Calling All Scientists to Fight the Next Pandemic
Q&A with Nevan Krogan, director of UCSF’s Quantitative Biosciences Institute

Nevan Krogan, PhD, is not one to think small. No, Krogan thinks big – such as when he gathered forces from around the globe in early 2020 to battle a fatal virus. Two years later, his team at UCSF’s Quantitative Biosciences Institute (QBI) netted a $67.5 million grant, the biggest ever awarded to UCSF by the National Institutes of Health (NIH), to unite scientists and the biomedical industry to speed treatments aimed at the world’s deadliest diseases. It seems a job he was born to do.
Why do you think QBI was selected for this huge challenge?
We are connectors. We connect different institutions at UCSF, around the United States, around the world. We connect governmental agencies with scientists. We connect scientists and nonscientists.
Is that unique?
Incredibly. Science is often very siloed, as are scientists. If you look at UCSF, there’s the cancer center, the neurodegeneration center, etc. But QBI shows what happens when you bring scientists together from different disciplines, when you use disease-agnostic technology to facilitate these connections. That’s where the big breakthroughs happen.
For example?
When the pandemic hit, we immediately looked at our worldwide map and said, “Who can we work with?” We had already established trust at the Institut Pasteur in Paris and at New York’s Mount Sinai Hospital, which has one of the best microbiology departments in the U.S. We turned to them, and away we went.
That is unusual?
Yes. We could move fast because we had built this worldwide network. Thank God we had a relationship with the Institut Pasteur, because they had the virus growing in a BSL-3 [biosafety level 3 laboratory] early in the pandemic. We didn’t have it here in San Francisco until later, and it was crucial for research.
All the work that we accomplished, as well as the NIH grant – none of that would have happened if we hadn’t laid the tracks before the pandemic with Institut Pasteur.
Seems like making connections comes easily to you. Is that a personality trait?
I think so. In science, I’m in the business of making connections between proteins. When QBI came to fruition, I hired Jacqueline Fabius as the COO. She is not a scientist; she worked at the United Nations. People said to me, “What? The UN?” I said, “We need somebody who can help facilitate relationships around the world.”
During the pandemic, people threw all the barriers out the window – and look how fast the world moved.”
How did these connections help during the early days of the pandemic?
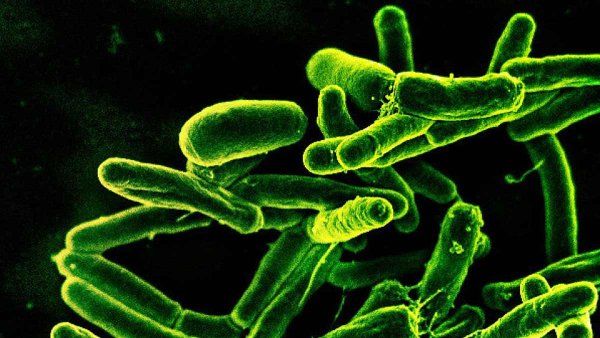
We were the first group in the world to clone all the genes for SARS-CoV-2, about 30 of them, in January 2020. We distributed them to over 400 labs in 40 countries in a couple of weeks, which helped expedite research on the novel coronavirus.
