Steven Mendoza was five weeks old when he first landed in the emergency room. His skin was dusky gray, his eyes were rolling back in his head. The doctors and nurses at Zuckerberg San Francisco General Hospital (ZSFG) swarmed around him, peppering his distraught parents with questions: Did he have epilepsy? Had he suffered some trauma? “No, no,” his mother, Fabiola Gudiel, responded. “No puede respirar!” He can’t breathe.

Fabiola Gudiel with her son, Steven Mendoza. Photo: Gabriela Hasbun
A flexible tube inserted into Steven’s trachea kept his airway open while he was rushed by ambulance to the pediatric intensive care unit at UC San Francisco Medical Center. He stayed there for seven days, recovering from a respiratory infection.
At age six months, after continued breathing problems, Steven was diagnosed with asthma. Treatment? That was trickier. Steven didn’t respond as well as hoped to a shifting array of medications, leaving him either exhausted and drowsy or hyperactive. He was also plagued by croup. The family’s one-room apartment in San Francisco’s Excelsior District was spotless, thanks to Gudiel’s housekeeping. But she couldn’t do much about the damp, dank carpeting or the cracked and strangely bulging walls.
“Before he even reached preschool, Steven had 11 episodes requiring oral corticosteroids in the hospital or urgent care. That’s unheard of,” says Kimberlee Honda, RN, MS, director of the ZSFG Pediatric Asthma and Allergy Clinic.
Steven is now four and a half years old. His survival is more than an example of lifesaving patient care. His case is also an illustration of UCSF’s compelling imperative to advance cutting-edge biomedicine and health equity for an increasingly diverse population.
Precision Public Health
“You can match a blood transfusion to a blood type,” President Obama said in announcing his Precision Medicine Initiative last year. “What if matching a cancer cure to our genetic code was just as easy, just as standard? What if figuring out the right dose of medicine was as simple as taking our temperature?”
“Precision medicine” is the starring attraction of today’s health care, with $215 million in federal funding and heady promises of transforming disease prevention and treatment by leveraging advances in genomics and data analysis.
With 15 publications on the subject and more than two dozen related research and development projects in the pipeline, UCSF is at the forefront of the precision medicine endeavor. In fact, the term was coined in a 2011 National Academy of Sciences report co-authored by several UCSF faculty, including Susan Desmond-Hellmann, MD, MPH, and resident alumna, while she was chancellor of the University. Her successor as chancellor, Sam Hawgood, MBBS, has identified precision medicine as a priority to strengthen the University’s impact on local and global health, economics, and innovation.
But even ardent fans of the approach caution that precision medicine could too easily become privileged medicine, undercutting another of the University’s foundational mandates: serving vulnerable populations.
“Precision medicine has the potential to be extremely expensive to develop and manage – and fraught with opportunities for voltage drops, losing patients along every step of the way,” says Dean Schillinger, MD, resident alumnus, chief of the UCSF Division of General Internal Medicine, and director of the Health Communication and Health Literacy Program at ZSFG’s Center for Vulnerable Populations (CVP).
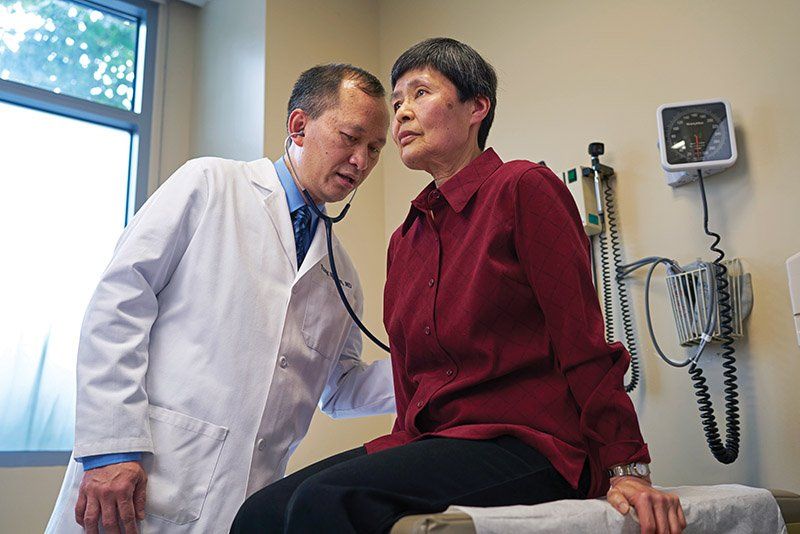
Physician Tung Nguyen (left) has conducted research on health disparities among African American, Asian American, and Latino patients. Photo: Steve Babuljak
To help navigate the tension between a low-cost, one-size-fits-all approach and individually tailored medicine, UCSF hosted a Precision Public Health Summit in June, convened by the White House Office of Science and Technology Policy and the Bill & Melinda Gates Foundation. A key takeaway: “Telescoping out” is as important as “telescoping down” to the genetic level.
