Recovering From a Head Injury? Your Age, Gender, and Race Might Matter
Kristine Yaffe, MD, shares what scientists are learning about the long-term consequences of traumatic brain injury.
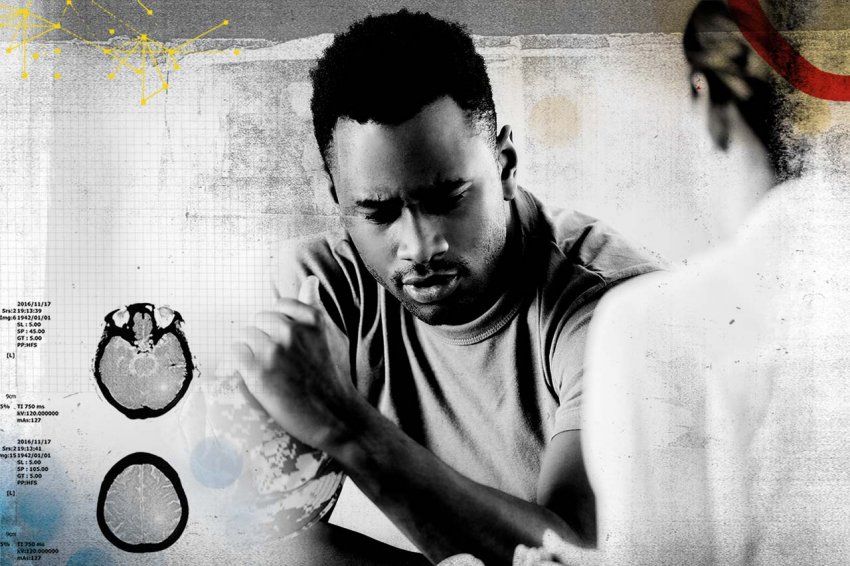
For many Americans, the words “traumatic brain injury” (TBI) conjure images of soldiers returning from combat. That’s a logical association: Technological advances in helmets, armor, and other gear have saved the lives of many soldiers but dramatically increased the number of veterans living with TBI.
Now researchers are struggling to understand what these injuries mean for veterans and other individuals over the long term. With access to more than 2 million veterans’ electronic medical records – the largest dataset of its kind – and dual degrees in neurology and psychiatry, UCSF professor Kristine Yaffe, MD, is in a unique position to find out.
What do we know about the link between TBI and dementia?
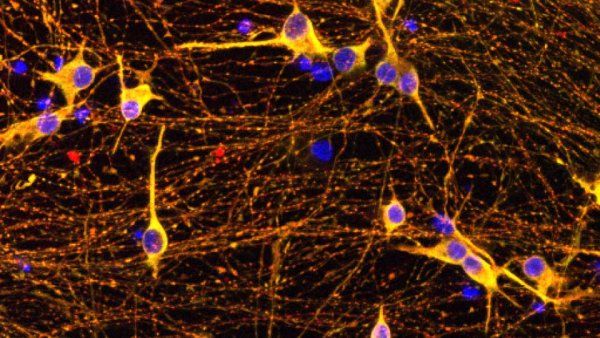
We believe TBI is a very important risk factor for dementia, and yet, when you dig a little deeper, there are so many questions. We don’t know, for example, what kinds of dementia TBI is linked to. Is it Alzheimer’s? Is it chronic traumatic encephalopathy (CTE)? And who is most likely to experience dementia and other adverse effects after TBI?

Kristine Yaffe, MD
Do traumatic brain injuries impact different people in different ways?
We think that they do, though we’re only beginning to understand these differences. We know men are more likely to experience a TBI than women. We know that combining a TBI with another condition – for example, chronic pain or depression – typically results in worse outcomes. There is also evidence that TBI outcomes may be worse among underrepresented minorities, but studies haven’t explored whether risk of dementia is higher after TBI for these groups.
What do we know about how TBI affects older men?
Older veterans with a history of TBI have a lot more behavioral problems — more depression, more anxiety, more post-traumatic stress disorder (PTSD) — and more issues with memory, motor skills, language, decision-making, and time management. We’ve also discovered a relationship between the number of TBIs an older veteran has experienced and the severity of these issues.
Do we know anything about how TBI affects female veterans?
We know almost nothing because women have been really understudied in TBI research. However, my team has the first-ever grant to look at the risk factors for dementia, including TBI, in older female veterans. We have the electronic medical records of every female veteran over the age of 55 – almost 200,000 women. About 1 percent (or 2,000) of these women have a history of traumatic brain injury. We’re only beginning to analyze the data to understand how TBIs impact these women over a lifetime, but it seems that the downstream consequences after a TBI are very similar in women. We’re also seeing that women who have a combination of TBI and either PTSD or depression have double the risk of developing dementia. There seems to be something especially damaging about that combination.
How does traumatic brain injury impact younger veterans?
We’ve found that younger veterans with a history of both TBI and chronic pain are more likely to seek opioid treatment and are more vulnerable to opioid addiction. This finding calls attention to the need for better pain management options for veterans and other patients with TBI. Healthcare providers should be considering non-opioid therapies for pain treatment first in patients with a history of TBI.
Do race or education affect a person’s recovery after a TBI?
We haven’t studied that yet, but we’re planning on it. Fortunately, we have a very diverse group of men and women in our dataset of 2 million veterans to mine for answers.
We do know from other work that underrepresented minorities tend to have a greater risk of dementia for a variety of reasons. My guess is that we might also see a bigger effect from TBI, but we don’t yet know.
There is also the hypothesis that more education and greater cognitive reserve can buffer the effects of TBI and help your brain to better adapt to the damage from a TBI.
What other questions are you hoping to answer?
I want to understand what goes hand-in-hand with the worst outcomes of TBI. Then we can focus on the treatable things — such as depression, high blood pressure, and sleep problems — and provide a buffer against what we call “the TBI effect” on dementia.
It’s also important that we begin to figure out the etiology of the dementia we’re seeing. We know TBI is a risk factor for dementia but of what kind of dementia? And why is it a risk factor? We have quite a bit of work ahead of us.