Talmadge King Jr., MD, dean of the UCSF School of Medicine, tells the story of an ER physician who had lost a document and was searching frantically for it in the garbage bins behind Zuckerberg San Francisco General Hospital and Trauma Center. What he found instead in the mountain of rubbish were crumpled prescription slips that patients had tossed in hospital trash cans throughout the week.
“Going forward, the conversations that ER doctor had with his patients changed. They became, ‘Well, you need these drugs. Which can you afford? How can I help?’” relates King. “Often it’s not that the patients aren’t adhering to advice. It’s that they can’t pay for the drugs, didn’t understand why they should take them, or simply that they did not feel the doctor even listened to them.”
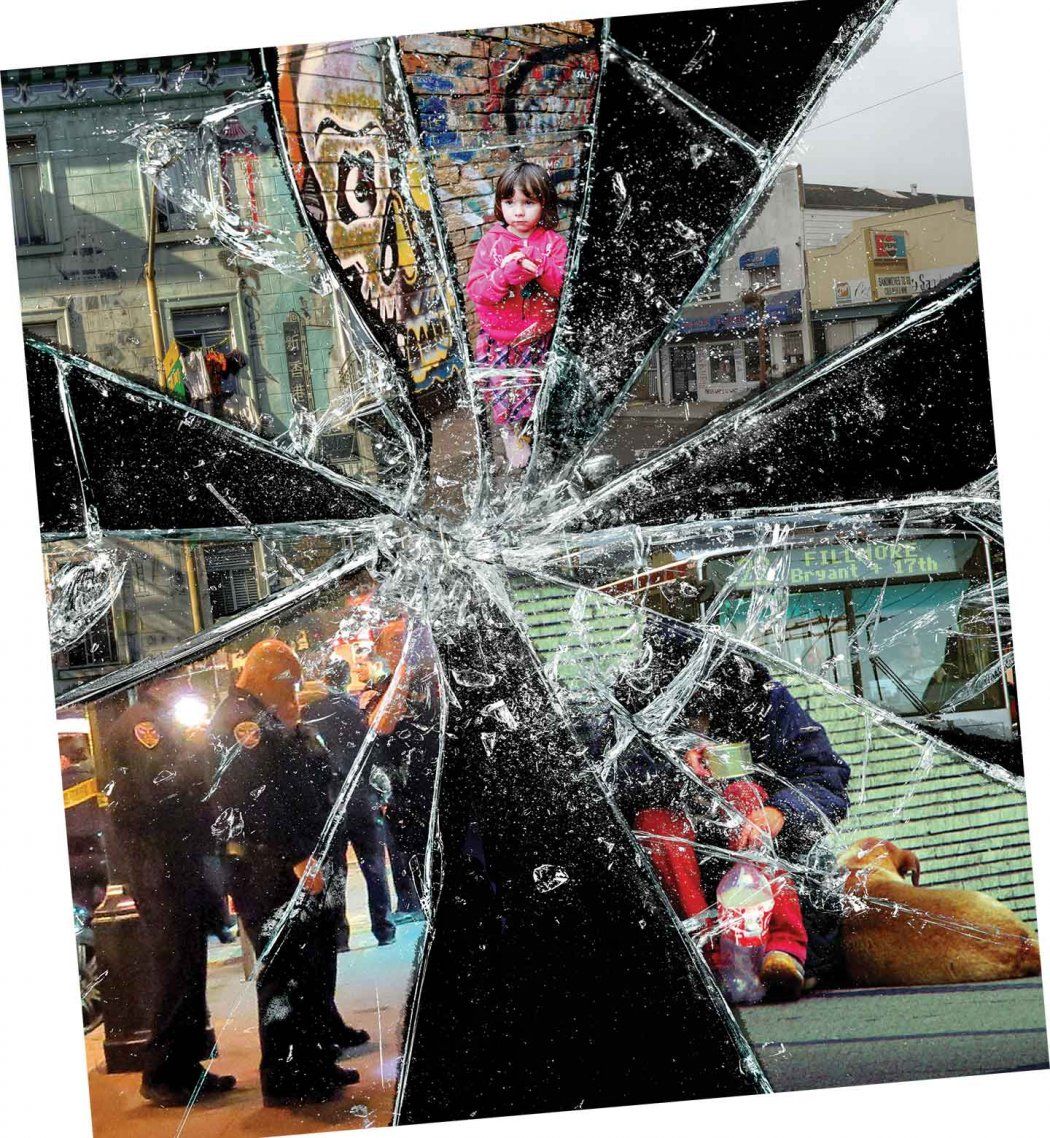
Poverty collides with health every day at UCSF, compelling clinicians and scientists to engineer ways to disentangle the two, one complexity at a time. It’s the nurse trying to help a mom living in a single-room-occupancy hotel find refrigeration for her son’s antibiotic before an infection ruptures his second eardrum. Or the scientist gathering data on the toxic effects of stress on unborn children. Or the dentist trying to salvage the graying teeth in a toddler’s mouth – poverty’s most obvious portal.