“After taking into account our individual genetics, we have different behaviors; different social backgrounds; different places where we live, eat, pray, sleep,” says Sam Oh, PhD, MPH, an associate researcher at the UCSF School of Medicine and an epidemiologist at the UCSF Center for Genes, Environment, and Health.
Neighborhood is one key proxy for health disparities, indicating significant variations in air quality, housing, and social environment: “Depending on where you live, there are different stresses on you and your psyche and different risk factors for disease and response to treatment,” Oh adds. “It’s also about your interactions with law enforcement or how easy it is to access health care.”
Consider Oakland, where the number of African American men killed on its streets in the past decade nearly matched the number who graduated from its high schools ready to attend a state university, the San Francisco Chronicle reported.
In Pursuit of Health Equity
UCSF’s “tremendous depth” in epidemiological, genotype, and molecular research – together with the strong expertise in vulnerable patient populations of UCSF Benioff Children’s Hospitals and partners San Francisco Veterans Affairs Medical Center and ZSFG – uniquely positions the institution to foster a more holistic and equitable approach to both patient care and research, says Schillinger.
“It’s not just basic bench science,” he says, likening the effort to UCSF’s response during the AIDS epidemic in the 1980s, when he was chief medical resident at ZSFG. “When we tackled a problem like AIDS, it was understanding the virus, understanding the bathhouses, understanding mother-child transmissions.”
Indeed, what helped Steven Mendoza, the young asthma patient, as much as therapeutics was UCSF’s focus on social and environmental determinants around health.
Gudiel, now 39, moved to San Francisco from Central America 12 years ago and had never heard of asthma before her son’s diagnosis. ZSFG’s pediatric asthma clinic – a multidisciplinary collaboration that includes community health workers, behavioral health specialists, a nutritionist, and a lawyer – helped Gudiel became an expert in telling the difference between asthma symptoms and the barking cough of croup.
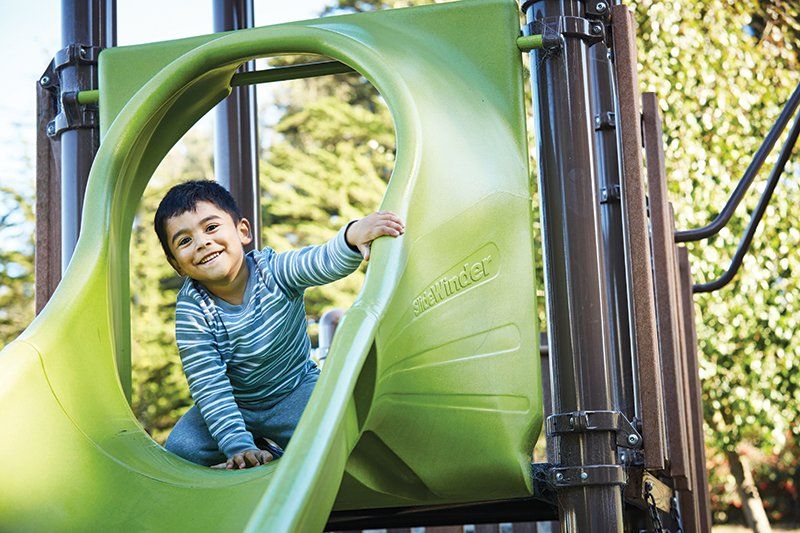
Under the care of ZSFG’s multidisciplinary team, Steven Mendoza has made many fewer trips to urgent care for treatment of his asthma. Photo: Gabriela Hasbun
She also learned about deadly environmental triggers for her son’s breathing problems: mold, dust, vermin, humidity, second-hand smoke. Gudiel asked the landlord to fix the walls and carpet in the family’s apartment, to no avail.
“It was disgusting,” Gudiel says in Spanish, with Silvia Raymundo, one of the clinic’s community health workers, translating. “The landlord would come and paint over the mold, but the wall would get inflated and crack, and you could see the mold again.”
In 2013, Raymundo visited the apartment, noting chipping paint, damaged window frames, and a severe mold infestation. The clinic wrote a letter to the landlord, requesting immediate remediation. Rather than make repairs, the landlord offered Gudiel and her family a different unit. They could barely afford the 20-percent rent increase – $300 a month – that came with it, but the move, along with fine-tuning Steven’s medication regimen, has paid off. This past year, the family’s frantic trips to urgent care were down by half.

