
When Tom Solis, a renowned chef and baker, fell ill with AIDS in the 1990s, he believed he would soon die. But breakthrough drugs called protease inhibitors quickly put him back on a path to a fairly normal life. Still, he struggled for years with the challenges of managing his disease and the deaths of loved ones in his community. “I felt I always had this tight armor that I could not get out of,” he says.
Then, in 2016, a doctor suggested he look into a clinical trial at UC San Francisco that had just begun recruiting patients for a study of psychedelic therapy in long-term AIDS survivors experiencing demoralization, a kind of existential distress. Solis jumped at the chance. “I’ll be totally honest,” he says. “I wanted to get super-high.”
And that he did. The experience was also one of the most profound of his life. It was momentous for UCSF, too, because the trial marked the beginning of the University’s foray into the fast-growing field of psychedelic medicine.
In 1970, when the U.S. Drug Enforcement Administration (DEA) categorized psychedelics like psilocybin and LSD as Schedule I drugs – the most highly regulated substances – academic studies of them all but ceased. But now, after decades of being pushed to the fringes, research into the healing powers of psychedelics is undergoing a renaissance. In preliminary trials, researchers at UCSF and other institutions around the world are finding that these once-villainized substances show promise in treating a remarkably wide range of mental health disorders, including post-traumatic stress disorder, depression, and addiction.
And for some early trial participants, such as Solis, the drugs’ curative effects have lingered long after the studies concluded.
Down the Rabbit Hole
The impetus for UCSF’s first psychedelic medicine trial wasn’t, as might be suspected, Burning Man – an annual art festival in the Nevada desert known for encouraging radical ideas and hallucinogen use – but a San Francisco mansion with an unobstructed view of the Golden Gate Bridge. It was the home of George Sarlo, a venture capitalist and philanthropist. In 2015, Sarlo hosted a dinner for students and facilitators who had participated in undergraduate psychology training he had funded. Among the guests was a young UCSF psychiatrist and researcher named Joshua Woolley, MD ’07, PhD ’05.

Woolley, a self-described square with an earnest, chatty energy, listened as Sarlo regaled the group with a tale of taking ayahuasca, a drink brewed from a bark that contains a psychedelic known as DMT, which causes intense hallucinations. Anyone who has chatted with a “psychonaut,” as devotees of psychedelics are known, knows that trip stories can be as meandering and convoluted as people’s dreams. But Woolley was captivated.
Sarlo had grown up in Budapest and had survived the Holocaust. His father had disappeared one day into a work camp and never returned. It wasn’t until he took ayahuasca, Sarlo said, that he was finally able to confront his past. He described seeing a vision of dead bodies in the snow, including a skeleton he knew was his father. He asked the skeleton why he had never said goodbye; his father responded that he’d thought he would return and added, “With my last breath, I blessed you and I promised to guard you all your life.”
At the time, Woolley’s lab at UCSF was investigating whether oxytocin – a hormone known as the “love drug” – could facilitate group therapy for methamphetamine addicts. “You’re giving this drug with the idea that you could change social behavior – and maybe trust, openness, and emotional responses – to make the therapy more effective,” he says. Psychedelics, which have similar mind-opening effects, had been on his radar, but he’d never tried them himself and hadn’t imagined he would be the type to study them.
“Hardly anyone had any real expertise in psychedelic trials, so it was kind of the Wild West.”
As he listened to Sarlo enthuse about their virtues, he thought “Why not?” He had a lab at a world-class biomedical institution and was familiar with running clinical trials. The only problem? “Few researchers at UCSF had any expertise in psychedelic trials, so it was kind of the Wild West,” Woolley says. He did, however, know someone who could help.

Brian Anderson, MD, MSc, at the time a UCSF resident in psychiatry, had studied the serotonin system, a neurotransmitter network in the brain that psychedelics act on, and had earned a master’s degree researching Brazilian churches that use ayahuasca for spiritual practices. Like Woolley, he had assumed that pursuing psychedelic medicine trials was not, as he politely puts it, “something that would be beneficial for your academic career.” But he was keen to contribute to the effort and signed on to lead the first trial.