Each is a temporary fix, merely scratching at the surface of what epidemiologists have long referred to as the “cause of causes” – poverty itself. This year marks the 50th anniversary of President Lyndon B. Johnson’s War on Poverty – part of his Great Society vision, which brought us such programs as Medicare, Medicaid and Head Start. Yet the income discrepancy between rich and poor has not been as wide as it is now since the late 1920s, an era Mark Twain termed the Gilded Age due to the abject poverty that existed beneath a thin veneer of great wealth. Today, from their front-row seats on the health effects of poverty, scientists and clinicians at UCSF are carefully documenting, and trying to blunt, poverty’s debilitating toll as it cycles through families, from one generation to another.
Mounting Evidence
“Socioeconomic status is the most powerful predictor of disease, disorder, injury and mortality we have,” says Tom Boyce, MD, chief of UCSF’s Division of Developmental Medicine within the Department of Pediatrics. Socioeconomic status is a term that often includes measurements of income, education, and job prestige – individually or in combination. The predictive power of income alone is perhaps most obvious when considering life expectancy. Impoverished adults live seven to eight years less than those who have incomes four or more times the federal poverty level, which is $11,770 for a one-person household, whether you live in Silicon Valley, the Rust Belt or the rural South.
Discrepancies in life span grow significantly when race enters the equation. Paula Braveman, MD ’79, MPH, director of UCSF’s Center on Social Disparities in Health, points to a recent life-expectancy study that used education to reflect socio-economic status and that also considered race. “They found that white people with more than 16 years of education lived 14.2 years longer than black people with less than 12 years of education,” says Braveman, who has published extensively on social disparities for more than two decades. “It’s shocking. It reflects the combined effects of socioeconomic disadvantage and additional racial inequities.”
Socioeconomic status is the most powerful predictor of disease, disorder, injury and mortality we have.”
As dramatic, perhaps, is the association being born into a poor family has with brain development. Programs like Head Start, which intervene with 4- and 5-year-old children to provide increased cognitive stimulation, have shown in randomized trials to significantly improve the IQ of participating children. “Yet when the intervention stops, those gains go away,” says Boyce, the Lisa and John Pritzker Distinguished Professor of Developmental and Behavioral Health. The research is proof positive of the critical need for, and effectiveness of, early and lasting enrichment, which he believes would be ideal by age 3.
In one of his own studies, Boyce and his colleagues put electroencephalogram (EEG) caps on 8- to 12-year-old kids from low-income and affluent families as they played a game. The EEG caps tracked the kids’ brain activity while the game directed them to select a unique stimulus from a group of similar-looking stimuli. The researchers found fundamental differences in brain function. “The kids from poor families had lower IQs and less effective executive functioning, which takes place in the prefrontal part of the brain – things like working memory, semantic fluency and cognitive flexibility, the capacity to readily switch tasks,” reports Boyce. All are essential for academic achievement and advancement.
Boyce points to a recent study in Nature Neuroscience showing that the further you go up the scale in parental education, the more folding – or cortical surface area – is evident in a child’s brain. Cortical surface area sets humans apart from other species; our brains fold inward to squeeze more surface area into our skulls. The kids with the better-educated moms had literally more brain in regions supporting language, reading, executive functions and spatial skills. “These differences are the central nervous system underpinnings of growing up in poverty,” says Boyce. “It is especially important to understand that finding neurobiological differences among children from disadvantaged communities does not imply that the differences are genetic in origin. Rather, many or even most such socioeconomic disparities in brain structure and function are the direct consequences of early rearing in impoverished, chaotic and stressful conditions.”
