Behind makeshift orange fencing, the Ebola isolation unit in Bo, Sierra Leone, lies shrouded in a haze of smoke from the constant fires burning contaminated bedding and clothing. UC San Francisco physician Andrea Tenner, MD, MPH, looking like an astronaut in a head-to-toe protective suit, peers through foggy goggles as she reviews duty lists with local colleagues before entering the hot zone – the testing ward for patients with possible Ebola virus infection. She weaves her way through the labyrinth of protective barriers, ending up in the suspect ward, where patients who’ve exhibited Ebola symptoms anxiously await their test results.
Sierra Leone’s 90-degree heat and 80-percent humidity are oppressive enough in street clothes. But for those like Tenner, working long shifts intermittently clothed in the equivalent of high-tech plastic bags, the climate is almost unbearable. But she’s traveled thousands of miles from UCSF with a commitment to serve; bearing the heat is just part of the work Tenner came here to do.
Tenner spent almost three months in Sierra Leone last winter and spring, thanks to a university-wide effort allowing qualified personnel to respond to the Ebola epidemic. She is one of many UCSF faculty, staff and students who have volunteered their time and expertise during national and international medical crises.
From Earthquakes to Ebola
UCSF’s history of disaster response dates back to the 1906 San Francisco earthquake. While the city was still wracked with aftershocks, the university set up improvised outdoor hospitals in Golden Gate Park to aid the sick and wounded, plus temporary kitchens to feed the public. With that pioneering spirit, UCSF also started the first dedicated AIDS treatment clinic in 1983, a time when much of the world remained silent in the face of the epidemic.
In the past 20 years, globalization and variations in international responses have brought about dramatic changes in the approach to humanitarian crises and to the actions volunteers can take, especially in foreign countries. Formerly, experts rushed in to deliver hands-on care, often without considering the impact their presence and eventual departure would have on ongoing projects in the field. While the motivation behind the aid was admirable, its benefits often fell short of the goal; once volunteers headed home, local staff often found it impractical to sustain the level of care the visitors provided.

Andrea Tenner regularly travels to Africa on epidemic and disaster response assignments. Photo: Elisabeth Fall
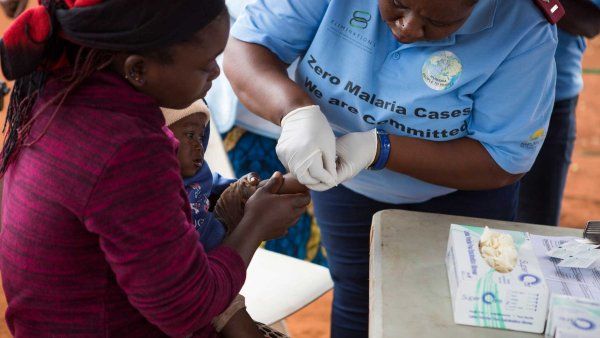
Today, the goal for both researchers and clinicians is not to throw U.S. expertise at indigenous crises and other global health challenges, but to respond by reducing the burden of disease while also empowering local leaders, strengthening local health systems, and leaving behind a sustainable model.
Currently, more than 470 UCSF faculty members are conducting ongoing research and training projects in 135 countries around the world. Hundreds more, like Tenner, step in when their specific skills are needed, volunteering to work with in-country partners and collaborate with international nongovernmental organizations like Médecins Sans Frontières, the International Rescue Committee, and many others. These efforts not only provide expertise, training, and capital to resource-limited populations, but also give UCSF faculty and students a chance to gain experience working in challenging settings.
The World Over
UCSF’s global disaster and medical response efforts focus on sustainability and cultural awareness, training local staff, strengthening existing health systems, and doing it all with sensitivity for local customs. Here is a sample of programs that further those goals:
- Global Health Sciences, established in 2003, was the first international research and service institute of its kind in the U.S.; it offers graduate and fellowship programs like the two-year HEAL Initiative, continuing education programs like Global Health Bootcamp, and an annual Global Health Summit.
- Global Health-Hospital Medicine Fellowship, a two-year program, offers training in teaching skills, quality improvement, patient safety, and systems improvement in resource-limited settings.
- School of Nursing Center for Global Health offers graduate coursework and a fellowship program, and supports research and medical response projects.