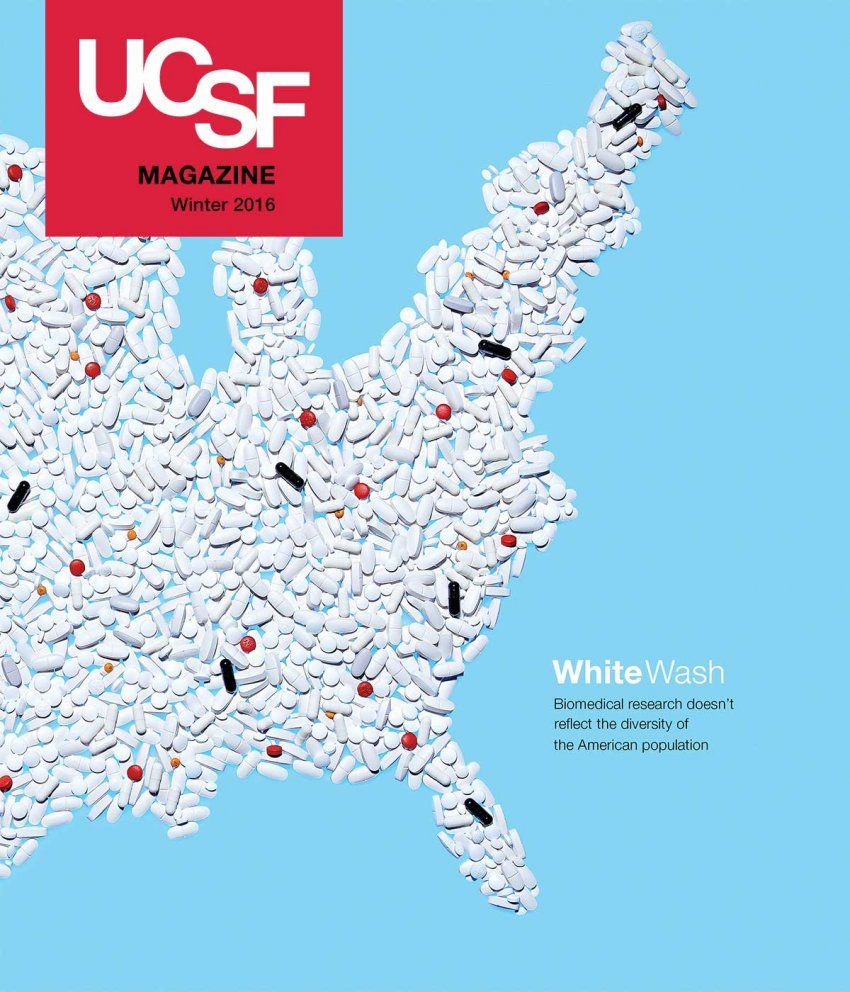
Photo Illustration: David Arky
Bridging the Research Diversity Divide
Luis (not his real name), a Salvadoran immigrant, was invited to participate in a UCSF clinical trial. He wasn’t interested. His cancer – initially misdiagnosed by a small-town clinic – continued to progress. His co-workers had to cover his shifts when he came to UCSF for treatment. He couldn’t afford to take more time off work and by that point was wondering if any doctor could help him.
Broader obstacles to recruiting participants for clinical trials – particularly minorities – include historical exploitation in medical research and cultural and language barriers. Even if the trial advances science, it rarely offers participants a cure.
But after two years, Luis changed his mind. “His energy was going, and he had lost a lot of weight,” says Daniel Dohan, PhD, a professor of health policy and social medicine and co-lead of the EngageUC initiative. “He had developed a strong relationship with his oncologist, and she again suggested a research study – for treatments that might help him feel better and help other people. That clearly appealed to him.”
With more than 1,400 clinical trials ongoing and more federal funding for biomedicine research last year than any other public university in the country, UCSF is one of the busiest health research institutes in the world. Increasing diversity in research is a top priority because it elevates both science and health equity. Here are three examples of the University’s multifaceted approach.
EngageUC: The University of California’s five medical centers serve a diverse patient population of about 13 million – one-third of the state’s population. To effectively investigate health needs and treatments at the genomic level, a long-term UC goal is to create a web-based repository of patient blood samples collected during clinical care. Step one is building transparency and community ownership for the project. Led by UCSF, EngageUC held in-depth focus groups this year to understand the cultural and trust issues around participation in a biobank.