Chronic disease – which accounts for 70 percent of deaths in this country – is also deeply rooted in poverty. UCSF’s Center for Vulnerable Populations (CVP) is devoted to helping populations at risk for poor health and inadequate health care because of social vulnerabilities. Researchers at CVP report that chronic conditions are striking minority communities earlier and more often. Take diabetes: 10 years ago, one in 11 kids had prediabetes; now it’s one in four. “If you look at minority populations, 50 percent of African American and a third of Latino children will develop diabetes in their lifetime. Those are staggering numbers, and if you look at the poor among them, they are even more so,” says Kirsten Bibbins-Domingo, PhD ’94, MD ’99, director of the CVP. “These diseases usually happen in middle age, but we are already seeing real chronic disease manifestations in people in their 20s, teens, and even younger.”
Poverty’s Path to Bad Health
Research forges a solid, convincing link between low socioeconomic status and bad health. Yet understanding how and why people in poverty are statistically at greater risk for disease is more complex. Diet and exercise play a big role in determining a person’s health status; however, research shows that health behaviors like these are largely driven by the context of where people live. Poor neighborhoods are more likely to have higher crime rates, lower-performing schools, and little access to healthy foods. “It’s difficult to exercise in an unsafe neighborhood, or to eat well in a neighborhood where healthy foods are either not sold or are more expensive than unhealthy options,” says Nancy Adler, PhD, director of UCSF’s Center for Health and Community. Transportation and time also factor into health behaviors. A person who has strung together three jobs to make ends meet for his or her family, and who must travel by bus to each job, likely does not have the luxury of time for exercise.
U.S. Ranks Second to Last in Child Poverty
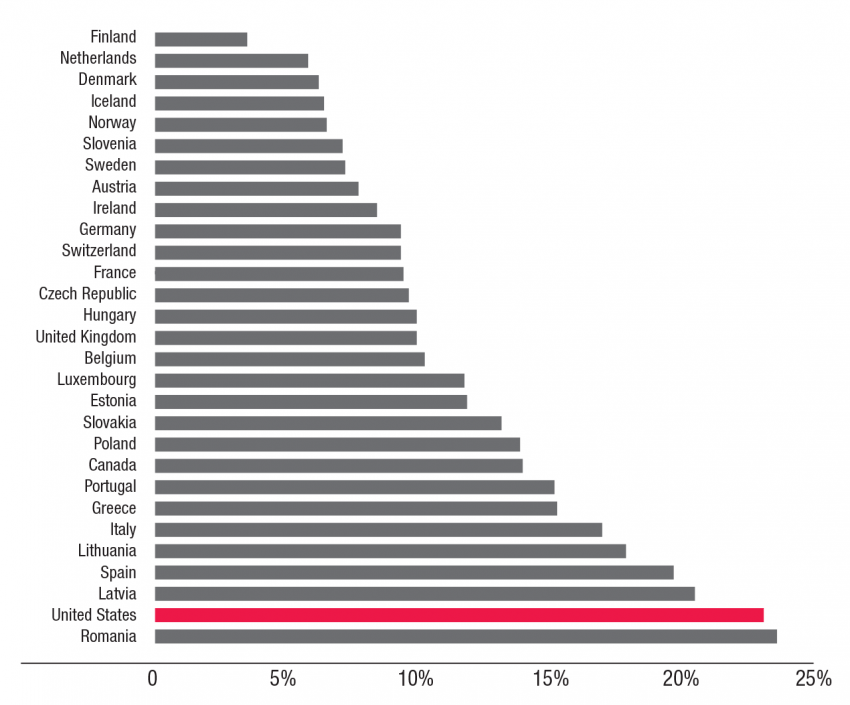
Percent of children aged 0-17 living in households with incomes below 50 percent of median national income out of 29 developed countries. Source: UNICEF
Then imagine layering on top of poverty a sick child. Take, for instance, a family with a child just diagnosed with severe asthma – a chronic condition commonly found in children living in areas exposed to high levels of automobile exhaust. “The mom may not have a job that lets her leave to take care of her child. She has to deal with health insurance, accessing specialists, and getting and affording medications,” says Anda Kuo, MD ’98, a resident alumna, and the founding director of UCSF’s Pediatric Leadership for the Underserved, a residency training program. “All of that is incredibly stressful, and we know that, ultimately, impoverished children with a chronic disease or cancer diagnosis face higher rates of morbidity and mortality than others.”
