Take a pill. Get a shot. Use an inhaler. Apply a patch. Fast. Easy. But the journey from discovering and developing effective, precise medications to using them correctly and safely in patients is hardly fast and easy. Nor is it a straight shot. At every step along the way, UCSF School of Pharmacy scientists are challenging the status quo. Their efforts hold the possibility of stunning breakthroughs in how we prevent, treat, and cure disease. Here are some of the most difficult problems they’re solving – and how.
The Problem
Identifying potential new drugs is like trying to hit a target hidden inside a massively complex, constantly moving machine – with a single tiny arrow.
Our Solution
Explore molecular targets in daring new ways.
How can we keep the inner workings of our cells in check?
Inside each of our trillions of cells, thousands of proteins are busy maintaining a stable environment – doing everything from metabolizing nutrients to repairing genetic damage.
To convey signals or carry out chemical reactions, these cellular proteins change shape, folding into new configurations that activate other proteins to each do their specific jobs. But sometimes an important protein gets bent into the wrong shape, leading to a cascade of harmful protein-protein interactions – a process that can lead to disease.

Michelle Arkin,
chemical biologist
Michelle Arkin, PhD, co-director of the Small Molecule Discovery Center, has spent two decades uncovering details of this molecular interplay. By testing millions of molecules – with a particular eye for their influence on protein-protein interactions in test tubes – Arkin seeks to identify promising new drug candidates. She’s currently hot on the trail of P97, a protein that’s central to interactions which, if they go awry, can cause a variety of conditions, from neurodegenerative diseases to cancers. Illuminating P97’s role may lead to new therapies for those conditions.
How can we make drugs side-effect free?
Drugs that treat psychiatric diseases work by influencing neurotransmitter receptors. These are brain proteins – typically found in the spaces, or synapses, between nerve cells – that convey signals from one nerve cell to another. Many psychiatric drugs affect several types of these receptors, meaning they can cause not only the desired therapeutic effects, such as the alleviation of anxiety, but also undesired side effects, such as insomnia.

Brian Shoichet,
computational chemist
Brian Shoichet, PhD ’91, is using 3-D models of individual neurotransmitter receptors to design drug-like molecules that fit only into specific receptors – with the aim of alleviating side effects. He and his team recently discovered a highly selective molecule that activates a dopamine receptor subtype called D4. This finding holds promise for the development of medications to treat addiction and psychosis that don’t induce the movement disorders commonly associated with many of today’s psychiatric drugs.
Can a new point of view turn a drug discovery failure into success?
Decades ago, scientists noticed that cancer cells produce signals that promote tumor growth. They tried blocking some of those signals with a class of drugs known as PI3K inhibitors. The result? Tumors stopped growing – but only in petri dishes and animal models. In clinical trials, the drugs totally failed to extend the lifespans of cancer patients – so PI3K inhibitors were shelved.

Sourav Bandyopadhyay,
systems biologist
Sourav Bandyopadhyay, PhD, wondered how such promising drugs could have stumbled at the finish line. Using a new technology that he developed, he measured the levels of all the different signals present in tumor cells and found that a handful of signals changed in response to PI3K inhibitors, allowing cancer to compensate for the effects of the drugs. Combining PI3K inhibitors with other drugs that block these additional signals led to an even more dramatic decrease in tumor growth in animal models, compared to PI3K inhibitors on their own. He’s now exploring ways to test this new combination therapy in clinical trials, making good on the therapeutic promise of one of cancer biology’s earliest discoveries.
The Problem
Drugs travel through our bloodstreams into every corner of our bodies – both where they’re needed and where they’re not – and can cause potentially dangerous side effects in healthy tissues or organs.
Our Solution
Get drugs to exactly where they’re needed.
How can we make sure drugs affect only sick cells and not healthy ones?
Chemotherapy drugs attack fast-growing cancer cells, but these drugs are not discerning; they attack fast-growing healthy cells, too. Luckily, tiny functional differences separate healthy cells from cancer cells. By finding and exploiting those differences, it may be possible to create molecular machines that set out to find sick cells, infiltrate them, and only then release the drug, thus sparing healthy tissues. Because cancerous cells have abnormal amounts of free-floating iron, Adam Renslo, PhD, co-director of the Small Molecule Discovery Center, realized cancer drugs could be improved by inserting them into molecular envelopes that require the presence of iron to open.

