetic testing before deciding whether or not to have it done.”
The purpose of genetic counseling is multifold, Tong says. One is gathering information about the patient’s personal and family history, determining the likelihood of a hereditary predisposition or hereditary risk of disease, and looking at the guidelines to determine whether genetic testing is appropriate.
“The counseling side of [genetic testing] in the pretest setting is talking with the patient about what the testing entails, what you learn, what you don’t learn, what the risks and benefits are, and helping the patient come to a decision whether or not they want to do the genetic testing – making an informed decision about it,” Tong says.
He adds that there are no medical risks to genetic testing. But testing could reveal information the person wasn’t seeking, there could be family implications, or the person might not be psychologically prepared for the information learned from the testing. This is why the third part of the process, interpreting and explaining the results to the patient, is so critical.

Amie Blanco, MS, clinical services director for the Cancer Genetics and Prevention Program, says that post-test genetic counseling is a process of shared decision-making and that the role of the counselor is particularly important when delivering a positive test result because information in a vacuum doesn’t necessarily lead to action.
“If our goal is to reduce the burden of cancer, we hope that patients take action on these positive test results to ultimately reduce their risk of cancer or find it as early as possible,” Blanco says.
“By building this relationship with patients through shared decision-making and motivational interviewing and other tools to really help patients feel supported in their decision-making processes, we hope to get patients to where they are taking the necessary steps to reduce their risks,” she adds.
This is one reason it’s important to distinguish between genetic tests ordered by a doctor and those offered by direct-to-consumer companies such as 23andMe. The direct-to-consumer commercial tests are far more simplistic than medical tests, and though some companies offer genetic counseling, the advice should be taken with a grain of salt.
“Sometimes the commercial laboratories will provide genetic counseling, but they obviously have a huge conflict of interest if [they] work for a lab to say you should have this test,” Norton says.
Further, commercial companies don’t usually offer clinician support or follow-ups. “So we end up with a lot of these patients who were given certain risks, and they want to know what to do with this information,” Rajkovic says.
And that leads to the subject of ethics.
The Genetic Information Nondiscrimination Act (GINA) prohibits health insurers from using genetic information to set rates or offer or withhold policies and prohibits employers from using it in employment decisions. But GINA’s protections don’t apply to long-term care insurance, life insurance, or disability insurance, nor do they apply to the military, which is allowed to use genetic information in employment decisions.
Nadav Ahituv, PhD, director of the UCSF Institute for Human Genetics, says an ethical dilemma can arise when genetic testing yields what’s known as a variant of unknown significance (VUS). These are variants that are quite rare and have not yet been connected to a health condition.
“So those are very hard to interpret, and [counselors] really try to make sure that if they provide results, they’re reliable,” Ahituv says.
Additionally, some members of minority groups are suspicious of genetic testing because of historical abuse of such information. The eugenics movement, for example, advocated selective breeding (once theoretical, but now possible). Bogus science has often been used to justify racism. Then there’s the case of Henrietta Lacks, a young Black woman whose cancer cells were taken without her consent in 1951. The cells were cultured, and what is now known as the HeLa cell line has been used in medical research ever since.
“As medical professionals, we must ensure that genetic testing is conducted ethically, equitably, and with sensitivity to the historical context that may affect trust among minority groups,” Rajkovic says. “Our goal is to make genetic testing accessible and fair for all individuals, irrespective of their ethnicity or race, and to actively address and work to overcome the barriers created by past misuses of genetic science.”
The ABCs of DNA: A Genetic Glossary
DNA
DNA is the molecular structure in every living thing containing that organism’s genetic code; it’s a long strand of nucleotides twisted into a double helix shape. Medical genetic testing doesn’t require visualizing DNA with microscopy but instead uses laboratory techniques and bioinformatics to analyze nucleotide sequences in specific, targeted regions on the strand.
Gene
A gene is a discrete segment of DNA that carries the information needed to make a specific protein. Each protein, in turn, directs a particular bodily function. Abnormal (or mutated) genes cause genetic conditions. Genetic testing is done when a specific gene or set of genes is suspected to be the culprit behind a disease.
Chromosome
Human genes are organized into 23 pairs of thread-like structures called chromosomes; we inherit one set of chromosomes from each parent. Some genetic conditions, such as Down syndrome, result when there are too many or too few chromosomes due to errors during cell division. In other cases, such as cystic fibrosis and sickle cell anemia, a mutation in a single gene on a specific chromosome can cause the disease.