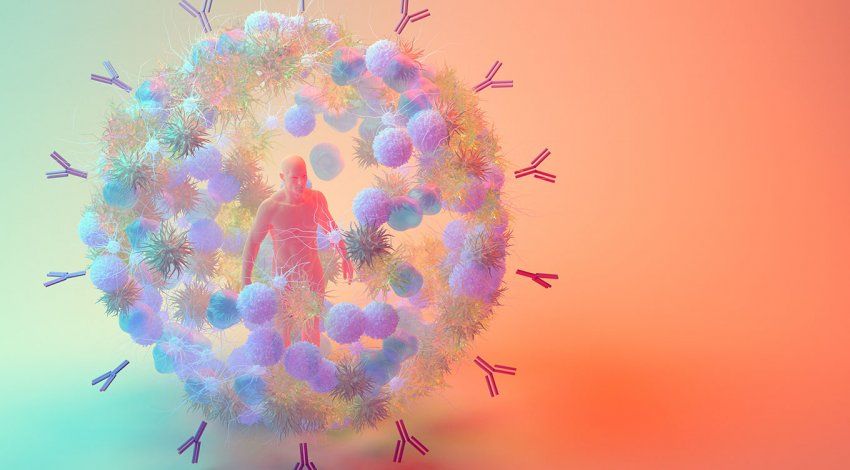
Next, we looked at what human proteins were touching the viral proteins, because the virus needs our proteins to live, to replicate, and to infect us. We identified about 300 proteins out of 20,000 human proteins that the virus was hijacking.
Then, in efforts led by QBI investigators Kevan Shokat and Brian Shoichet, we worked to find drugs already in clinical trials that targeted those proteins. We identified a whole slew, but two stood out: zotatifin and plitidepsin. Both are now in clinical trials to treat COVID-19. They’re anti-cancer drugs, by the way.
Did that surprise you?
No, it didn’t, because it comes back to science being siloed. When you look across disease areas, you see commonalities. It’s the same genes being mutated in cancer that SARS-CoV-2 is hijacking. It’s the same genes being mutated in autism that Zika is hijacking. It makes sense.
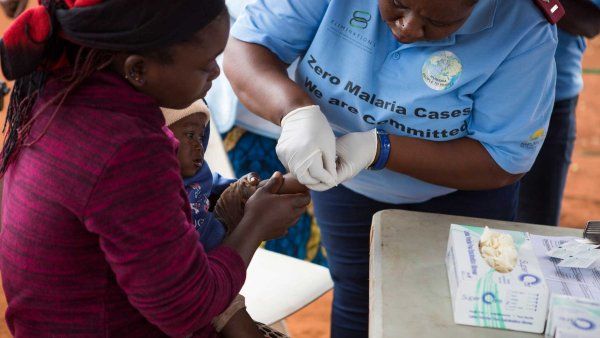
The NIH grant covers several deadly viral families – including Zika, measles, hemorrhagic fevers, and Ebola – all with pandemic potential. Will your team develop treatments?
Yes. During our COVID work, we built up an international collaboration among over 300 laboratories. We leveraged this network to include virologists with specialties in those diseases who are in London, New York, Paris. Half of the 43 labs on the grant are from QBI, and the other half are spread around the world.
Will this project revolutionize traditional drug development?
Going back to silos, I believe that this will force academics to think more about how their discoveries can be translated into treatments. I hope that this work will be revolutionary, that it will show us how to use our tools more effectively for drug discovery and show us all the value of partnering between academia and industry. That’ll have a much more profound impact than just targeting SARS-CoV-2. During the pandemic, a lot of people realized the value of relationships with pharmaceutical companies.
Before COVID, it wasn’t friendly?
Twenty years ago, not so much. During the pandemic, people threw all the barriers out the window – and look how fast the world moved. We didn’t even know about COVID a little more than three years ago. Now, we’ve got vaccines. We’ve got drugs. That’s unheard of in the biomedical world. Usually, it takes decades. It happened because everybody was collaborating – scientists, universities, pharmaceutical firms.
Now, as the dust settles – if it is settling from this pandemic – the question is: Can we learn from these lessons? Why aren’t we studying all diseases like this? Breast cancer, Parkinson’s, Alzheimer’s?
What do you think?
The vision was there before 2020. The pandemic was a huge tragedy. It was also a huge opportunity that we used for good. I truly believe that because of the pandemic, a couple of decades from now, we’re going to have many more treatments for diseases.
Wow. That’s because…?
We learned so much. The challenge is to make sure we implement the lessons going forward. Enough of us will. I believe the pandemic, in the long run, ironically, is going to save more lives than it cost.
Those are big words.
They are big words. We’ll see if they’re true.