Special Populations Initiative: A portion of an $85-million National Institutes of Health grant awarded to UCSF’s Clinical and Translational Science Institute will support a renewed focus on all aspects of patient-oriented research within and across low-income and minority populations, children, and the elderly. The initiative will leverage clinical and research expertise at UCSF Medical Center at Parnassus and Mt. Zion, Zuckerberg San Francisco General Hospital, UCSF Benioff Children’s Hospitals in Oakland and San Francisco, the Veterans Administration Hospital in San Francisco, and community partners.
Clinical Trials Finder: In the fall of 2016, UCSF launched a revamped user-friendly website for patients, their families, and referring physicians, with concise information about open clinical trials and, for those interested in participating, clickable links to contact investigators for further details. A grant application has also been submitted to extend the system UC-wide and translate it into languages other than English.
Reflecting America
Given UCSF’s goal of improving quality of life through research into health and disease, it’s an “absolute necessity” that research accurately reflects demographics, says Executive Vice Chancellor and Provost Daniel Lowenstein, MD, resident alumnus, and the Aird Professor of Neurology.
Science, Lowenstein says, has failed to meet that challenge for “a very, very long time.”
For decades, the vast majority of U.S. epidemiological studies reported on cohorts with very few women or even none altogether. The number of non-white participants? Even fewer.
Despite Congressional mandates aimed at diversifying clinical research and improvements in gender parity, little else has changed in the last 30 years: Since 1993, less than 2 percent of 10,000-plus National Cancer Institute-funded clinical trials and less than 5 percent of National Institutes of Health-funded respiratory studies have included enough minorities to be relevant. Those figures were published in PLoS Medicine in December 2015 by Oh and Esteban Burchard, MD, MPH, resident alumnus, and the Harry Wm. and Diana V. Hind Distinguished Professor in Pharmaceutical Sciences II.

Postdoctoral scholar Marquitta White (left) and Esteban Burchard (right), director of UCSF’s Asthma Collaboratory lab, are studying genetic and environmental influences on asthma in minority children. Photo: Noah Berger
With these diseases hitting minority populations at a disproportionate rate, and with drugs affecting people differently based on their genetic backgrounds, the lack of diversity in research is already having serious impacts on care for the nearly 40 percent of the U.S. population with non-European heritage. Additionally, health disparities cost the U.S. an estimated $300 billion a year in medical care, lost wages and productivity, family leave, and premature death.
“Generalizing results from research performed in one racial/ethnic group to another can work reasonably well, or it can have fatal consequences,” Burchard, Oh, and a co-author from Stanford wrote in a February editorial in the American Journal of Respiratory and Critical Care Medicine.
One striking example is asthma – the most common chronic disease among children worldwide. In the U.S., minority kids like Steven – his Nicaraguan and Salvadoran parents likely have a mix of Native American, Caucasian, and African ancestry – are at far higher risk of having asthma than their white peers.
Puerto Ricans and African Americans also tend to have more severe asthma that is harder to control with common drugs, and African American children die of asthma-related episodes at four times the rate of white children. Why? There haven’t been definitive answers, because almost all of the genetic studies of asthma have included only white patients.
Genetic vs. Race-Based Research
Burchard, as director of the UCSF Asthma Collaboratory, has spent 18 years collecting DNA samples of African American and Latino kids to study genetic and environmental influences on asthma. He now has more than 10,000 samples – the country’s largest such collection from minority children with asthma.
This treasure trove of data has led to several significant studies. One, led by Marquitta White, PhD, a postdoctoral scholar in the Asthma Collaboratory, recently identified both new genetic risk factors and the fact that only a tiny fraction of known factors for asthma apply to African American children – a crucial step toward improving diagnosis and treatment.
By recruiting people into genetic studies by race, however, Burchard and his colleagues have come under fire from critics pointing to a scientific legacy – like the infamous “Tuskegee Study of Untreated Syphilis in the Negro Male” – that has persecuted people of color rather than advancing their interests.
This country is plagued by racial and ethnic disparities in some of the most deadly diseases. The only way we will make progress in decreasing that burden of disease is by understanding why it occurs.”
Esteban G. Burchard, MD, MPH
“We look at genetic ancestry, at things we can measure. Racial and ethnic groups don’t have a basis in biology,” explains White, who identifies as African American and has African, European, and “a little block of Southeast Asian ancestry” in her genome.
“So many of us are from admixed populations,” she says, using the term for new genetic lineages introduced from the interbreeding of two or more previously isolated populations. “The percentages of those parent populations can affect susceptibility to disease or response to medication.”
Diversity in science is not just “science done well,” as Oh says. It’s also vital to health equity.
“This country is plagued by racial and ethnic disparities in some of the most deadly diseases,” Burchard says. “The only way we will make progress in decreasing that burden of disease is by understanding why it occurs. We can’t understand that without including diverse communities in our research.”