Digital Health: Transformative Tech or Unfulfilled Potential?
Q&A with Linda Park, associate professor of community health systems at the UCSF School of Nursing
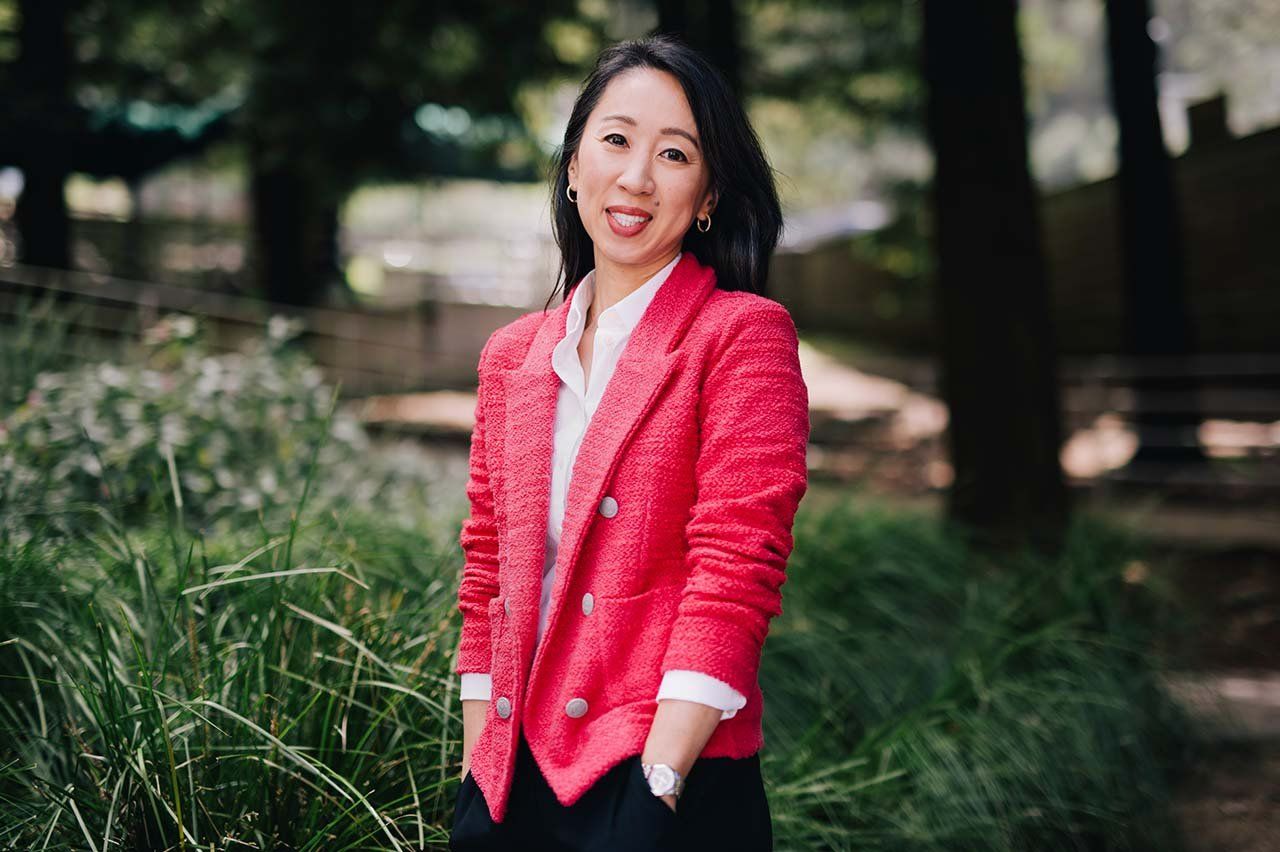
“Digital health” is an umbrella term that encompasses technologies ranging from electronic health records and telemedicine to fitness trackers and implantable medical devices. Linda Park, PhD ’13, NP, studies how health care providers can best use such tools to boost patient outcomes. Can digital health really make individuals, and even populations, healthier?
What are the biggest benefits of digital health?
Before, you were at the mercy of what your provider told you. You’d take a prescription and do your best. But digital health puts so much power in patients’ hands. The benefit really happens when people want to implement healthy behaviors, whether physical activity, medication adherence, or something else.
From the provider’s perspective, digital health is extremely efficient. There’s health monitoring that happens on patients’ cell phones and wearables, as well as more advanced technology like implantable sensors and devices. These give providers information that we wouldn’t be able to get otherwise.
How are digital health tools being successfully used today?
Telemedicine now provides patients with fundamental access to health care providers. The telehealth boom is here to stay.
Here’s a more complex scenario: I work in a cardiac catheterization lab at John Muir Health’s Concord Medical Center. Managing patients with heart failure is very complicated. They have one of the highest hospital readmission rates. There are implantable devices for remotely measuring pressure and volume and fluid status in the heart for advanced heart failure management. These digital health tools offer different passive ways of diagnosing conditions. If the numbers are off, a nurse can call the patient and say, “Why don’t you take an extra diuretic today?” We also have sensors that we implant into the chest wall to detect arrhythmias. Abnormal heart rhythms can otherwise be challenging to diagnose in real time when patients experience fleeting palpitations or pass out.
Digital devices can be as simple as blood pressure cuffs or weight scales. Those give us important data points. Using the data, though, is the challenge. These are valuable tools, but we have to do better at integrating them into the clinical decision-making process.
What about the health data collected by our smartphones and smartwatches? Are these data points helpful to clinicians?
I’ve heard over and over again from patients in the clinical setting that they identified their atrial fibrillation through their smartwatch. In this context, an electrophysiologist would want to see the rhythm tracings. But it is unlikely a clinician would ask a patient for their entire record of step counts.
But providers don’t yet have a way to merge all these insightful data points. Some health systems have tried to integrate data from wearables similarly to how glucometer and blood pressure data can be integrated: transmitting it directly to the electronic health record. But that’s the gold standard for the future; there’s no connection at this point.
Do digital health initiatives really make an impact on public health?
They can. One example that warms my heart is Text4baby, a free, national text-messaging program for people when they’re pregnant. (Text4baby texts subscribers timely, reliable information and resources about maternal and child health. A randomized study found that program participants were three times as likely to believe they were prepared to be new mothers as those in a control group.) It’s a positive model of what can happen with the simplest technologies. It’s not this flashy mobile app. You don’t even need a smartphone. Just a simple intervention has really improved things for moms and babies.
What worries you about digital health? What are the pitfalls?
Despite the investment, the potential to disseminate these technologies has not been realized. The secret sauce is being able to profit from them so health care systems will be incentivized to promote digital health.
A case in point is cardiac rehabilitation: Medicare never covered virtual home-based rehab – only facility-based rehab – until the COVID-19 public health emergency that ended in 2023. Too often, we realize the benefit of digital health but then backtrack because of reimbursement. It comes down to the payer and whether we figure out a pathway to profit. Analyzing the cost-effectiveness needs more focus. That’s the only way we’re going to get these products out there and get health care systems embracing them.
I also worry about access. There are millions of Americans without broadband internet, and many more in the rest of the world. That’s very limiting for rural communities and minority and low-resource communities. I definitely worry about leaving people behind.
What will it take for digital health to fulfill its potential?
Providers need to be invested in the possibilities and take the time to look at the data patients bring them. It will also take smart and innovative engineering and computer modeling. Patients need to be invested in managing and engaging with the technologies we give them. And payers need to realize the benefits of digital health, like keeping people out of the hospital and achieving better communication between patients and providers. It will take a village, but I think the future is very bright.