Woolley (now an associate professor) and Anderson (an assistant professor) also recruited Jennifer Mitchell, PhD ’99, a professor of neurology and of psychiatry and behavioral sciences, who was interested in exploring the therapeutic benefits of MDMA, a psychedelic commonly known as “ecstasy” or “molly.” But the team soon encountered another roadblock: Nobody wants to take mind-altering hallucinogens in a sterile hospital room.

What the psychedelic community calls “set and setting” – that is, a person’s mindset when they trip (the “set”) and their environment (the “setting”) – has a profound effect on their experience and on the drug’s long-term effects. Taking psychedelics in a forest, for example, is different from taking them at a music festival, and both of those are different from taking them in a quiet room in the presence of two professional, sober facilitators. “You need a room that you can decorate, have a couch in, play music,” Woolley says. “That’s not easy to do at a university.”
The researchers also needed the DEA’s permission to use Schedule I substances, an arduous process that involved an investigation of the spaces they intended to use for the study. But fortuitously, as Anderson sniffed out, UCSF already had a Schedule I-approved drug safe in its investigational pharmacy. And in UCSF’s Langley Porter Psychiatric Hospital, there was an empty research suite that had previously been used to test the side effects of Schedule I drugs. The team decorated it with art, a patterned rug, a sofa bed, and lamps that cast a soft light.
For the trial, they chose to focus on demoralization among long-term AIDS survivors, a decision that resonated with UCSF’s history as ground zero for treating patients during the AIDS crisis. Facilitators would give participants a standardized dose of psilocybin, the active ingredient in so-called “magic mushrooms.” The dose would be high enough to put them into a dreamlike state, but they likely wouldn’t lose touch with reality. Following their trips, the participants would meet for group therapy sessions to process their experiences.
“A lot of the men had struggled with social isolation,” Anderson says. The goal of the group therapy, he explains, was to help them “connect with each other and find support with each other.” Ultimately, the team hoped, this psychedelics-plus-therapy regimen would allow these men to break free of the stigma, depression, and loneliness they’d carried with them for so long.
By 2017 – with funding from Sarlo and others, including the Usona Institute and the Heffter Research Institute – the study began.
New Perspectives
Indigenous cultures have used naturally occurring psychedelics – such as ayahuasca, psilocybin (which can be found in more than 180 species of mushrooms), and peyote (a cactus that contains mescaline) – for millennia. They take these drugs “not just to treat mental illness,” Anderson says, “but for forms of prayer, to facilitate community gatherings, to solve community and personal issues, and to address all sorts of challenges to human flourishing.” In the 1950s, after chemists had isolated and synthesized several psychedelic compounds in the lab, Western researchers began studying their effects on a plethora of health conditions, including addiction, anxiety, schizophrenia, end-of-life pain, and depression. More than 1,000 studies were published on LSD-enhanced psychotherapy alone.
But in 1970, after the Controlled Substances Act put hallucinogens in the Schedule I category, many of the early pioneers in the field turned away from studying psychedelic therapies for fear of stigmatization or of losing their medical licenses – or simply to avoid the many impractical and burdensome regulatory hurdles. The drought in psychedelics research lasted for more than 30 years until, in 2006, a breakthrough was announced. Researchers at Johns Hopkins University had managed to get permission from the DEA and the U.S. Food and Drug Administration (FDA) to study psilocybin and had published a paper showing that the drug brought on mystical experiences in healthy volunteers. The study provided a road map for other scientists itching to enter the field, and soon, institutions across the country were once again embracing psychedelics as promising therapeutic agents.

Psychedelics seem to help patients break down personal barriers and access new perspectives. (See “How do psychedelics work?”) “Often, the experience can be blissful,” Woolley says. “However, sometimes it can be very challenging and open up people to memories and feelings they did not expect.” Psychedelics tend to amplify emotions, positive or negative. “Patients encounter their psyches, their own fears, and their own strengths as well,” says Gisele Fernandes-Osterhold, MA, a licensed psychotherapist who works with Woolley as the director of facilitation for several psychedelic therapy trials now underway at UCSF.
This was the case for Tom Solis, the AIDS survivor. Before joining the initial UCSF trial, he had experimented with psychedelics, but he’d never taken as high a dose as the study prescribed. In the trial, after swallowing a psilocybin capsule, he slipped on an eye mask and headphones playing instrumental music.
