Walk into any grocery store, grab a few packaged products, and flip to the ingredients. You’ll likely spot added sugars – lots of them – provided you can discern their dizzying array of names: sucrose, dextrose, barley malt, agave nectar, high-fructose corn syrup, treacle, to list just a few.
Why is our food saturated with all these sweeteners? When did they make their way into our yogurt, cereal, and oatmeal? How did they sneak into our salad dressing, soup, bread, lunch meat, pasta sauce, and pretzels?
And, most crucially, what forces are responsible for this deluge, which is making some of us very sick?
UCSF scientists are uncovering the answers to those questions. What they’re finding is that the food and beverage industry pushes sugary products, while obfuscating the significant health hazards of added sugars. UCSF researchers are scrutinizing this influence, scouring the research to better understand sugars’ link to disease, and fighting biased science by exposing industry tactics and educating the public.
The more we eat, the sicker we get
When Dean Schillinger, MD, was a resident at San Francisco General Hospital in the early 1990s, almost half his patients had HIV or AIDS. Today, he’s chief of general internal medicine at the hospital, and a new crisis occupies him: Nearly half his patients have type 2 diabetes. Many grapple with its horrific toll, including blindness, kidney failure, amputations, heart attacks, and strokes.
Startling statistics bear out Schillinger’s experience: Since 1970, the incidence of diabetes has more than tripled (type 2 diabetes accounts for about 95 percent of that increase). In California alone, 11 percent of adults have diabetes and 46 percent are prediabetic. That adds up to over half the state’s population. Another troubling fact: People of color and those at lower income levels are at higher risk of having type 2 diabetes and are getting it at younger and younger ages.
Nearly one in four teens has prediabetes, placing them at very high risk of acquiring full-blown diabetes within 10 years, in the prime of their lives. About one in two children of color born today will be diagnosed with type 2 diabetes during their lifetimes.
It’s not the only disease that’s reared its ugly head in recent decades. Nonalcoholic fatty liver disease – a buildup of extra fat in liver cells, which can lead to cirrhosis, or scarring of liver tissue – wasn’t even a known diagnostic entity 30 years ago. Now almost one-third of U.S. adults have it. The disease is on track to become the leading cause of liver transplantation within five years. And doctors are treating the first generation of kids with fatty livers.
We need the general public to become aware of what’s going on with industry influence.
Dean Schillinger, MD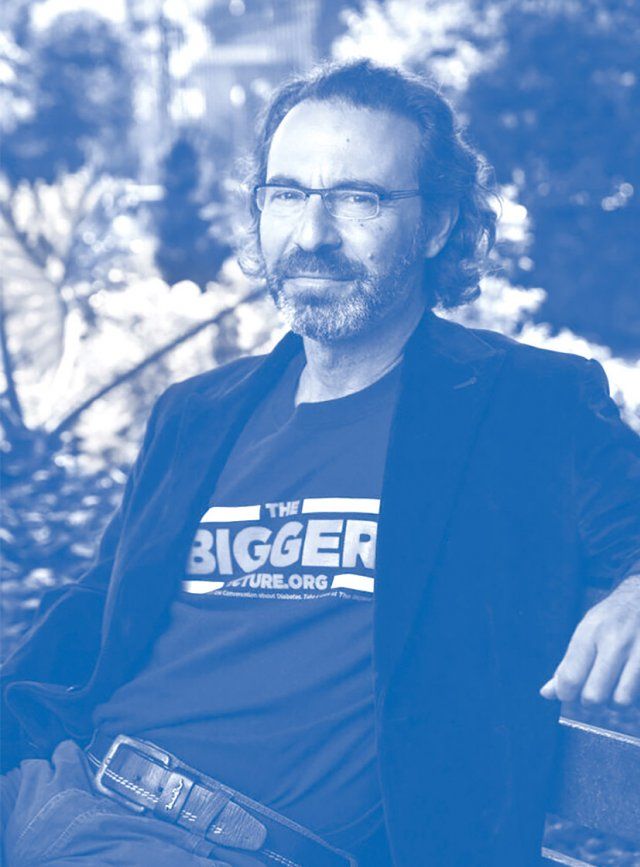
The dramatic spike in these diseases isn’t caused by genetic changes, a common misbelief, says Schillinger. “Something in the environment has changed.”