Adam Renslo,
medicinal chemist
Renslo’s method lays the groundwork for treatments that reach only cancerous cells, allowing health care providers to use smaller doses of cancer-fighting medicines and still achieve the same therapeutic effect – but with fewer side effects – compared to existing methods of chemotherapy delivery.
How can we design molecules nimble enough to negotiate the body’s obstacle course?
Our bodies control which substances can enter our tissues, whether the destination is an organ like the brain or a specific type of cell. When designing a potential new drug for a given disease, scientists must ensure that it is physically capable of both penetrating the body’s defenses and being accepted by its target once it arrives. Matthew Jacobson, PhD, is working to overcome this challenge using novel molecules called peptide macrocycles, which are capable of penetrating the biological membranes that separate tissues and cells. For all their girth, macrocycles are especially nimble.

Matthew Jacobson,
physical chemist and MacWilliam Distinguished Professor
Jacobson’s approach involves engineering small “hinges” into macrocycles, allowing them to fold into specific shapes to pass through the body’s various barriers. He’s shown how tweaks to a class of these molecules can be used not only to ensure their passage through the gut and into the bloodstream, but also to improve their ability to inhibit a certain receptor, called CXCR7, that plays important roles in the development of heart disease and cancer.
How can we pinpoint and control drug delivery over time?
A good drug is less than ideal if it’s hard to use. Nanotechnology-based drug delivery vehicles, placed inside the body, can eliminate the need for patients to administer drugs themselves on a tight schedule. These vehicles can also deliver drugs continuously, maximizing their effectiveness. Anti-glaucoma drugs are a case in point. Glaucoma is currently treated using liquid drops that reduce pressure in the eye, but elderly patients struggle to administer the drops correctly and on the right schedule.

Tejal Desai,
bioengineer and Ernest L. Prien Professor
Tejal Desai, PhD ’98, has engineered a tiny implant that slowly releases a controlled amount of the pressure-reducing drug – from within the eye – sparing glaucoma patients from daily eye-drop regimens. And she’s applying the same concept to the prevention and treatment of HIV/AIDS as well. Compared to men, women experience a higher risk of contracting the HIV virus if they miss taking their preventive medications. The Desai lab is creating a biodegradable drug delivery device, that’s inserted under the skin, to solve this problem. This may help arrest the spread of HIV globally, especially among women.
The Problem
How we live varies as much as our biological makeups; both affect the outcome of drug therapies.
Our Solution
Take into account all the factors that can influence a drug’s effectiveness for each individual – from genetic heritage and lifestyle to age and weight.
How can we treat chronic pain without fueling opioid addiction in women living with HIV?
As the pharmacist for the UCSF Women’s HIV Program, Jennifer Cocohoba, PharmD ’01, creates and monitors individualized drug treatment regimens for her HIV-positive patients, many of whom have been affected by traumatic life experiences such as homelessness, drug addiction, sexual assault, or physical abuse. They’re at high risk of developing chronic pain, both because of these traumas and because of the painful conditions – like neuropathy or avascular necrosis – caused by HIV or the drugs used to treat it.

Jennifer Cocohoba,
clinical scientist and pharmacist
Alarmed by these facts, and by the rising national incidence of prescription painkiller overdoses in women, Cocohoba and her UCSF School of Nursing colleague Yvette Cuca Bromberger, PhD ’13, MPH, set out to learn more about these patients and their relationships to opioids. They’re asking patients about their dependence on opioids, perceptions of the drugs’ risks, and attempts to reduce their opioid use. Armed with initial research data, they hope to then design and test interventions to promote safe use of opioids for effective pain relief, especially for women living with HIV.
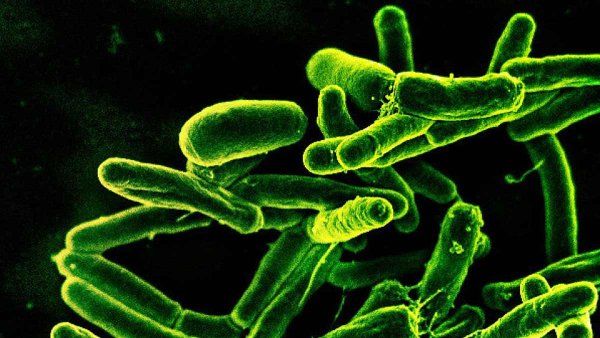
How can we use existing TB medications more effectively in individual patients worldwide?
Tuberculosis (TB) is curable and preventable, according to the World Health Organization. But it still kills nearly 2 million people a year, making it the deadliest infectious disease in the world. Rada Savic, PhD, thinks those deaths are unnecessary – and she knows how to prevent them. For decades, health care providers have treated TB using a standard six-month regimen of a handful of antibiotics, but Savic’s research has shown that this one-size-fits-all approach doesn’t work for all patients. Those who need treatment for less than the standard six months often end up bedridden for a few extra months due to side effects. And those who need treatment for more than six months can end up with recurring bouts of infection, which are more likely to be drug resistant – and deadly.

