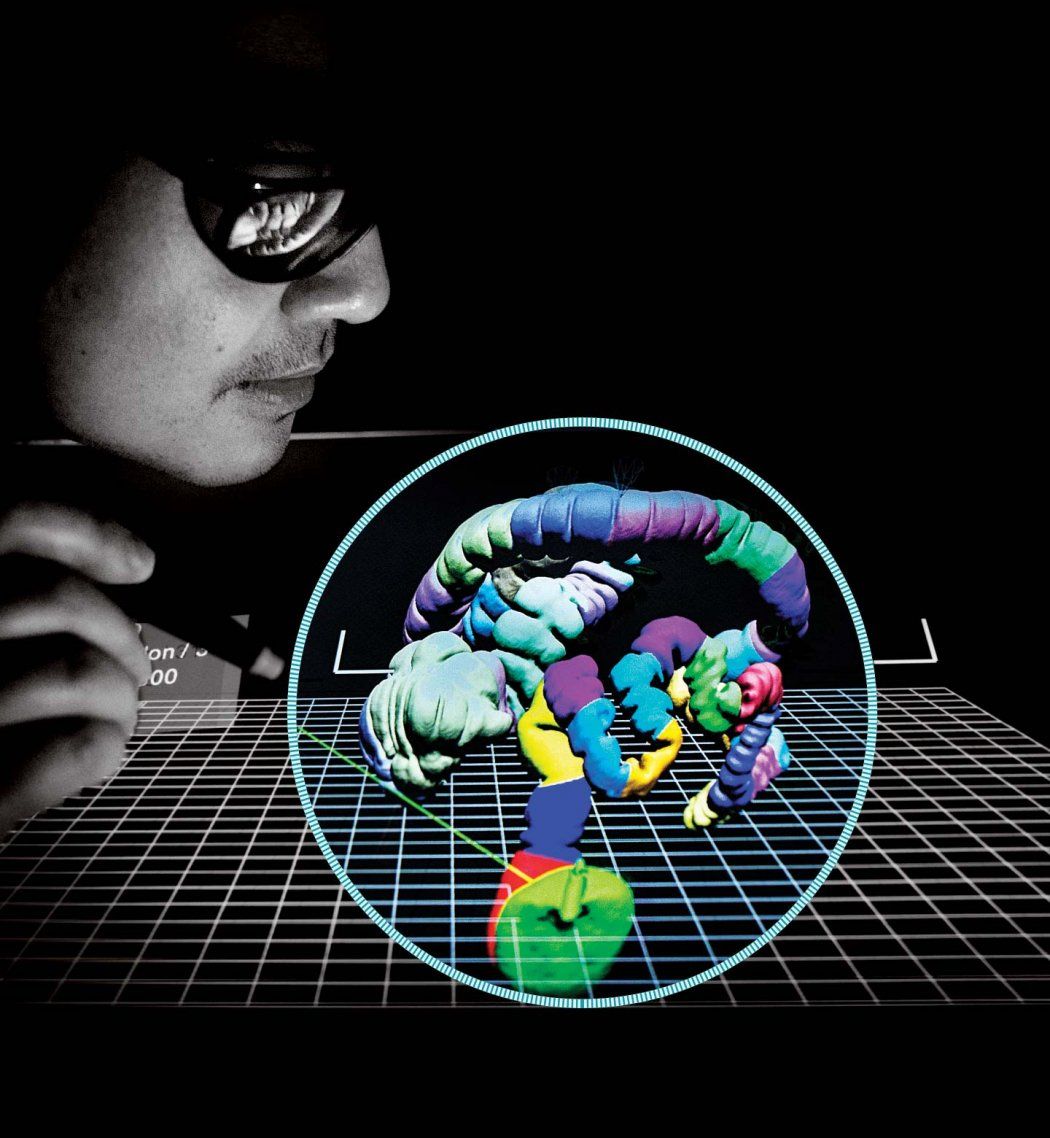
At UCSF’s 3-D Imaging Lab, radiologist Judy Yee, MD, pulls up an image that looks more like a birthday party balloon animal than a patient’s colon: a vibrant, color-segmented tube, torqued and twisted in on itself.
Created from thin slices of a computed tomography (CT) scan, the image appears three-dimensional on the flat screen. It can even morph into video “fly-through” views, enhancing polyps, lesions, and other precancerous anomalies. Yee refined this revolutionary blend of advanced graphical software and scanning technology – known as CT colonography (CTC) or virtual colonoscopy – as a far less invasive and easier-to-interpret alternative to conventional colonoscopies.
Yee, professor and vice chair of the Department of Radiology and Biomedical Imaging at UCSF and chief of radiology at San Francisco Veterans Affairs Health Care System, is now pushing radiology even further with holograms. Virtual holography CTC is the latest phase in her two decades of research committed to earlier, safer, life-saving detection of colorectal cancer. Though the disease is often preventable, it is the second most common cause of cancer deaths in the United States.
