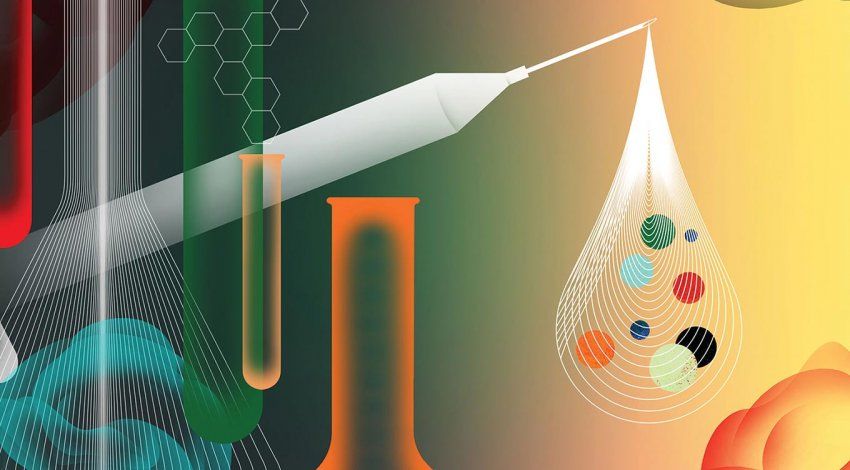
Generic Drugs: Are They on a Par with Pricier Brands?
Americans save billions of dollars using lower-cost generics instead of brand-name drugs. Are they as effective?
Animation: Farah Hamade
More than three-quarters of prescriptions in the U.S. are for generic drugs – off-brand medications that can cost less than half of their brand-name counterparts. Generic drugs saved Americans and our health care system over $300 billion in 2019 alone.
The use of generics has more than doubled over the past decade, thanks to legislation promoting generic-drug production and to the expiration of patents on widely used medications. Despite this enormous growth, myths about generics’ quality persist. UCSF drug safety experts help us understand what’s the same and what’s different, and whether brand should affect your choices.
MYTH #1:
Generic drugs are second-rate knockoffs.
Off-brand products like spaghetti sauce or facial tissue have often earned their reputation for being less good – they may taste mediocre or be less durable than the products they’re imitating. Consumers sometimes lump generic drugs in with second-rate knockoffs because of their cheaper price tags; there’s even skepticism among some providers.
It’s time to shake off this lingering myth once and for all. Generic drugs aren’t like other off-brand products, says Candy Tsourounis, PharmD, a professor of clinical pharmacy. They are in their own highly controlled category.
The myth of shoddiness may be reinforced by the way generics look, feel, or taste compared to brand-name drugs consumers are familiar with. That’s because inactive fillers, coatings, or liquids that help deliver the active ingredient – the actual drug – can vary.
“Many people view generics as somehow being inferior because of observable differences,” Tsourounis says, because generic manufacturers tweak these inactive components. This also explains why branded over-the-counter treatments like headache or allergy medications look different from over-the-counter generics. “For example, the brand name might be a tablet with a shiny coating that tastes nice and goes down easy, whereas the generic might be a chalky white pill with a bitter aftertaste.”
“Those differences exist, but the pharmacology – how the drug works in the body, the actual medicine it contains, and how long it takes to get to where it needs to be in the body – is the same,” says Tsourounis, who oversees UCSF Health’s medication formulary, the list of safe and effective medications approved for use within the institution. “Those are the most critical pieces,” she says. “The rest is just aesthetics.”
MYTH #2:
Testing of generics is not as rigorous.
Generic drugs don’t go through the same testing protocols as name-brand medications, but there’s a good reason, Tsourounis explains.
“It’s not that the testing is less rigorous, but that it’s different,” she says. It takes eight to 12 years of research and development, including clinical trials, to ensure that a new drug is safe and effective. All the steps to bring a drug to market add up to major costs for the company holding the patent.
By contrast, generics are not new drugs. When the patent becomes available on an existing approved drug, a generic manufacturer simply purchases or produces the already developed, tested, and approved active component and formulates it into a tablet, capsule, or other delivery vehicle. “That timeline is months, not years,” Tsourounis says, so it costs far less to bring a generic drug to market. When multiple manufacturers produce the same generic drug, competition drives prices down further.
The FDA requires that generics contain the same active ingredient as the branded version, be the same strength and format (such as a tablet or capsule) and use the same delivery route (such as oral or injection). To prove that their formulations work like the original drug, generic manufacturers must meet strict requirements for bioequivalence, which means the medicine must be absorbed by the body and measurable in the blood at levels comparable, within a strict range, to those of the brand-name drug.
Tsourounis also points out that FDA regulations govern every detail of pharmaceutical manufacturing, from laboratory facilities to the training required for individuals who handle and package drugs.
Shalini Lynch, PharmD ’92, an associate professor of clinical pharmacy, co-authored a study that found generic-drug skepticism is higher among ancillary providers like nurses and physician assistants, who receive limited pharmacology training, than among physicians. “Additional training on specific concepts such as bioequivalence,” Lynch explains, “could … foster a better understanding of the generic approval process.”
MYTH #3:
Generics just don’t work as well as brand-name drugs.
Especially when people switch from a name-brand drug to a generic, they may experience modest changes. Tsourounis says to avoid jumping to the conclusion that the generic isn’t up to snuff.
“There’s a lot to evaluate before concluding that the generic drug is not working as well as the brand,” she says. Are there interactions with food or other medications that affect the way the drug is being absorbed? Is the person taking the medicine at the same time every day? When she hears complaints that a drug didn’t work as quickly or caused a side effect, “there’s generally no pharmacological reason for these impacts, so I look to other causes or possibly even a placebo effect based on these myths about generics not being as good,” she says.
Pharmacies stock both AB-rated generics – drugs with the highest bioequivalence assessments – and B-rated drugs, which still meet rigid FDA requirements but have slightly lower bioequivalence. B-rated generics may be better suited for initial use of a drug rather than replacing a name-brand version. While Lynch cautions that additional monitoring may be required for patients with conditions where small changes in blood levels could pose “immediate and serious risks,” she says that caveat is about individual situations and risk, not classes of drugs. Lynch and Tsourounis assert that it’s beneficial for all patients to talk with their physicians about generic drug options.
“The bottom line is that generic drugs provide the same active ingredient as the brand for a lower cost, and they should be used whenever appropriate,” Tsourounis says. “They’re good medicine.”