In fact, the sheer stress and adversity of poverty itself is perhaps its most toxic component, impacting multiple systems in the body. “We know that kids growing up in poverty are more exposed to toxins, noise, turmoil and violence,” says Boyce. “These exposures damage the capacity of the brain to develop optimally.” They provoke the body to produce the hormone cortisol, which sets the body on high alert so that people can maximize their capacity to escape a threat. Put in evolutionary terms, this means that if you encounter a lion, your body releases cortisol so you can get away.
“Cortisol basically shuts down functions you don’t need in a moment of extreme stress, like reproduction or digestion. Your blood pressure goes up, it mobilizes glucose, so you have energy for the escape,” says Adler. That’s fine when you encounter a lion every once in a while. But when you encounter stress every day at home or work, it takes a toll.
People who have a continually heightened response to stress can acquire an allostatic load – wear and tear on the body caused by stress – that permanently throws off their endocrine system and causes it to overproduce cortisol. Their cortisol level goes up and doesn’t come down, putting them at lifelong risk of cardiovascular disease. Others exposed to constant stress have a “hypo-response,” a flattening effect, and they don’t produce cortisol even when it is needed, creating a heightened risk for autoimmune diseases like arthritis, explains Adler.
“Poverty gets under our skin and leads to biological changes that can last into adulthood, even when circumstances change, and, in some cases, affect the next generation through maternal health,” says Bibbins-Domingo. There is emerging evidence that the stresses of poverty could create a lasting effect through what are called epigenetic changes in how our genes are expressed, and that these effects may even happen in utero.
“So, cyclically, poverty leads to poor health and poor health leads to poverty,” says Bibbins-Domingo, who holds the Lee Goldman, MD, Endowed Chair in Medicine. “If that cycle happens across generations, then you are talking about major, seemingly intractable effects on communities living in poverty.”
Dodging the Bullet
How, then, does a clinician prevent or treat disease in poor patients if unstable housing, low-performing schools, and exposure to toxins and violence conspire to undermine their health?
30 Years Later: How Intervention Helps
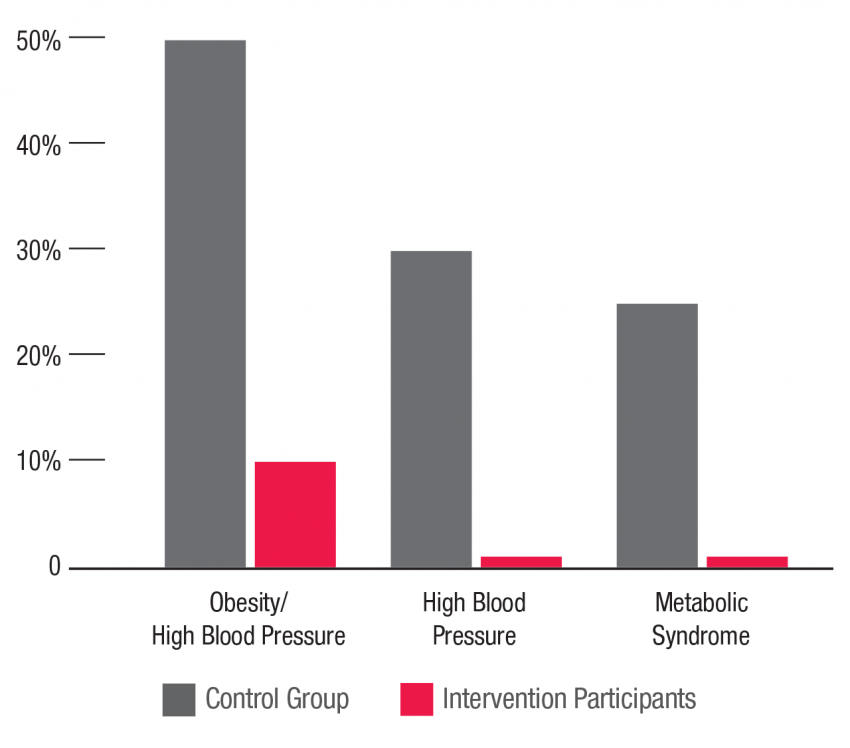
The Abecedarian Project was an early education program in North Carolina for children from infancy through age 5 who were at risk for developmental delays and school failure. The project’s long-term effects have revealed diminished signs of metabolic syndrome, in the form of lower blood pressure, lower blood sugar, decreased waist fat, and more normal cholesterol levels that together decrease the risks of heart disease, stroke, and diabetes. Source: Campbell, Heckman, et al.; Science, 2014
UCSF practitioners and researchers have long been developing programs and studies to circumvent the social determinants of health. “People ask, ‘What can a doctor do about homelessness?’” says King. “A lot, it turns out.” While King was chair of the Department of Medicine, physicians at Zuckerberg San Francisco General took note that certain patients experience frequent hospitalizations. After a bit of investigation, they found that often these patients didn’t have stable housing in which to convalesce. This led the hospital to develop a respite-care program involving short-term housing for homeless persons who are either recovering from a hospitalization or receiving medical care for a condition that renders them too ill to live on the street or in a shelter.