As the drug took effect, he says, “I went deeper and deeper and deeper.” A vision of one of his three brothers came to him. His brother’s face was in profile, like a face on a coin. The image was clear and compelling; Solis had been close with this brother growing up. Another brother appeared more faintly; Solis had a more complicated relationship with this one. And then the third brother, with whom Solis had the weakest connection, appeared dimmest of all.
To Solis, the three apparitions “represented the familial, cultural judgment – that no matter what I did, it wasn’t good enough.” The brothers vanished, and suddenly, Solis was overcome with a new thought: I am worthy; you guys are wrong. You don’t realize what you’re missing.
The defensive armor that he’d always felt vanished, too. “It was just like a sugar coating that melted in the rain,” he says. “It was that quick.” Solis realized he could break the cycle of rejection by being present for his brothers in a way they hadn’t been there for him. He then began to move through some yoga poses. “I was on the bed, dancing,” he recalls. “I felt this great release in movement because I had the freedom to do it now. I was unencumbered. I was pure.”
“I felt this great release in movement because I had the freedom to do it now. I was unencumbered. I was pure.”
Not every participant in the first UCSF trial had such an ecstatic experience. Of the 18 participants, four reported that they felt paranoia during their trip. One, who had never become ill from HIV, suffered severe nausea and hallucinations of vomiting and soiling himself. He later said that the trip was nonetheless meaningful: He believed the hallucinations reflected his intention to better understand the experiences of loved ones who had died of AIDS. (Research so far suggests that both good and bad trips can lead to positive outcomes.)
Overall, participants largely reported decreased feelings of existential distress, better mood, and less anxiety – which lasted weeks to months after their trips. The trial ended in early 2019, and the results were published in October 2020 in the Lancet journal eClinicalMedicine.
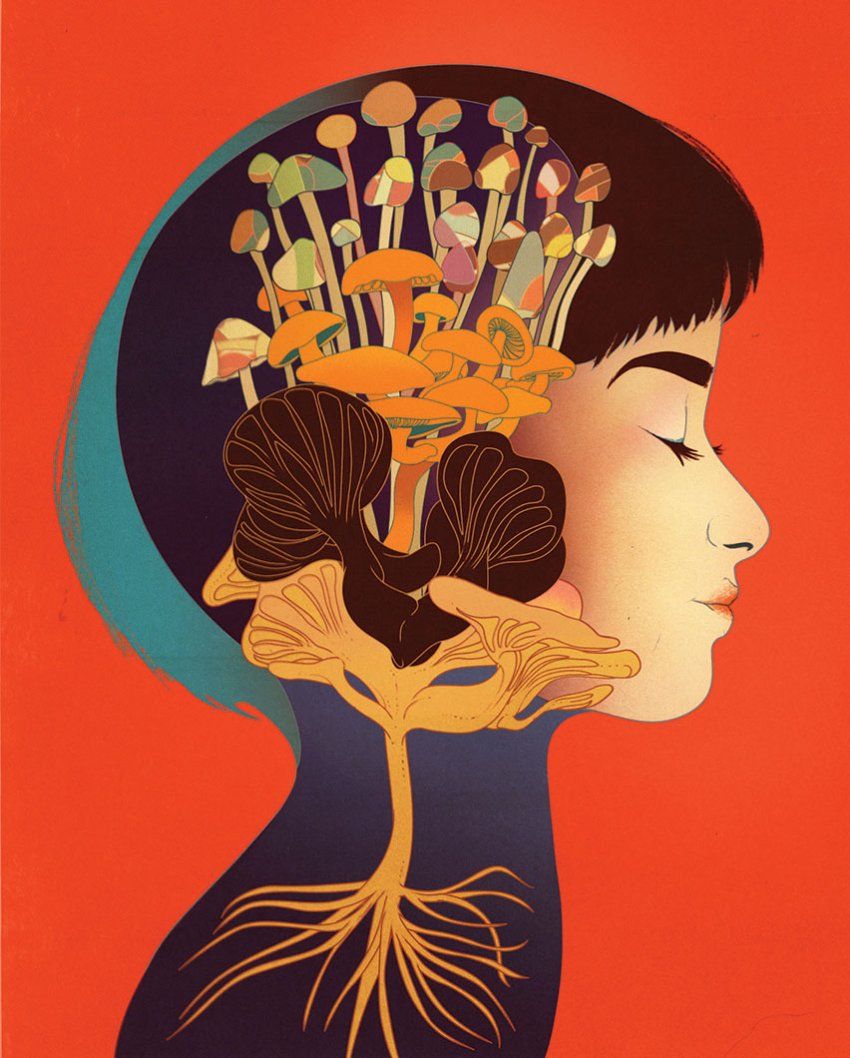
How do psychedelics work?