“When screening for breast cancer, lung cancer, prostate cancer and other malignancies, we’re typically looking for the cancer itself. By then it’s too late,” Yee says. “Here we have a specific pathology that allows us to find a lesion (known as a polyp) before it turns into cancer. If we could just get more patients to come in for screening, we could certainly have a huge impact on preventing colorectal cancer.”
Holography: Radiology’s Future?
Yee slips on a pair of 3-D black metal-rimmed glasses and points a laser stylus at the monitor still displaying her patient’s colon.
By flicking the stylus and turning her head while keeping her eyes on the monitor, Yee is suddenly “inside” the colon, moving through it, pulling it toward her, spinning it around.
Using 3-D technology, UCSF doctors can isolate and examine parts of the bowel in detail without using invasive cameras.
As she moves, a computer monitor with stereoscopic optical technology tracks her glasses, which have different polarization in each lens, prompting her brain to construct a virtual holographic object that recreates the size and shape of the human anatomy. The stylus, working in tandem with advanced graphical processing of the CTC image, allows her to “grab” the portion of the scan she wants to examine in more detail and interact with it in three-dimensional space.
“I don’t know of anyone else who is doing this,” Yee says, about UCSF’s blending of radiology with virtual holography. “You can cut away the parts of what you don’t want to see and manipulate it so that you improve what you do want to see. It’s a more engaging way to read large data sets. With the added dimension, you can see flat, more dangerous lesions better.”
The technology also has far-reaching promise for neurological, cardiac, and musculoskeletal applications, she adds.
“As the equipment evolves, it allows us to view the same disease processes in a completely different way so we can improve detection and diagnostic ability and streamline workflow,” Yee says. “This could go a long way toward helping show what radiology can bring to patient diagnosis and management for all different parts of the body.”
The ‘Aha’ Moment
A graduate of the Bronx High School of Science, Yee fell for the field of radiology in medical school, where she discovered how imaging blended her rich background in science and mathematics and had a wide variety of applications in medicine.