Rada Savic,
pharmacometrician
Based on patient data already collected by clinics worldwide – like X-rays, bacterial culture results, age, and nutrition status – Savic is confident that health care providers can successfully implement an evidence-based treatment plan for every patient, tailoring medication dose and frequency to each individual case. She’s optimistic that by following this course, the world may soon eradicate TB, once and for all.
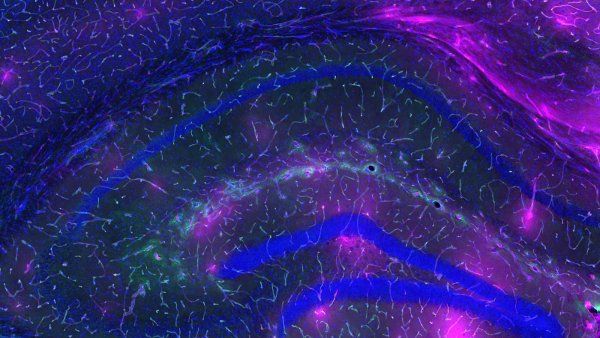
How can we leverage the unique genetic ancestry of each individual to better treat patients with asthma?
Variations in our genetic ancestry, as well as in the social and environmental factors we’re exposed to, can affect how vulnerable we are to disease. Our genetic ancestry can also influence the safety and effectiveness of drugs we’re prescribed. This is shockingly true of asthma – the most common chronic disease in children in the U.S. – and the medications used to treat it.

Esteban Burchard,
physician-scientist and Hind Distinguished Professor
For the past 20 years, Esteban Burchard, MD, MPH, has been studying the causes of health disparities in children with asthma, focusing on Latino and African American children. In the U.S., Puerto Ricans and African Americans are three times more likely to die from asthma than Mexicans and non-Latino whites. In addition, they have the lowest response to albuterol, the most commonly prescribed asthma medication worldwide. Burchard, together with his School of Pharmacy colleagues Ryan Hernandez, PhD, and Nadav Ahituv, PhD, plus 12 other research teams from eight universities, set out to uncover why there are racial/ethnic differences in patients’ responses to albuterol.
The group investigated the entire genomes of 1,441 Puerto Rican, African American, and Mexican children with asthma who responded either very well or very poorly to albuterol. They recently uncovered genetic variants that may explain some of the differences, a discovery that is helping to clear the path to personalizing asthma treatments for minority children.
The Problem
Policy makers, awash with complex new medical information, face daunting challenges.
Our Solution
Provide them with evidence-based recommendations that prioritize patient health, safety, and access to treatments and diagnostic tests.
How can we better advance, approve, and monitor medical products?
The development and ultimate approval of new drugs – and the monitoring of drugs after they’re on pharmacy shelves – involve intense scrutiny and regulation by the U.S. Food and Drug Administration (FDA). This is necessary to ensure that medications are safe and effective. Developing the rules and tools to do this is a science in itself – a science that Kathy Giacomini, PhD, aims to improve as co-director of the UCSF-Stanford Center of Excellence in Regulatory Science and Innovation (CERSI).

Kathy Giacomini,
regulatory scientist and pharmacogenomicist
Giacomini is now leading a major research study looking at 400 of the many inactive ingredients in generic tablets, capsules, and syrups taken orally – ingredients such as coatings, binding agents, and thickeners – that, with the active ingredients, travel to patients’ intestines. There, the active ingredient is absorbed into the bloodstream by intestinal transporters. Do the inactive ingredients, which can make up 90 percent of a drug formulation, hinder how well their active companions are absorbed? She intends to find out. Her results may help the FDA better regulate any inactive ingredients that hinder absorption and ensure that generic drugs used by patients have equivalent biological effects, dose by dose, to their brand-name counterparts.
How can we drive health policy so that genetic testing and the information it reveals benefit patients?

Kathryn Phillips,
health services and policy researcher
Genetic tests on the market today hold the promise of health care tailored to each patient’s unique biology and situation. But Kathryn Phillips, PhD, knows there’s a wide gap between this promise and a patient’s ability to benefit from it. She’s methodically narrowing that gap by asking hard questions and revealing critical answers, in her role as director of the Center for Translational and Policy Research on Personalized Medicine (TRANSPERS). Her team there recently found that the use of, and insurance coverage for, genomic tests for developmental disabilities such as autism, vary greatly. Instead of benefiting from diagnoses based on genomic testing, many of the one in six children in the U.S. who are developmentally disabled end up on diagnostic odysseys lasting many years. Findings like this – which Phillips and her fellow TRANSPERS researchers then share with policymakers – are essential if personalized medicine is to benefit all patients equitably.
The Problem
It takes too long to get effective new treatments to patients.
Our Solution
Start incrementally and locally – then apply the best solutions broadly.
How can we keep patients from being readmitted to the hospital because of medication problems?
Not paying strict attention to your medications can have serious, even deadly, consequences. It’s estimated that one million emergency department visits and 125,000 hospital admissions are caused each year by medication issues (called adverse drug events) in outpatient settings. Marilyn Stebbins, PharmD ’88, is determined to change those statistics, beginning with patients who are transitioning from the hospital to home.