One of the leading theories posits that psychedelics temporarily change our brains so that we can let go of prior associations and acquire new beliefs. UCSF’s Robin Carhart-Harris developed this theory, called Relaxed Beliefs Under Psychedelics (known as REBUS), while he was at Imperial College London. By taking fMRI scans of people’s brains while they were on psilocybin, he found that subjects’ brain activity during their trips was dysregulated, or impaired, compared to when they were sober.
The reason may have to do with biochemistry. Classic psychedelics bind to 5-HT2A serotonin receptors, cellular proteins that play a role in cognitive flexibility – basically, our willingness to change our minds or think differently. These receptors cluster in an area of the brain called the default mode network (DMN), which is responsible for high-level consciousness, including sense of self and autobiographical memory (think of it as your ego center). A hyperactive DMN may give rise to excessive rumination and negative self-thinking – features of depression, addiction, anxiety, obsessive-compulsive disorder, and many other mental health conditions.
So when DMN activity is dysregulated by psychedelics, Carhart-Harris speculates, those depressive thought patterns weaken, freeing the brain to make new, healthier connections. He believes this neural relaxation may also allow the rational parts of the brain to communicate more fluidly with its instinctual parts, such as its limbic system. Such changes may explain why psychedelics can foster a childlike sense of joy or enable people to revise previously held convictions about life – and even politics and religion.
Trial Fever
Psychedelics research is now booming. Journalist Michael Pollan’s bestselling 2018 book, How to Change Your Mind, brought mainstream attention to psychedelic therapy. And as foundations and pharmaceutical companies took note of the excitement, funding for clinical studies began flowing more readily.
Bolstered by the success of the psilocybin trial in AIDS survivors, UCSF researchers began investigating psychedelics for a variety of disorders. Woolley launched the Translational Psychedelic Research (TrPR, pronounced “tripper”) Program, a consortium of UCSF researchers that is now investigating psilocybin as a treatment for eating disorders, for depression in people with bipolar disorder, and even for chronic low back pain. Because so much of pain is about perception, the researchers hypothesize, psychedelics might help patients learn to manage their pain with less emotional suffering.
In collaboration with the UCSF Movement Disorders Center, TrPR is also testing psilocybin for depression and anxiety in Parkinson’s patients – the first-ever trial in the U.S. to use a psychedelic for a neurodegenerative disorder. Previous studies suggest that psilocybin and LSD create long-term changes in cognitive function and coping strategies. They may also enhance the brain’s ability to acquire new information and make new connections, functions that are often impaired by depression and other neuropsychiatric disorders. For this reason, researchers believe these drugs could be most useful for treating conditions related to existential distress, addiction, or being stuck in certain ways of thinking.

The decision to study Parkinson’s – a degenerative brain disorder marked by uncontrollable movements, loss of coordination, and difficulty with balance – may seem puzzling. But “Parkinson’s is like an iceberg,” says Ellen Bradley, MD, who is leading the trial, which will end early this year. “Motor features are above the water, but there’s this giant part that’s invisible but impactful for functioning.” Depression and anxiety, in particular, plague many people with Parkinson’s, but such patients don’t tend to respond well to antidepressant or antianxiety medications.
Because this trial involves a neurological disorder, Bradley’s team has taken extra safety precautions, including screening for comorbidities, such as dementia, and giving patients a lower initial dose of psilocybin. “You want to target certain symptoms, but it won’t be a useful real-world treatment if it makes other parts of the illness worse,” explains Bradley, who is an assistant professor of psychiatry and TrPR’s associate director.