That “something” includes many societal shifts – such as sedentary lifestyles and larger portion sizes – as well as greatly increased consumption of added sugars, say Schillinger and others.
Americans eat far more packaged foods and consume more sugary beverages than we did 50 years ago. And sweeteners are almost impossible to escape: They’re in three-fourths of packaged products. Liquid sugar, in the form of sodas, energy drinks, and sports drinks, represents 36 percent of the added sugar we consume. On average, Americans eat about 17 teaspoons of added sugars every day — substantially more than the U.S. Dietary Guidelines’ recommended maximum of 12 teaspoons on a 2,000-calorie diet. That adds up to a whopping 57 pounds a year.
“Our food system is completely out of whack,” says Laura Schmidt, PhD, MSW, MPH, a professor of health policy and the lead investigator of UCSF’s SugarScience initiative.
A growing body of scientific evidence now links long-term overconsumption of added sugars to diabetes, cavities, liver disease, and heart disease. Much of this evidence focuses on a cluster of metabolic issues, known collectively as metabolic syndrome (MetS), that raises people’s risk of developing chronic diseases. These issues include insulin resistance, elevated blood sugar, high blood fats (triglycerides), high cholesterol, high blood pressure, and a condition known as “sugar belly.”
Our AIDS ward has become a diabetes ward. It happened in front of my eyes in basically one generation.
One of the main culprits in MetS is fructose. Fructose is found naturally in fruits and honey, but in processed foods and sodas it’s been extracted from corn, beets, or sugarcane, stripped of fiber and nutrients, and concentrated. Nearly all added sugars, even healthy-sounding ones like organic cane sugar, contain significant fructose. Table sugar, for example, is 50 percent fructose. The most common type of high-fructose corn syrup, a concentrated, liquid form of added sugar, is about 55 percent fructose.
The problem with fructose is that the body can turn only so much of it into energy; the liver transforms the rest into fat globules called triglycerides, which in excess can wreak havoc. The liver releases some of these into the bloodstream, causing “sugar belly” (an especially dangerous form of body fat) and raising cholesterol levels (which are linked to heart disease).
Even worse, the triglycerides that stay in the liver affect insulin’s ability to regulate blood sugar, a condition known as insulin resistance. This causes more fructose to be turned into fat and accelerates the amount of fat the liver releases into the blood. It’s a vicious cycle — one too many Americans are trapped in.
With almost half of Californians and millions of others nationwide at risk of developing full-blown diabetes, “we are sitting on a ticking time bomb,” says Schmidt.

Health policy expert Laura Schmidt (right), who collaborates with sugar industry investigator Cristin Kearns (left). Photo by Saroyan Humphrey
Documents reveal scientific shenanigans
In 2007, Cristin Kearns, DDS, MBA, began an unlikely journey that would shed light on some of the forces that helped push us to this brink. Her foray began years before she became an assistant professor at UCSF, at a dental conference on the connection between gum disease and diabetes. One of the keynote speakers gave his seal of approval to Lipton Brisk, a sugar-laden tea. Aghast, Kearns chased him down and asked how he could possibly call sweetened tea healthy. “There is no evidence linking sugar to chronic disease,” he calmly replied.
“I was speechless,” Kearns recalls. “I literally had no words.”
After all, she had seen how sugary drinks damaged her patients’ oral health. Some had cavities in every tooth, and she knew tooth decay was the leading chronic disease afflicting kids.
Another speaker at the conference, this one from the federal government’s National Diabetes Education Program, shared a dietary advice pamphlet that said nothing about sugar intake. “I found that strange,” says Kearns. She had worked in an inner city clinic where many patients had diabetes, and it was clear to her that excess sugar played a role in their disease.
What was going on? Kearns couldn’t let go of that question, so she went home and started researching sugar. Driven by a nagging hunch, she focused on the players behind the disconnect between her experience and what she heard from “experts.” Up popped the website of the Sugar Association, a trade group that dates back to 1943; its members include Domino Sugar, Imperial Sugar, and other sugar producers.