Stuart Gansky, DrPH, director of UCSF’s Center to Address Disparities in Children’s Oral Health, has had great success in changing the standard of care for impoverished children at risk for dental disease. His group showed, in a randomized trial of poor children in San Francisco, that fluoride varnish, which is used routinely in Europe in older children, prevents cavities when applied twice a year to preschoolers’ teeth. It can be applied quickly, easily and to great effect by pediatricians for families with no access to dental care. He points to cultural competence as the key to his study’s success. “In a related study, our medical anthropologists and social scientists held interviews to learn about the experience people had, what works and doesn’t work in the context of their lives,” recalls Gansky, who holds the John C. Greene Endowed Chair in Primary Care Dentistry. “We hired bicultural, bilingual people to whom patient families can relate.” Staff learned that many parents couldn’t bring their children to the clinic during the workweek because of work conflicts or distance. “We held follow-up visits on Saturdays or in evenings,” he reports. “We created playrooms for siblings. We paid for bus vouchers.”
Back to the Drawing Board
Gansky’s study came up with a viable, cheaper alternative than a trip to the dentist, but like all of these programs, it does not address the roots of poverty itself. Though the health care system alone can’t solve poverty, many practitioners and researchers, particularly in the arena of pediatrics, are trying to travel further upstream to intervene before deprivation-related illness sets in and wreaks havoc with families. In doing so, they are rethinking the scope of primary care, particularly in its earliest and most inclusive point of entry – pediatrics.
“First we need to throw out all our assumptions about what pediatricians do,” says Boyce, “particularly now that children can be immunized and have an ear infection treated at a Walmart.” Using community policing as a model, Boyce envisions child resource centers in every neighborhood where parents, who themselves may have been poorly parented, can get expert care and advice in how to break the cycle of adversity. “Could there be child resource centers where social work and primary education is done? Where pediatricians can collaborate with teachers, social workers, and parents?” asks Boyce. “It’s certainly a broader, better model than we have now.”
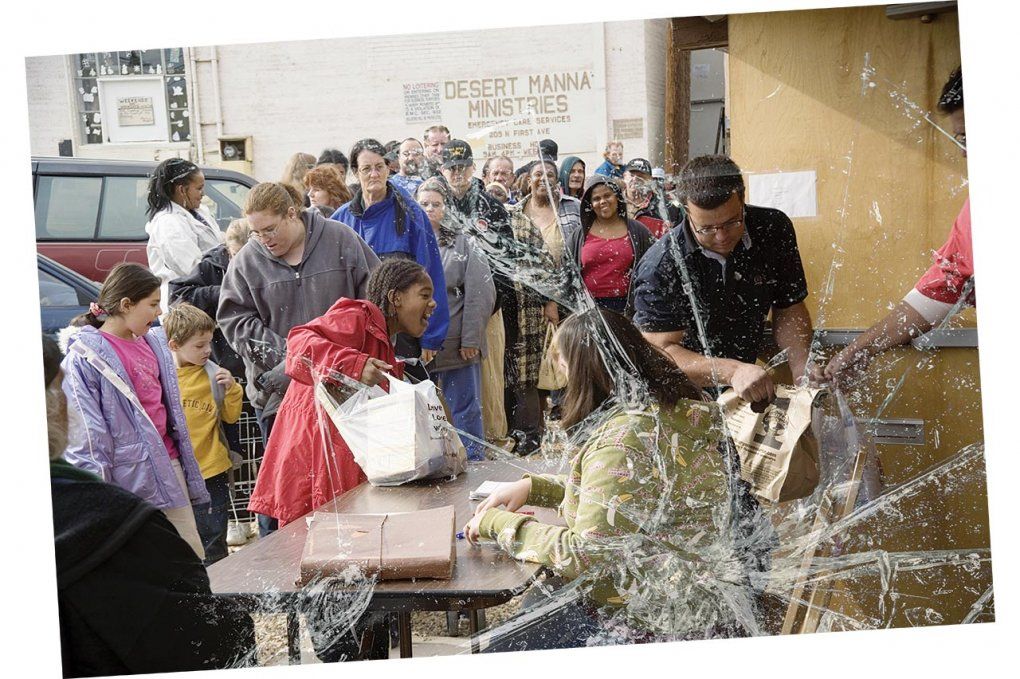
Photo: Spencer Grant
Adler is also considering ways to extend the reach of the pediatrician beyond the clinic doors. She is working with Laura Gottlieb, MD, MPH, and colleagues at UCSF Benioff Children’s Hospitals of San Francisco and Oakland and at SFGH to screen families for problems with housing, nutrition, violence and schooling and to link them with needed services. As part of this effort, they are examining the impact on the child. Half the families are randomly assigned to receive a paper listing of resources that address their identified needs. The other half interact with a trained volunteer or community health worker, who helps link them to the services and follows up by phone. Preliminary findings are encouraging and suggest greater benefit for those who receive the active intervention.
