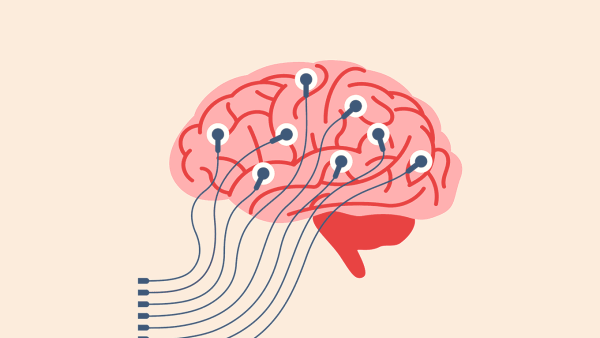
Building the Brains of Precision Medicine
Q&A with Keith Yamamoto

Ten years ago, Keith Yamamoto, PhD, helped lay the foundation for the precision medicine revolution. Even back then, he knew this mode of medicine, sometimes dubbed “the right care for the right patient,” could deploy a new tool – a knowledge network. Yamamoto, now UCSF’s director of precision medicine, explains what this network entails and how it will transform health care.
What is a knowledge network?
It’s the brains of precision medicine. It combines on a single computational platform all research findings about normal and abnormal biological processes. The information is derived from molecules, from experimental organisms, from well and ill people, and from social determinants of health. Machine learning algorithms sort through all this information and find patterns, producing a knowledge network that continuously expands and improves.
Then we link your information to the network – your genome, your blood sugar levels, the stresses you’re under, the quality of the air you breathe, the food you eat – and we ask: What can we say about you? The network seeks to tell you what diseases you’re at risk of; what you can do to prevent them; and, if you do get them, how to treat them in a way that’s most effective for you, not for some statistical group similar to you.
UCSF is building a knowledge network called SPOKE. What kinds of data go into it?
SPOKE merges over 40 huge public databases onto a common platform. It includes information about all human genes, including those that predispose people to disease; proteins those genes encode, including their molecular structures and how they interact with each other; all microbial genes; chemical compounds that interact with proteins; drugs and drug candidates and their effects and side effects; and much more. SPOKE ties all that together and reveals correlations. We’re now seeking to add databases on social determinants of health. Finally, we overlay patient data onto the knowledge network to produce rich individual patient profiles that reveal new insights. The databases are updated weekly, so the network is continuously growing and evolving.
How will SPOKE change patient care?
Profoundly. On the front end, it will enrich our understanding of each patient by connecting individual patient data with SPOKE’s huge, dynamic repository of information, enabling more informed decisions about a patient’s health and health care. Eventually, we should be able to predict someone’s risk of chronic diseases years, even decades, before symptoms appear. My father died of Alzheimer’s when he was 85. In retrospect, I think there were hints of problems 10 years earlier. I’m confident that knowledge networks will be able, early in life, to identify risk and causal factors that predict such diseases, propose optimal treatments for them, and even prevent them through behavioral or environmental interventions.
On the back end, SPOKE will continuously relate discoveries made by basic scientists to human physiology, health, and disease. That will sharpen the hypotheses scientists set out to test and will speed the clinical application of their discoveries. Today, the median time between a basic science discovery and its development into an FDA-approved drug is over three decades! Knowledge networks have the potential to reduce that period manyfold.
And for patients who are already sick? How could SPOKE help them?
There are many ways to answer that question. Here’s one: UCSF data scientists showed recently that type 2 diabetes patients at UCSF are on over 1,600 different treatment plans. Across the five UC medical centers, 6,500 treatment plans were found for this one disease! Clinicians select an approved drug and dosage for each patient and typically adjust them every few months, looking for an optimal response. These choices are based on individual physicians’ expertise, savvy, and experience. But in the future, they could be informed by knowledge network-derived profiles that predict an optimal treatment plan based on a patient’s particular history and biology.
So a knowledge network will reduce trial and error?
Exactly. Here’s an example: Today, clinical trials can take years and cost a billion dollars. But if we better understand a disease’s molecular mechanism, a trial cohort can be focused on patients who have defects in that mechanism and who thus are more likely to respond favorably to a drug specific to that mechanism. This will reduce the number of patients who need to be tested and the duration and cost of trials, and will increase the likelihood of trials’ success. That would reduce trial and error.
Interestingly, SPOKE predicted that the drug dexamethasone would help COVID patients on ventilators, based on what was happening in patients’ lungs at the molecular level. That study was published in May 2020. A couple of months later, a clinical trial confirmed dexamethasone’s efficacy. So a knowledge network could elevate our preparedness for the next pandemic.
What does all this mean for the future of science?
Progress in understanding biological processes and disease mechanisms now comes not just from biologists and clinicians but also from physicists, chemists, engineers, computer scientists, and social scientists. If we integrate their findings into a knowledge network, we will expand the kinds of questions scientists can ask and speed up the pace of discovery. Knowledge networks have the potential to sustain a seamless continuum of science and technology, promoting transformative progress in addressing existential societal challenges – not only in health but also in the environmental, climate, energy, food, and water sectors.
Keith Yamamoto is also UCSF’s vice chancellor for science policy and strategy and a professor of cellular and molecular pharmacology.