The more Kearns unearthed about the Sugar Association, the more convinced she became that they were influencing science and federal policies. She quit her job to dig into archives all across the country. One day, she hit the mother lode: 1,500 internal Sugar Association documents related to a public relations campaign the industry had launched in 1976. The documents clearly showed the industry’s plan to influence the Food and Drug Administration’s regulatory review of the safety of sugar. “I couldn’t believe I’d found it,” she says.
Kearns came to UCSF as a postdoctoral fellow in 2013 to learn how to analyze industry tactics, drawn by the faculty’s expertise combating the tobacco industry. In the 1990s, UCSF’s analysis of thousands of tobacco industry documents showed that tobacco companies had known about the grave dangers of smoking for decades, but they withheld that information from the public to protect their profits.
The fruits of her labor revealed the sugar industry’s decades-long strategy to downplay sweeteners’ potentially harmful health effects. She found strong evidence that the industry had manipulated science to protect its commercial interests, influence regulations, and shape public opinion. (The industry has disputed this assessment through public statements by the Sugar Association.)
One of her studies, published in JAMA Internal Medicine, showed that the Sugar Research Foundation, which later become the Sugar Association, recognized as early as 1954 that if Americans adopted low-fat diets, then per-capita consumption of sucrose would increase by more than one-third.
By the mid-1960s, however, researchers had begun wondering whether sugar might be related to heart disease. The Sugar Research Foundation paid three Harvard scientists today’s equivalent of $50,000 to review the existing research on sugar, fat, and heart disease. Their analysis, published in the prestigious New England Journal of Medicine (NEJM), minimized the link between sugar and heart health and promoted fat as the culprit instead.
“It was clearly a biased evaluation,” says Kearns, who spent a year analyzing the communications between the industry and the researchers, as well as the studies included in the review. “The literature review helped shape not only public opinion on what causes heart problems but also the scientific community’s view of how to evaluate dietary risk factors for heart disease,” she says.
These tactics contributed to the low-fat craze, which began in the early 1970s and paralleled a rise in obesity, according to Kearns and Schmidt. Many health experts encouraged Americans to reduce their fat intake, which led people to eat foods low in fat but loaded with sugar (think SnackWell’s cookies). The trend is an example of “how industry has deeply penetrated science in order to distort the facts about what’s good for our health,” says Schmidt, a co-author of the JAMA paper.
Another of Kearns’s studies, published in PLOS Biology, showed that the industry also withheld critical scientific evidence. In 1968, the Sugar Research Foundation funded a research project on animals to illuminate the connection between sugar and heart health. Early results uncovered a potential link between sucrose and bladder cancer. Within weeks of obtaining conclusive evidence that sucrose elevates blood triglycerides by interacting with gut bacteria, the foundation ended the study. The results were never published. At the time, the FDA was deciding whether to take a hard stance on high-sugar foods. Kearns says if the results had been made public, sugar might have been more heavily scrutinized.
With thousands of documents still to analyze, and more archives being identified, she believes she has just scratched the surface of the industry’s influence. “It’s vast,” she says. “I could be doing this for years.”
Diabetes expert Schillinger has also been probing biases in sugar science. In a report in the Annals of Internal Medicine, co-authored with Kearns, he reviewed the 60 studies between 2001 and 2016 that looked at whether sugary drinks contribute to obesity or diabetes. Of the 26 studies that found no link, all were funded by the sugar-sweetened-beverage industry or conducted by people with financial ties to the industry. Of the 34 studies that found a link, just one was funded by the beverage industry; the rest were independently funded.
“It was by far the strongest relationship … I’ve observed between conflicts of interest and science,” Schillinger says.
Stop blaming yourself
Since sugar-related chronic diseases are largely preventable with changes in diet and physical activity, there’s a tendency to point fingers at people for making bad choices and being lazy. Soda companies add to the cacophony by claiming their products can be enjoyed as part of a healthy lifestyle.
Such ideas are bunk, say sugar scientists.
“We need to stop blaming individuals for getting sick and start changing our crazy food environment,” says Schmidt. “It puts an incredible burden on individuals. People’s choices are very limited when 74 percent of our food has added sugar.” And that burden falls most heavily on those without the time and money to purchase and prepare healthy foods.
Scientists and policymakers can change the environment by pursuing the same public health prevention strategies used to combat Big Tobacco, Schmidt says.
