The Case of the Brain-Eating Amoeba
After diagnosing a middle-aged man with an incredibly rare and almost always fatal infection, a medical team led by UCSF fellow Natasha Spottiswoode raced to find a treatment that could save his life.

In the summer of 2021, an otherwise healthy man in his mid-50s had a sudden, unexplained seizure. After an MRI at his local hospital revealed a lesion on his brain, he was transferred to UCSF Medical Center for specialty care.
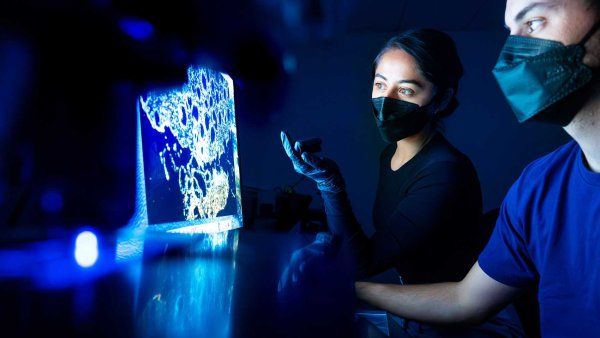
A biopsy ruled out most of the usual suspects, including cancer, bacterial or fungal infections, and tuberculosis. Then the UCSF team noticed a curious pattern in the biopsied tissue that made them think the problem might be an amoeba.
Single-celled amoebas commonly inhabit soil and water; occasionally, they can enter a human body through the nose, mouth, or skin and migrate to the brain. This happens so infrequently, though, that few medical centers in the U.S. are equipped to test for an amoeba infection. The UCSF team sent a sample of the biopsy to a specialized lab that confirmed their hunch: The man’s brain had been infiltrated by the “brain-eating” amoeba Balamuthia mandrillaris.
Such infections are nearly always fatal. And for the few Balamuthia survivors, there’s no clear evidence of what saved them. “It’s not a disease with a great deal of good data because it’s so rare and so deadly,” says Natasha Spottiswoode, MD, PhD, a UCSF infectious diseases fellow who helped care for the patient.
After consulting with the U.S. Centers for Disease Control and Prevention, the UCSF team started the patient on an intensive – and highly toxic – regimen of antibacterial, antiparasitic, and antifungal drugs based on what had been given to previous Balamuthia patients. But soon after, the man’s kidneys began to fail, and his blood sugar levels and white blood cell counts dropped dangerously low. So the team stopped giving him the most noxious medications. His brain lesions multiplied and grew as the amoebic infection spread.
In an urgent search for a better treatment, Spottiswoode scoured the medical literature. One paper in particular caught her eye: a 2018 report by UCSF researchers who, after another patient died from a Balamuthia infection, had been determined to find a cure. They screened more than 2,000 drugs looking for something that could beat the amoeba. Their lead candidate: nitroxoline.
The drug is prescribed for urinary tract infections in some countries but isn’t available in the U.S. However, the paper’s senior author, Joe DeRisi, PhD, pointed Spottiswoode to a manufacturer in China. She immediately contacted the company. “They were incredibly kind and helpful,” she says, and supplied the nitroxoline for free. After getting approval from the U.S. Food and Drug Administration for emergency use, her team had a potentially lifesaving treatment in hand.
The patient’s lesions began to shrink after he was on nitroxoline for one week, Spottiswoode recalls. After seven weeks, the team could see that the infection was clearing.
The patient is now home, and Spottiswoode’s team continues to monitor his progress. “There’s no road map,” she says. “He’s the first person to have been successfully treated with this drug for this condition – ever.”