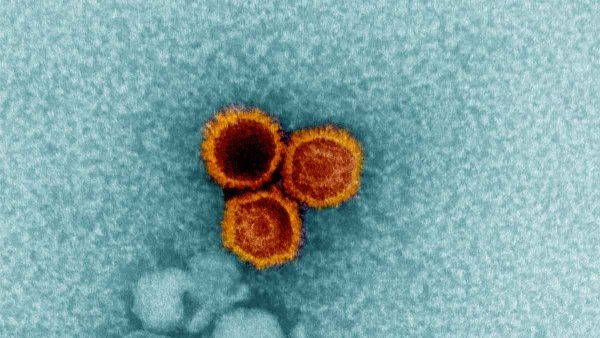
A Goldilocks Dose of Coronavirus
Do masks provide a just-right amount of COVID‑19?
Infectious diseases expert Monica Gandhi, MD, MPH, explores the idea that one of the benefits of masks may be that they provide exposure to enough coronavirus to build immunity but not enough to cause illness. It’s a hypothesis she and epidemiologist George Rutherford, MD, UCSF’s Luca Professor of Preventive Medicine, developed and discussed in a recent essay in the New England Journal of Medicine.

Monica Gandhi, MD, MPH, Professor of Medicine
What do we know about how COVID-19 is transmitted?
We know it’s a respiratory virus, like other severe coronaviruses that have arisen in the past, such as SARS and MERS. And one really interesting aspect of COVID-19 that we discovered relatively early – in late February – is the degree of asymptomatic transmission. With this infection, we know you can be feeling perfectly well but be shedding the virus at a high rate from your upper respiratory tract.
In other words, we know that it is possible for people to pass the virus on to others even when they feel fine. This is in contrast to infections such as influenza, where you have high loads of the virus in your nose and mouth when you feel sick, or with SARS, where you have higher viral loads in your lower respiratory tract, including your lungs and deeper airways, when you’re ill. A virus that can be transmitted when someone is asymptomatic isn’t totally new – it can happen with measles, for example. But it’s something we haven’t seen to this degree for a long time.
How does the amount of virus you are exposed to affect how sick you might get?
We are postulating that the amount of virus you’re exposed to – the viral inoculum – is one factor related to whether you develop symptoms, and if you do, whether you get really sick.
For example, health care workers who intubated people with COVID-19 early on in the epidemic – when the workers were less likely to be masked and thus exposed to a larger dose of the virus – may have become more ill than after health care workers started universally masking. This hypothesis of a higher viral inoculum being related to more severe disease is well-known in animal studies, including one study performed in hamsters with SARS-CoV-2, so we think that the viral inoculum really does matter.
How does wearing a mask affect your degree of exposure to COVID-19?
Wearing a mask filters out some particles, decreasing the amount of virus that you and others are exposed to. We therefore wondered whether wearing a mask and exposing others to a relatively smaller amount of virus might increase the rate of asymptomatic infection and contribute to herd immunity, without making people really sick, while we await a vaccine.
Is exposure to a small quantity of a virus to protect against infection a new idea?
Not at all. In fact, exposure to a small amount of infectious material to activate the immune system was the inspiration for vaccine development. It started with a technique called variolation, which was used to build the immune response to smallpox, another highly infectious disease. It entailed making a small cut in someone’s arm and putting in pus or hair from a vesicle from someone infected with smallpox or cowpox; that would expose the recipient to the infection, often building immunity against smallpox. In the past, variolation was a deliberate process, and importantly, some people actually did get sick from it. We are certainly not proposing we do that purposely now with COVID-19.
But our point in the article is that one effect of wearing a mask may essentially be variolation. Wearing a mask may allow people to be exposed to a quantity of virus that could lead to immunity but not to symptomatic infection. We hypothesize that masks not only affect the transmission and severity of disease but also may contribute to immunity if you’re exposed to just enough virus to get an asymptomatic infection.
What evidence did you use to build the hypothesis that masks may be offering variolation?
Observational evidence has shown that when groups of people wear masks, the rate of asymptomatic infection increases. We saw that with the COVID-19 outbreaks on the cruise ships. We also saw that once masks started to be handed out at food processing plants, 95% of infections were asymptomatic. And social distancing at jails also has been linked to a lot of asymptomatic infections.
If variolation is occurring, how might it affect the pandemic’s outcome
Anything you can do to drive up the rate of asymptomatic infections is a good thing when it comes to building herd immunity because people who have an asymptomatic infection aren’t getting really sick but are developing immunity to the virus. From some recent and very powerful work done at UCSF and elsewhere, we know that even asymptomatic infections can generate a really strong T-cell response, which is a key part of immunity. So wearing a mask may increasing rates of immunity. However, I want to be very clear that this is just a hypothesis; it hasn’t been proven. Also, we have no idea how long such immunity might last.
What benefits might variolation provide while we await a COVID-19 vaccine?
Variolation from masking could provide some benefits similar to what we ultimately hope to see from a vaccine. That’s because the goal of a vaccine is not only to provide a degree of protection against COVID-19 but also to decrease the severity of disease if someone does contract the virus. While we wait for vaccines to get developed and distributed, variolation may already be doing those things to some degree.
If you get an asymptomatic infection and then develop immunity, it is a way to build a bridge to herd immunity while awaiting a vaccine.”
That is key because we know this is a wildly transmissible virus, and because of that, I don’t think we are going to eradicate the infection altogether. When Vietnam reopened, for example, they thought they would be in the clear, but they had another surge of cases after four months.
So although we may not be able to get rid of the virus, we can aim to decrease the severity of the illness it causes. If you get an asymptomatic infection and then develop immunity, it is a way to build a bridge to herd immunity while awaiting a vaccine. For obvious reasons, this is better than achieving herd immunity through people getting sick.
Given the handful of reinfections we’ve seen, are you optimistic that immunity gained through infection – including asymptomatic infection – is durable?
We don’t know how long immunity to COVID-19 will last after natural infection. We have had a handful of reinfections to the virus, but despite so many infected people and so much virus still circulating, we have not seen that many cases. If there was no immunity to the virus, we would be seeing reinfection over and over again. However, we are still in the early phases with a new pandemic; the question of durability of immunity to COVID-19 (from either natural infection or a vaccine) can only be answered over time.
In light of the hypothesis that some immunity may be conferred by masking, can readers let their guards down in regard to preventing the spread of COVID-19?
Absolutely not. It’s very important for people to continue wearing their masks, socially distancing, maintaining good hand hygiene, and remaining vigilant!
Illustration: Lyubov Ivanova