Cell
A cell is the most basic unit of life. The process of genetic testing requires DNA to be extracted from the patient’s cells. First, a chemical reaction breaks down the cell membranes. Then the DNA is separated from the other cellular components through a series of purification procedures.
Genome
An organism’s genome is its complete set of DNA. Variations in our genome influence our risk of developing genetic diseases, as well as our responses to medications. Whole-genome sequencing involves analysis of an individual’s entire genome and can be done when the cause of a disease or disorder is unclear.
With knowledge comes power
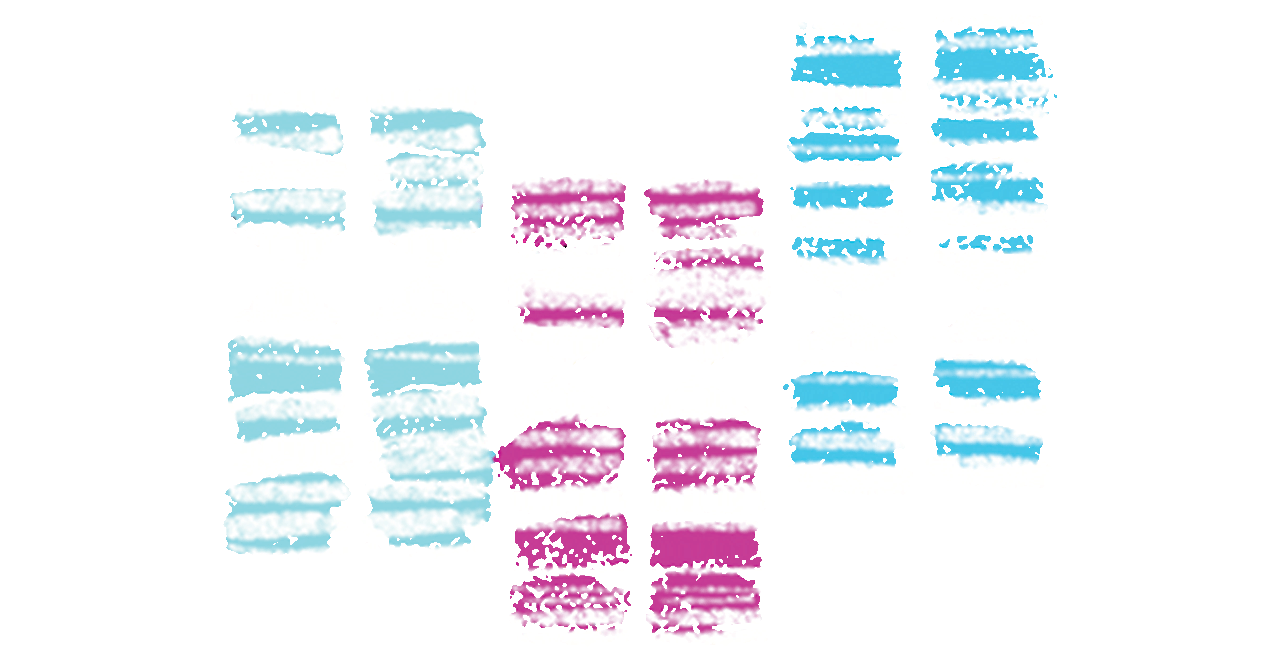
Eighteen days after Tong walked Fusco’s blood sample down the street, the results came back. Fusco, it turned out, has a BRCA2 mutation, meaning one of her BRCA2 genes doesn’t work properly. We all inherit two copies of the BRCA1 and BRCA2 genes, whose functions are to produce proteins that help repair damaged DNA and suppress cancer. People who inherit a mutation or variant in either BRCA1 or BRCA2 are at greater risk of developing several cancers, notably breast and ovarian, and of developing cancer at a younger age.
Tong says the mutation is the primary cause of Fusco’s cancer. After receiving the test results, he met with Fusco’s parents and then tested them, her brother, and her sister. Her father also has the BRCA2 mutation.
BRCA mutations are probably the most widely known among the public because a number of high-profile people who have them have gone public, including actors Christina Applegate and Angelina Jolie. Both women have a family history of breast cancer, and upon learning of their BRCA mutation, each woman had a double mastectomy. They opted for the surgery as a preventive measure, though only Applegate had breast cancer (and only in one breast).