- Institute for Global Emergency Care, a collaboration between UCSF, the University of Cape Town, and Stellenbosch University in South Africa, advances emergency care in sub-Saharan Africa and strengthens health systems to increase their ability to respond to disasters.
- Global Health and Disaster Medicine Fellowships, Department of Emergency Medicine, offers one- and two-year programs in emergency response and response-system development.
Many domestic programs keep an eye on world events, too. A case in point is the California Poison Control System (CPCS), a service of the UCSF School of Pharmacy. Primarily a free statewide hotline for Californians exposed to poisons or toxins, the program shifts gears during public events involving exposure to nuclear, chemical, biological, or other noxious agents. For example, after the 2011 tsunami in Japan, the CPCS fielded over 150 calls from people concerned about radiation emissions from the Fukushima Daiichi nuclear plant.
The Essential Ingredients
No matter where or when a disaster or epidemic strikes, several factors are key to an effective response. Speed is one. UCSF Chancellor Sam Hawgood, MBBS, responded quickly in October 2014 to President Obama’s call for U.S. experts to help stem the Ebola epidemic in West Africa. He issued safety guidelines, coordinated training with federal agencies, and set up a vacation donation bank so qualified clinicians like Tenner could volunteer to go.
Flexibility is another key factor. “You can’t be a cowboy,” Tenner says of her experience in Sierra Leone, where she was unexpectedly asked to oversee three isolation units and coordinate patient triage. “Of course, this work is risky. But it’s a calculated risk. You have to do everything in your power to protect yourself and others. In a resource-limited environment, everyone has to do their part.”
You think you are ready, but every day brings something new. You do what you can with available resources, but in this environment, relieving pain and suffering is not always possible.”
In the Bay Area, Tenner is an assistant clinical professor of emergency medicine, director of the Department of Emergency Medicine’s Global Health Fellowship program, and an emergency physician at San Francisco General Hospital. Her training in infectious diseases and disaster preparedness primed her for the last-minute duty change and the tension of the hot zone. But, she adds, “You think you are ready, but every day brings something new. You do what you can with available resources, but in this environment, relieving pain and suffering is not always possible.”
Stamina, both physical and emotional, is also necessary. For example, those responding to the Ebola epidemic were directed to provide all care, from triage to treatment, without any direct patient contact. This “no-touch” policy was set after an unprecedented number of health care workers died from the disease. As well, wearing full protective gear is not tenable for long shifts and, as a result, explains Farrah Kashfipour, RN, MS ’14, “many patients die in pain, isolated from their families. It is the sad nature of the epidemic.” An alumna of the UCSF Global Health Sciences program, Kashfipour spent six weeks in Liberia providing patient care and training health care workers.

Phuoc Le, co-director of HEAL and the Global Health Core at UCSF, trains and mentors others in capacity-building. Photo: Elisabeth Fall
“No one wants this: not patients, not nurses, not doctors,” says Phuoc Le, MD, MPH, of the no-touch policy. Le, an assistant clinical professor of medicine and pediatrics, worked in Liberia at the height of the epidemic, unable to place a stethoscope on his patients’ chests, feel their abdomens for masses, or even shake their hands.
Additionally, demonstrating cultural sensitivity is critical. There is often tension between local customs – such as those obliging families to wash and prepare bodies for burial – and World Health Organization (WHO) infection-control guidelines. Balancing cultural sensitivity with disease containment isn’t always clear-cut – it’s individual to each situation. “How can you take the lessons learned from epidemics and disease response ... and apply that sustainably?” muses George Rutherford, MD, director of UCSF’s Prevention and Public Health Group and the Salvatore Pablo Lucia Professor of Preventive Medicine.
And ensuring that staff and volunteers are adequately trained is perhaps most important of all. UCSF’s HEAL Initiative (Health, Equity, Action, and Leadership) arose from recognition of that need. Le and the other co-founders of HEAL, who met while responding to the 2010 earthquake in Haiti, quickly realized the need to educate those who wanted to help but were unprepared to work in resource-limited settings.
“Health professionals have no business going into disasters or health crises without experience or training in disaster response and knowledge of how to work in resource-constrained settings,” says Le. “A doctor who can only perform with all the latest equipment is useless in an emergency response. Before you set foot in a disaster, you need to have training so you don’t cause harm and can be impactful and effective.”
