An Antidote to Loneliness
Physician and podcast host Emily Silverman discusses the pandemic’s emotional toll on health workers – and the therapeutic value of stories.

Emily Silverman, captured via FaceTime at her San Francisco apartment on May 14 at 2:30 p.m. by photographer Steve Babuljak
When Emily Silverman, MD, came to UCSF six years ago for her medical residency, she began, as she puts it, “the immense project of transforming from a nondoctor into a doctor.” While her newfound powers to heal amazed her, the job was hard. She worked long hours. She got little sleep. She saw suffering, illness, and death.
Then, in 2016, while searching for ways to process her struggle, she had an idea: “Let’s get 100 doctors in a room at night and talk about stuff we don’t normally talk about.” So she did. And The Nocturnists, a medical storytelling live show and podcast, was born.
The show became a hit. It was well into its third season when the coronavirus pandemic struck. Silverman, now a UCSF faculty physician at Zuckerberg San Francisco General Hospital (ZSFG), reflects on her experience caring for COVID-19 patients and creating an outlet for health care workers to share their stories.
What’s it like working at ZSFG now?
It’s pretty different. Before the pandemic, I’d get to work, and there’d be people outside and in the lobby just hanging around. Now the lobby is roped off with caution tape. It’s deserted.
There’s a line to get into the hospital. It leads to a screener, who sits behind a podium with a plexiglass shield. They point a temperature gun at your forehead and ask you questions: “Have you had a fever?” “Have you had a cough?” If you say “No,” they give you a sticker and let you through.
The COVID ward is on the sixth floor. It’s shaped like an oval. You walk around the oval, and you see room after room with precaution signs posted on the doors: “PLEASE REPORT TO NURSE BEFORE ENTERING.” There are paper bags taped to the walls with nurses’ names written on them in Sharpie, where they store their masks. Of course, everyone is washing their hands a lot more often than usual.
How do you feel caring for patients?
I want to help them. I want to lean in. I’m usually very touchy with my patients. I’ll sit next to them on the bed. I’ll put a hand on their back. I’ll put a hand on their leg. I’ll hold their hand.
Now I walk into the room and I stand there. I stare at the person. I look at their oxygen level. I talk to them, but I don’t touch them. I worry I’m not providing the same level of care I normally do. How do you bond with someone through layers and layers of masks and gowns and plastic – when they can’t see your face or mouth and on top of that, maybe they don’t speak your language or they’re hard of hearing?
Do you feel safe?
Really what has created the most anxiety for me isn’t exposure to the virus. It’s that I’m not always sure what is the right thing to do. I’m constantly having to think, “When do I change my gown? Where do I put my stethoscope? Do I wash it now or in five minutes?” Hospital procedures are changing so rapidly. It’s this feeling of building an airplane while it’s flying.
Meanwhile, you and your team at The Nocturnists have been producing a new podcast series and interactive map featuring audio diaries from health care workers across the U.S. – and even a few outside the country. What inspired that project?
When we put out the call for submissions, we told people, “You don’t have to prepare anything, you don’t have to write anything, you don’t have to rehearse. In fact, it’s better if you don’t. All we ask is that you come home after your shift, find a quiet place, turn on your phone, and just talk.”
Then we had 50 people sign up in the first 24 hours. Now almost 250 people are participating.
Wow. And the voices are so diverse. I expected to hear from a lot of physicians and nurses. But a few voices surprised me, like the veterinarian and the medical-equipment driver.
I was shocked to get the truck driver! I have no idea how he found us.
Are there particular voices or stories that have stuck with you?
So many. A hospital chaplain from Indiana sent in a tape in which she talks about the importance of rituals and holding space with families at the time of death, and how COVID has made that kind of spiritual care really challenging.
Oh, that was so sad. She can’t come into the patients’ rooms, and so she’s shouting prayers from their doorways.
She can’t be physically present the way she used to. That’s something that’s been on my mind a lot lately: How do we help our patients and families metabolize their trauma and grief when we don’t have access to our usual rituals, our usual ways of connecting as humans?
Who else stands out?
An endocrinologist who runs a private practice in a rural town. She talks about having to move her entire practice into her home. And her husband is the only pulmonologist in their entire county, so he’s basically been working for 20 days straight at this point. He comes home, showers in their pool, and then shuts himself in his room. She brings him dinner, and they eat over FaceTime. She’s taking care of him, she’s taking care of their three kids, she’s taking care of patients, and she’s running a business.
I heard her clip, and I was like “That woman is a badass.”
You just released Episode 9 of the podcast series, which you’re calling “Stories from a Pandemic.” What themes have emerged so far?
The theme of sacrifice has come up a lot. The media has been splashing around the hero narrative, but a lot of the people we hear from don’t feel like heroes. It’s a very complicated tangle of emotions. There’s this desire to jump in and be a part of history [as Gabe, a critical care physician, expresses in his April 2 diary entry]. You want to walk toward the fire and help out. At the same time, you’re feeling afraid, resentful, guilty.
I’m hearing a lot of guilt, actually. For every doctor who’s laid off and stuck at home and feeling guilty that they’re not working, there’s a doctor in the ICU, wrapped in PPE and intubating people, who feels guilty that his husband or wife is home with the kids.
You did a whole episode about guilt called “Helpless.” How did that come about?
When we put out the call for audio diaries, a lot of people wrote to us and said, “I’d love to keep a diary, but I’m in a place where COVID hasn’t hit yet,” or “I’m not actually seeing COVID patients. Do you still want to hear from me?”
Our response was a resounding “Yes.” The impacts of COVID ripple out and affect so many different aspects of people’s lives. Like the travel nurse who had her contract terminated because people who normally came into the hospital with heart attacks weren’t coming in. Her story has nothing to do with COVID and everything to do with COVID.
How have these audio diaries helped you personally?
For me, they’ve been an antidote to loneliness. Every hour or two, I get an email telling me that so-and-so has uploaded a new clip. I feel like these people are with me – like we’re all sitting together around a virtual campfire.
I hope our participants feel the same. It’s one thing to come home from a shift and turn on your phone and talk. It’s another thing to do that and know there’s someone on the other end of the line. And not just me. An entire community is listening.

More from this Series
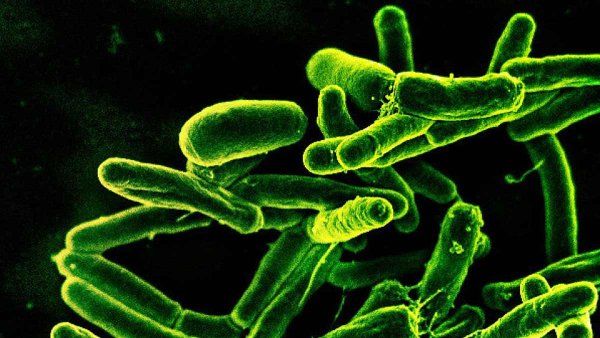
Clinical trial leader Annie Luetkemeyer, MD, tests promising therapies for COVID-19 – and soon a vaccine.