“We insert someone in the system who flags issues for a pediatrician: ‘This is somebody who needs legal help, enrollment in food stamps, housing,’” says Adler. “The pediatricians can’t be responsible for all those things, but they can be a part of a system that connects families with resources.” Though her intervention is pediatric in focus, it is a multigenerational approach that addresses the family’s situation holistically.
We know that, ultimately, impoverished children with a chronic disease or cancer diagnosis face higher rates of morbidity and mortality than others.”
The Center for Vulnerable Populations (CVP) is also engaging the passion and fury of adolescents and young adults to drive change in health behaviors in their own communities. The CVP has partnered with Youth Speaks and Youth Radio, powerful mouthpieces among San Francisco’s teens and young adults, to use video, radio, and the spoken word to relay messages about such perils as tobacco, e-cigarettes and sugary, processed foods. These are messages delivered by youth, for youth, in ways that are more effective and less costly than the $245 billion spent on treating people with diabetes each year. CVP also led the development of San Francisco’s EatSF program, in partnership with the Department of Public Health, to distribute vouchers for fruits and vegetables in the city’s poorest communities. EatSF increases the purchasing power of people in these neighborhoods, allowing them to buy healthier food, which in turn stimulates vendors to stock such items.
Kuo is leading a charge to unite all of UCSF’s efforts to ensure that child wellness and equity are a reality – for all Bay Area children and their families – by developing a Child Health Equity Collective. Boyce, Adler, and Braveman – all three considered leading experts in their field – will be essential parts of the collective. “It will pull people out of silos – whether pediatrician, oncologist, internist, epidemiologist, or neurologist – to talk about how better to reach struggling families,” says Kuo. “I want to see the children of the Bay Area leading lives determined by their own efforts and talents, not the incomes of their parents. That is the essence of the American dream.”
Why Now?
Poverty and its effects on mental and physical health are the subtext of many of the year’s headlines, be they on stories about the Black Lives Matter movement, about rising levels of violent crime or about efforts to establish a living wage. An expansion of Medicaid and an increase in the minimum wage were among the top recommendations of the Ferguson Commission report, compiled by a panel of experts to help heal the Missouri town torn by the fatal shooting of an unarmed black teen. The panel supported its recommendations with a chilling statistic: The average life expectancy in the mostly black Missouri suburb of Kinloch is more than three decades less than in the mostly white suburb of Wildwood.
Being able to quantify the biological wake of poverty across generations is a powerful tool. “When physicians are at the table framing these issues with health,” says Bibbins-Domingo, “that elevates the discussion from politics.” It also helps that physicians have come to the table with stronger evidence. “When people were talking about poverty and health or disease 25 years ago, I think they couldn’t say a lot about the mechanisms apart from obvious ones, like malnutrition and toxic exposures in the home or the neighborhood,” says Braveman. “Now we can talk about countless studies on the biologic mechanisms of the stress of always being on the edge of a cliff and barely holding on.”
But generating change will require more than convincing evidence, according to Adler. She believes we must shift the focus of health care away from how we treat disease to acknowledging why the disease happened in the first place. “The analogy I like to use is this: If you are hit by a truck, you are going to want to be treated at SFGH; it’s San Francisco’s only Level I trauma center,” she says. “But, in the end, your health is going to be more affected by the fact that you were hit by the truck than by how the health care system managed your care. Poverty is that truck.”