Should You Take a Direct-to-Consumer DNA Test?
What you need to know before sending away your DNA
Illustration: Keith Negley
Since the human genome was completely sequenced in 2003, genetic testing has exploded into a multibillion-dollar industry. And with the rise of so-called “direct-to-consumer” tests such as those sold by 23andMe, which don’t require a physician’s sign-off, investigating your genes is easier than ever.

Kathryn Phillips is the founder and director of the UCSF Center for Translational and Policy Research on Personalized Medicine.
But depending on your reasons, taking one of these tests may not be right for you, says Kathryn Phillips, PhD, a UCSF professor of clinical pharmacy who studies the use and value of new technologies for improving health care. She explains what you need to know before sending away your DNA.
What will you learn from a direct-to-consumer genetic test?
Many of these tests are geared more toward entertainment than clinical use. They report heritable traits like cheek dimples, earlobe type, and eye color, which may be fun but are not clinically important. They can also offer clues about disease risk, but such information is just a starting point. A physician would need to order you a more comprehensive, clinical-grade test if you want medical care based on your genetics.
How does a direct-to-consumer test compare to a clinical test?
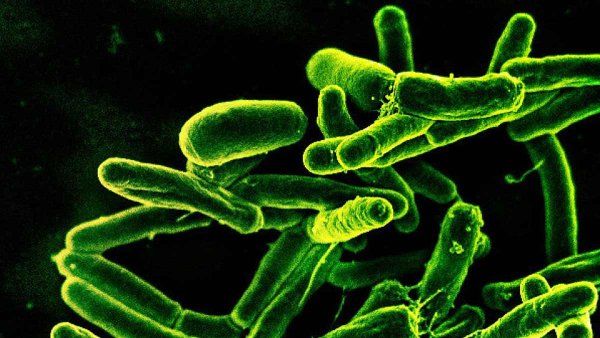
Direct-to-consumer kits typically aren’t testing at the same depth as clinical-grade tests. Take BRCA mutations, for instance. These are variants of the BRCA genes that may predispose a woman to breast or ovarian cancer. Direct-to-consumer kits only test for some of the most common mutations, so they can’t tell you whether you’re in the clear for every possible BRCA mutation. You’d need a clinical test for that.
What should you do if the results are unsettling?
Knowing what to do with a potentially confusing or unsettling finding can be a challenge. Imagine, for example, you tested positive for a gene that increased your risk of a disease for which there currently is no cure, such as Alzheimer’s. A genetic counselor could help you navigate results like that. The good news is that for most health conditions, genetics is just one piece of your risk: Your genes aren’t the only factor determining whether you get sick.
Will your genetic data be kept private?
Unfortunately, nothing is completely private these days. Most direct-to-consumer testing companies are in the business of selling the data they obtain – to pharmaceutical companies, for instance. These data typically are de-identified, meaning any personally identifiable information, such as your name and address, is removed. But your data may be used for purposes other than you intended, such as to help develop new drugs. Some people are okay with that, but others may not be.
Another issue you should be aware of is insurance. By law, health insurance providers cannot deny you coverage based on the findings of a genetic test, but those laws do not apply to other types of insurance. For instance, you could be asked to disclose the results of a genetic test when applying for life insurance, which could affect whether you’re offered a policy and how much you’re charged.
UCSF Magazine
Dive into the future of health in this special issue of UCSF Magazine.