In 2021, UCSF launched a Psychedelics Division within its Neuroscape translational neuroscience center and recruited Robin Carhart-Harris, PhD, to head it. Carhart-Harris, the Ralph Metzner Distinguished Professor, is known for studying the brain activity of people on psychedelics and has become something of a rock star in the world of psychedelics science. Under his leadership, Neuroscape researchers are planning clinical trials of psilocybin for end-of-life distress and alcoholism. And Jennifer Mitchell, now a member of the group, is leading two phase III trials of MDMA for post-traumatic stress disorder, the final step to earn FDA approval for its use in clinical settings. MDMA, which stimulates the release of oxytocin, as well as the hormones cortisol and vasopressin, seems to help patients confront and let go of traumatic memories.
Carhart-Harris himself is interested in how psychedelics affect the brain and what environmental conditions make them most effective as medicines. He is now conducting brain-imaging studies of healthy volunteers to understand what makes a trip good or bad, a dichotomy inherent to psychedelics. (British psychiatrist Humphry Osmond, MD, coined the term “psychedelic” in a 1956 letter to Aldous Huxley, writing, “To fathom Hell or soar angelic, just take a pinch of psychedelic.”) He also plans to design a new dosing room with high-definition visuals and sounds and curated scents to create more immersive therapeutic settings. “Some people say, ‘I went to a spa in Costa Rica, did three nights of ayahuasca, sat in a warm tub of water, and drank fresh mango juice,’” says Mitchell, who is collaborating with him on the project. “But what about people that wouldn’t be able to jump on a plane?”
The Road Ahead
Some researchers worry that the hype around the medical use of psychedelics will cause people to misuse them. Early studies suggest that the drugs can work as therapies, but only for certain conditions and only when taken under professional supervision. “People think it doesn’t look like the therapist is doing that much on whatever YouTube video they watched,” Mitchell says. “They’re pretty certain that their roommate could do that instead, which may work – until it doesn’t.”
Psychedelics seem to help patients break down personal barriers and access new perspectives.
Psychedelic trips can be especially distressing for those confronting deep-seated mental health issues. “The people who tend to publicly talk about the rainbows they saw are the people who had a positive experience,” Bradley says. “More than one person in our study has said that these sessions were some of the hardest days of their life. And that’s someone lying in a comfortable room with therapists around them and a doctor outside ready to respond to emergencies.”
For this reason, studies like Bradley’s are incredibly labor intensive. UCSF staff members perform medical and psychiatric screenings on all study participants and provide psychological, emotional, and health support during and following trips. A single trip can last for six to eight hours, so the dosing process takes all day.
The work is also expensive. The federal government rarely awards grants for psychedelics research, and many private foundations are wary of supporting drugs that still bear some stigma, so investigators rely primarily on individual philanthropists. This puts pressure on researchers and even participants. Some patients feel guilty if they don’t have positive experiences, Woolley says. “They don’t want to let the science down.”
“Expectations have been set very high,” Carhart-Harris agrees. “There are clear ways in which psychedelics could be superior to current treatments in psychiatry, but we want to be accurate.” And gathering accurate, evidence-based data takes time.
Laws around the use of psychedelics, meanwhile, are changing fast. Oregon, for example, recently legalized psilocybin services for adults. Indigenous populations and other communities around the world have long used psychedelics safely, Anderson points out, but there’s no model for their safe use in mainstream Western culture. Along with Mitchell and others, he is investigating the long-term outcomes of people who use psychedelics in recreational and other nonmedical settings, which he hopes will help inform regulatory policies.
Yet despite the challenges, those who have benefited from experimental psychedelic therapy see its promise for helping others. For many study participants, the experience has had “long-, long-, long-lasting effects,” as Solis puts it. A couple of years ago, for instance, when he heard that his eldest brother had had a stroke, he remembered his psilocybin trip at UCSF. This was the brother who had appeared to him most clearly. For the next year and a half, Solis helped care for him. “When he realized that he was going to pass,” Solis recalls, “he grabbed my hand, looked me straight in the eye, and said, ‘Please help me.’ And I was there.” He credits the psychedelic therapy for allowing him to be so present.
“You see the true nature of things,” he concludes. “You see the true color of things. You see the death of things, but you also see their birth.”