This type of training prepares one to expect the unexpected. Le, for example, was asked in Haiti to coordinate patient care among 10 hospitals; it wasn’t what he’d anticipated doing, but it was what needed to be done. “Contributing to a direct need ... was extremely rewarding,” Le says. He also made house calls, an activity now embodied in HEAL’s philosophy of actively bringing care to the patient rather than waiting passively at the hospital.
One Size Doesn't Fit All
Unlike Haiti and West Africa, some places have an established medical infrastructure and prefer not to have an influx of foreigners descending upon the chaos. The April 2015 earthquake in Nepal, for example, called for a different response.

Bibhav Acharya co-founded the nonprofits Possible Health and Shared Minds in Nepal. Photo: Elen Shrestha
It was 3 a.m. on April 25 when Nepal native, Bibhav Acharya, MD, a UCSF assistant professor of psychiatry, learned that a 7.8-magnitude earthquake had hit Nepal’s capital, Kathmandu. Acharya was visiting his brother in Boston and was up with jet lag, checking email, when he saw news of the quake. His first concern was for family members still in Nepal. For several hours, he and his brother tried desperately to reach their parents, but phone lines were dead or jammed and online access was down. Five hours later, they finally talked to their family and learned they were safe.
Then Acharya sprang into action – but not by hopping on a plane to Nepal. “The first impulse for most health professionals is an emotional one. You feel like you want to go there,” says Acharya. “Nepal didn’t need experts to fly in. Yes, hospitals were damaged – even providing care in tents. But they had trained staff and a supply chain. Instead of experts, they needed resources.” International organizations were mobilizing, but most were focused on Kathmandu, even though the rural areas were the hardest hit.
So Acharya and his brother launched a campaign on the crowdfunding website Indiegogo, setting a goal of $20,000. The response was quick and surprising; in just two weeks, they raised over $1 million. As a co-founder of two Nepali nonprofits, Acharya knew how to get the funds to the rural communities that larger charities might overlook. He also developed a mental health training curriculum and translated WHO protocols for responding to mass fatalities into Nepali and posted them online. The resources are now being used to train clinicians in Nepal. In addition, Acharya and his colleagues are working with WHO to develop management supervisory plans for doctors in the earthquake-affected areas. “If you send a doctor like me in for a few weeks, who takes over my case load when I leave? Focusing on training and capacity-building is significantly more important than a shortsighted, time-limited emergency response.”

These women are digging out an earthquake-damaged home in rural Nepal. Photo: Carli Schultz
Helping From Home
Back on campus, UCSF takes the findings from these projects and examines how to respond more safely and effectively. Robyn Gershon, MHS, DrPH, researches occupational and environmental health and safety in high-risk work situations and focuses on assessment and risk management in crisis situations. For example, she designed and conducted the largest human factors analysis of a high-rise evacuation, evaluating the 9/11 World Trade Center disaster. Not surprisingly, she found that organizations which actively promote workplace safety and preparedness produce a workforce that is able to react more quickly and calmly during evacuations due to disasters. Her conclusions contributed to critical revisions in New York’s high-rise fire-safety laws.
Focusing on training and capacity-building is significantly more important than a shortsighted, time-limited emergency response.”
And as a capstone project for her degree in global health sciences, Liza Dernehl, MS ’15, studied health care workers returning from the Ebola outbreak in Sierra Leone and Liberia. She found that the stigma of Ebola, the frustration of working in a resource-limited environment, and the inability to provide basic life-sustaining care, brought on periods of depression and anxiety for returnees. “Complex humanitarian crises and mass-casualty scenarios bring on stressors for health workers,” says Dernehl. The solution, she notes, is through predeployment preparation, strong psychosocial support, and improved public understanding about the nature of outbreaks. “We can provide psychosocial support and preparation for responders, but unfortunately,” she adds, “we are far from achieving public understanding of epidemics.”
A committee co-chaired by George Rutherford and Associate Chancellor Theresa O’Brien, PhD ’07, which was formed to develop guidelines for the Ebola response, is reviewing the lessons learned and determining the need for a standing committee to facilitate rapid, coordinated responses.
“What should our institutional posture be in relation to health crises? UCSF has a duty to protect the people of California,” explains Rutherford. “You can either solve an outbreak here or solve it there. We chose to solve Ebola there to protect the public and preserve safety. These crises will continue to happen, and hopefully our response will become part of our regular course of business, while we remain true to our mission of reducing the burden of disease and easing health disparities around the world.”