“It’s easy to forget that back in the ’50s and ’60s, smoking was the norm,” she explains. People smoked on airplanes, at work, in restaurants, even in hospitals. “You could buy cigarettes in our medical center vending machines,” she says. “Public health officials changed the environment. They made it unpopular to smoke.” They did so by amassing evidence of tobacco’s dangers, warning people of its harms, advocating for taxation, pushing to get cigarettes moved behind counters, and calling for smoking to be banned from bars and public buildings, among other approaches. Eventually, the death rate for lung cancer plummeted.
“We’re in the beginning stages of that kind of public health battle around sugar,” Schmidt says. UCSF has already started implementing many strategies, including these:
1. Provide evidence-based information to lawmakers and the public.
UCSF’s SugarScience.ucsf.edu website highlights the evidence about sugar and its impact on health. The site reflects an exhaustive review of more than 8,000 scientific papers published to date. Studies are rigorously reviewed, including for author bias and conflicts of interest.
In addition, the UCSF Industry Documents Library – which houses tobacco industry documents – and the UCSF Philip R. Lee Institute for Health Policy Studies launched the first-ever food industry document archive in November 2018. It includes thousands of previously secret documents by food industry executives, including Kearns’ stash, illuminating how the industry manipulates public health. It’s open to journalists, academics, and the public.
2. Tax products that make us sick.
Schmidt is working on soda tax initiatives with policymakers in the Bay Area and around the world, from India to Africa to Mexico. “Taxes trigger what I call a virtuous cycle of policymaking,” she says. Taxes gently discourage consumers from buying harmful products, while also generating funds that governments can pour into prevention – such as better screening for diabetes, construction of water refilling stations in low-income communities, and promulgation of public health messages.
The beverage industry, however, argues that such taxes make it harder for low-income individuals to buy groceries and unfairly single out soda. But this isn’t the case if the tax proceeds are returned to low-income communities through programs promoting healthy food and clean water access, Schmidt counters. The industry has spent millions of dollars around the country over the past decade to defeat soda tax initiatives. In June 2018, the California legislature passed a bill championed by the soda industry banning California cities and counties from passing new taxes on sugary beverages for 12 years. UCSF’s researchers say this significantly undermines the cities and counties from preventing diet-related chronic diseases through such taxation.
“That was a really bad week,” says Schmidt. “These companies have us totally outgunned. It’s like David versus Goliath.” Such struggles are why it’s essential for scientists to get evidence into the hands of policymakers and the public, she says.
3. Warn people of the harm.
Schmidt, Schillinger, and others at UCSF are trying to issue warnings, but the soda industry is thwarting these efforts, too. The researchers worked with local legislators to help pass, in 2015, the world’s first ordinance requiring billboards advertising sugar-sweetened beverages to include a warning notice. “This was huge,” says Schillinger. “A brilliant landmark for public health.”
But the beverage industry challenged the ordinance, and an appeals court blocked it, saying it unfairly targeted one group of products. In January 2018, the appeals court said it would rehear the case.
Wake Up to the Influence
“We need the general public to become aware of what’s going on,” says Schillinger, who was a paid expert for the City of San Francisco’s defense against the industry’s lawsuit to block the billboard ordinance. That experience, along with his research and boots-on-the-ground care of patients, has convinced him the sugar struggle is a societal problem that needs many more stakeholders. “If this is just a medical issue versus industry, we will lose,” he says.
To that end, Schillinger and UCSF’s Center for Vulnerable Populations co-created a social media campaign encouraging youths of color to voice their outrage in first-person, spoken-word pieces that reframe diabetes as a social and environmental problem, not just a medical one. Called “The Bigger Picture,” the campaign has garnered nearly 2 million views and won numerous public health and film/media awards. Many health departments have adopted it for their own public messaging.
Schmidt points to other encouraging trends – soda taxes have been implemented in 33 countries, for example – but says we still have a long way to go to prevent the looming tsunami of sugar-fueled diseases.
“These industries know sugar sells, they know it tastes good, they know people want it. They’re not going to stop doing what they do,” she says.
But with science on their side, neither will UCSF’s researchers. They’ll continue to seek a sweet ending to the reign of added sugar.