Blanco says half of the Cancer Genetics and Prevention Program’s referral volume is patients who don’t have cancer but do have a family history of the disease. “And really, our goal here is to identify those patients that do have an inherited cancer risk and inherited gene mutation because then we can implement screening programs that can identify cancer as early as possible, and in some cases [implement] risk-reducing medications [or] surgeries to prevent cancer from happening altogether.”
Knowing that Fusco had the mutation was crucial to her treatment because there is data suggesting that BRCA-mutated cancers are more sensitive to certain types of chemotherapy. Fusco had six months of platinum-based chemotherapy, which has been shown to improve survival rates for patients with BRCA-mutated PDAC, before undergoing an operation called a Whipple procedure to remove her tumor and part of her pancreas. Following surgery, Fusco was cancer- free for nine months, but the cancer returned. Since then, she’s been on targeted chemotherapy and other standard-of-care treatments.
A genetic revolution
We are living in the midst of a genetic revolution, but it’s still in its infancy, and it has its limitations.
Ensuring equitable access to genetic testing remains a challenge. And currently, there is much more genomic information about people of European ancestry than of any other demographic group. In order for more people to benefit from the revolution, it’s essential for research studies to include more individuals of non-European ancestry.
Additionally, no one test can detect every genetic condition, nor is every test definitive. A negative result could mean that the wrong test was done, that there is not yet a test for that specific condition, or that there simply isn’t a genetic cause for the person’s illness.
It’s also important to remember that genetics is only one part of the health equation. “Genetics is not simple and does not in itself determine our health. Our health is a confluence of genetics, environment, education, socioeconomic status, and other variables,” Rajkovic says.
Still, countless people like Fusco have benefited from genetic testing – and there will no doubt be many more in the future.
After all, says Rajkovic, we understand only 1.5% of the genome that codes for proteins and even less about the noncoding part of the genome.
One area that is quickly gaining traction is epigenetics – the study of how behavior and environment can cause changes in the way our genes work. “Epigenetics is increasingly used to classify tumors and predict the course of cancer syndromes,” Rajkovic explains, adding that because epigenetic signatures are so specific to tissue and tumor type, companies are exploring ways to use them to screen individuals for cancer.
“Similar to how a Pap smear is used to detect precancerous or cancerous cells, there is a growing effort to use epigenetic markers to identify early signs of cancer elsewhere in the body. This could enable early detection and treatment, potentially improving outcomes for patients,” Rajkovic says.
This could revolutionize preventive health care, allowing for early detection and intervention for countless conditions. It can also lead to the development of whole new classes of therapeutics to prevent disease manifestations.”
Aleks Rajkovic, MD, PhD
Studies also are looking at the impact of sequencing the genomes of every newborn, thus creating a genetic passport that can be used during their lifetime. Rajkovic says the likelihood of such a practice increases as costs decrease and as the benefits of early intervention become clearer. However, he emphasizes that significant research is still needed to establish the clinical value of such an approach, particularly its ability to reduce suffering and bring about positive health outcomes. “To validate the effectiveness and benefits of creating genetic passports for newborns, a large-scale study will be necessary. We expect considerable developments in this area within the next decade. Success in this endeavor will likely require government support,” Rajkovic says.
“This could revolutionize preventive health care, allowing for early detection and intervention for countless conditions. It can also lead to the development of whole new classes of therapeutics to prevent disease manifestations,” he adds.
Five years after her surgery, Fusco says she’s doing well and taking things one day at a time. In 2020, she and Adam moved to Southern California, and Fusco got her dream job producing for the video game Diablo IV. Her current care team consults with her oncologist at UCSF, and she and Tong stay in touch through social media. Though she recently learned that her cancer is spreading, Fusco’s optimism hasn’t waned.
“I think the genetic testing has prolonged my life, absolutely,” she says, adding that her options for treatment continue to be state-of-the-art because of the genetic testing, and she is currently investigating clinical trials for targeted treatment. “Given everything I’ve been through, I mean, my life is awesome and I’m really glad to be alive still. So I kind of take the good with the bad.”
She adds that on her weekends off from chemotherapy, she and Adam go to Disneyland.