Marilyn Stebbins,
clinical scientist and pharmacist
In collaboration with UCSF Medical Center and Walgreens at UCSF, Stebbins recently launched what’s known as a meds-to-beds program – a voluntary research pilot program that delivers medications to a patient’s hospital bedside as part of the discharge process, then follows up with patients about their medications, post-discharge, via an automated phone call. Any answer by the patient to the automated call triggers a personal follow-up call by a nurse, or by a pharmacist if the call involves a medication problem.
While all discharged patients receive the phone call, the meds-to-beds patients also leave the hospital with their prescribed medications in hand. The results to date? All meds-to-beds patients studied transitioned to home with their medications and were taking their medications, as prescribed, once they were home. Stebbins plans next to look at readmission rates for these patients and determine whether the program has an impact on medication-related readmissions.
Can pharmacists expand how they serve patients’ medication needs?
Since 2013, state laws have begun empowering specially trained, licensed California pharmacists to practice as legally recognized health care providers. They can now order tests to monitor the safety and effectiveness of medications, and they can prescribe hormonal contraception, nicotine replacement therapy, travel medicines, and naloxone (which can reverse the effects of an opioid overdose). A subset of pharmacists, known as advanced practice pharmacists, can now also initiate, adjust, or discontinue medication therapy for patients, joining their pharmacist peers who’ve been practicing at this level for years under special physician practice agreements in health care facilities.

Lisa Kroon,
clinical scientist and Thomas A. Oliver Professor
Lisa Kroon, PharmD and resident alumna, was instrumental in implementing these laws, and she has now turned to researching their impact on patient care. Preliminary results of a recent study, which she led in partnership with the national Albertsons pharmacy chain, indicate that community pharmacists can serve as convenient access points for patients seeking hormonal contraception. The next step? Research to explore whether such access can help lower the incidence of unintended pregnancies. Her findings are shedding light on the impact of expanding pharmacist practice authority across the nation.
How can we make sure we have the medications patients need in our hospitals and clinics?
If you’re admitted to a hospital, the idea that the institution might run short of a medication you need – an antibiotic, a painkiller, an anesthetic – would probably not cross your mind. But since 2005, the number of drug shortages in the U.S. has quadrupled – in many cases impacting patient care, health outcomes, and costs. It’s a national issue that’s generally addressed with a short-term approach, by reacting to shortages rather than anticipating them.

Rosa Rodriguez-Monguio,
health economist
As director of the Medication Outcomes Center, Rosa Rodriguez-Monguio, PhD, is leading a collaborative research agenda – involving experts in pharmacy, medicine, health economics, informatics, policy, and precision medicine – to ensure safe, cost-effective, equitable, evidence-based medication use at UCSF Health. Her current study aims to unearth the root causes and effects of drug shortages. With these findings in hand, she then plans to develop a forecasting model for anticipating and preventing potential drug shortages long before they arise, a model she hopes could ultimately be applied across all UC health care settings.
How can we protect the public against poisonings?
Poisons are everywhere, from chemicals under the kitchen sink to toxic smoke in the air. Two million children, most of them under age 6, will swallow a poison this year in the U.S.
The statewide California Poison Control System (CPCS), administered by the School of Pharmacy, keeps busy responding to calls from the public and health care providers about exposures to poisons and actual poisonings. CPCS poisoning specialists provide free, expert treatment advice and referrals 24/7, every day, at 800-222-1222 – handling 250,000 calls each year. Fifty-one percent of these calls concern children.

Stuart Heard,
pharmacist and health services and policy researcher
CPCS Executive Director Stuart Heard, PharmD ’72, and his team are currently fielding an uptick in calls related to unintentional pediatric marijuana exposure due to legalization increasing the availability of marijuana edibles, such as cookies and candies. A recent exposure at a child’s birthday party in San Francisco brought 12 children and 9 adults to emergency departments, all with central nervous system effects and many with cardiovascular effects from inadvertently eating gummy candies laced with THC, the psychoactive ingredient in cannabis. Follow-up research by the CPCS concluded that health care providers should consider exposure to THC in children who show altered mental states and should test for it when there is probable cause.
As the CPCS continues to provide Californians with around-the-clock treatment advice in cases of exposure to poisons, the results of CPCS studies like this are also keeping health care procedures and policies in synch with emerging sources of potential poisonings.