“We use images to work out the pieces of a puzzle,” she says. “It’s so gratifying to use those pieces to make a patient’s diagnosis and see how the patient responds to treatment. It allows you to participate in a continuum of care.”
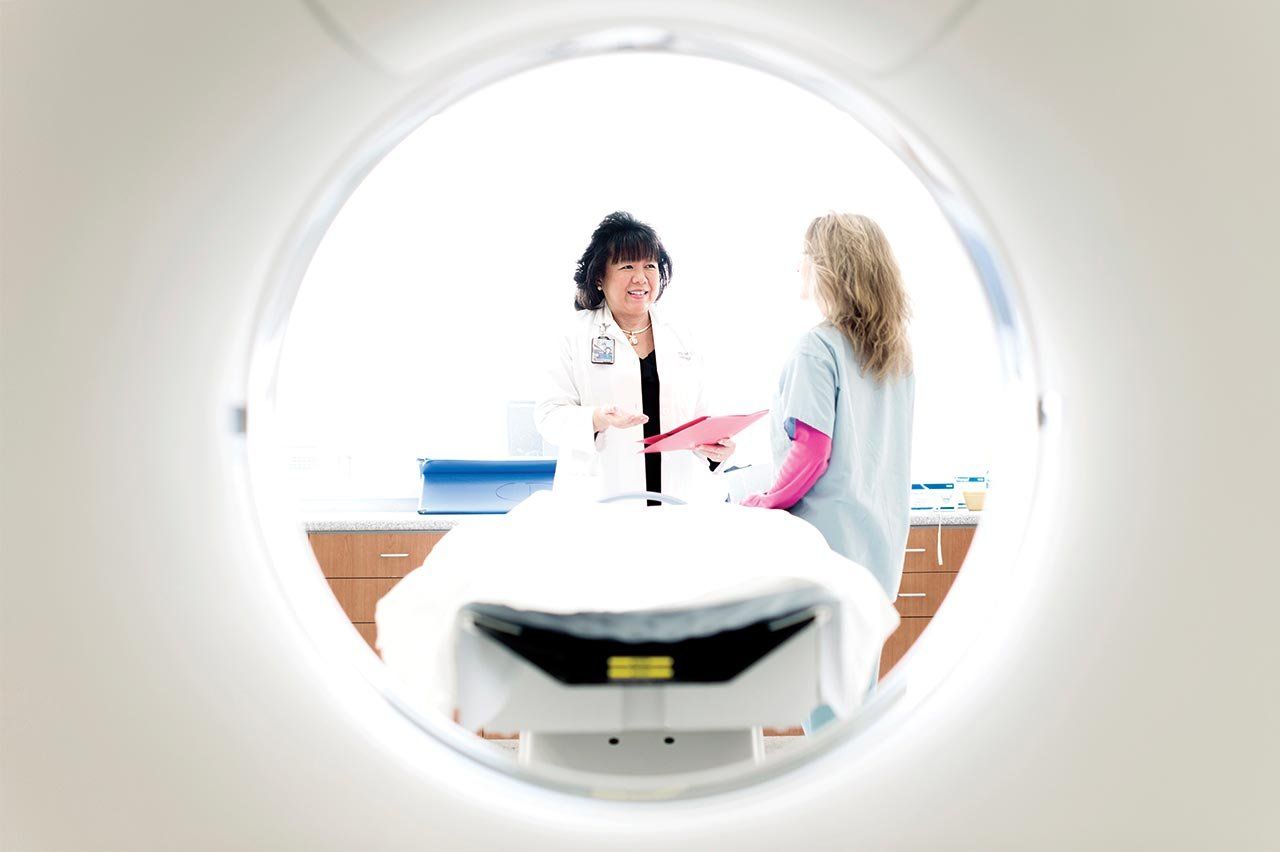
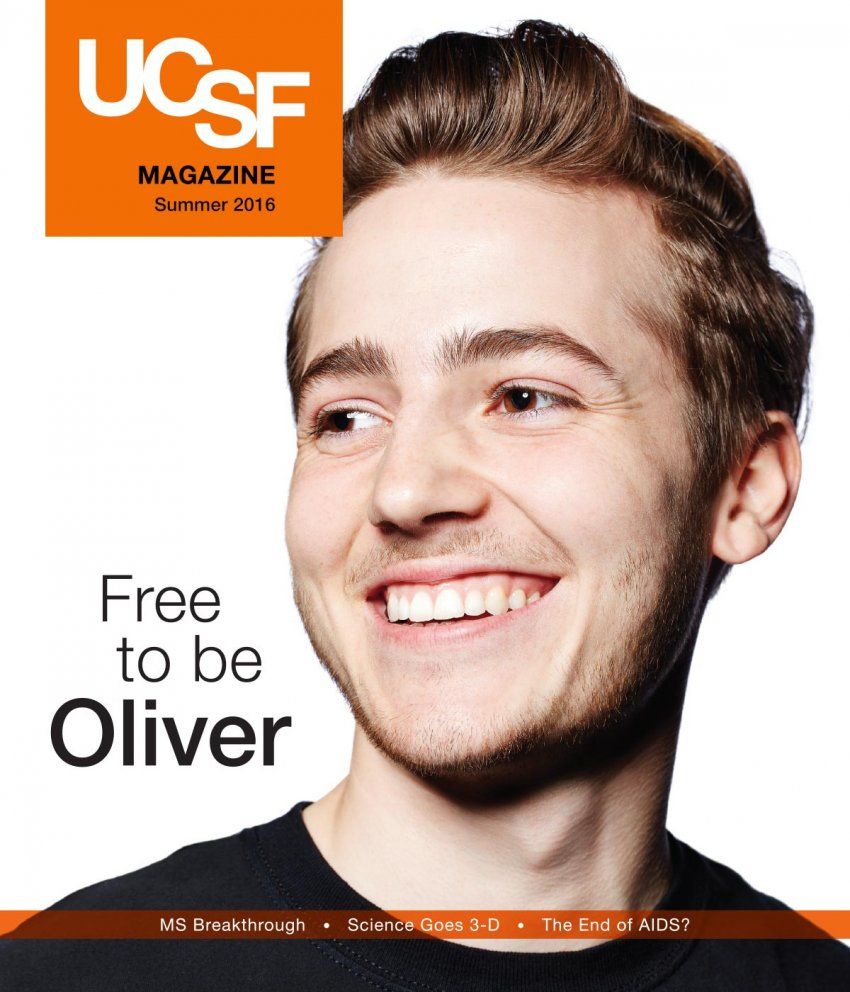
Judy Yee (left) says that if more patients would get screened, it could have a big impact on preventing colorectal cancer. She helped refine the virtual colonoscopy, which doesn’t require sedation, and the low-radiation-dose CT scan takes just 20 seconds. Photo: Noah Berger
Yee got her first look at CTC in 1997, at the annual meeting of the Society of Gastrointestinal Radiology. Inspired, she raced home and wrote a research proposal to further develop the technology, which she realized – even in its earliest stages – held the promise of a better experience for patients and a more effective screening tool for practitioners.
“Conventional testing for colon cancer was not reducing morbidity and mortality, and cancer rates in some areas were increasing,” Yee says. “Many individuals were not coming in to get screened for a malignancy that essentially could be prevented. There’s a fear of the invasive procedure.”
Conventional testing for colon cancer was not reducing morbidity and mortality, and cancer rates in some areas were increasing.”
Her research has fostered numerous improvements, including lowering the radiation dose per scan by two-thirds, while maintaining high-quality detection of polyps and cancers; decreasing the amount of preprocedure laxative required; and increasing the sensitivity of computer-aided detection.
Yee’s current CTC research includes providing data on the protective effect of negative test results. She hopes to persuade the American Cancer Society to endorse CTC screenings every 10 years – the same schedule as conventional colonoscopy – instead of every five years.
She and her colleagues also are working to remove a financial stumbling block to CTC access: Medicare’s refusal to reimburse for the procedure, even though numerous private insurers cover it. Although a CTC test costs significantly less than conventional colonoscopy, many Medicare patients may not be able pay for the procedure out of pocket.
“CTC should be the frontline colorectal cancer screening tool, with only those patients who have a lesion sent on to the more invasive colonoscopy,” Yee says.
Building the Evidence Base
Now president of the Society of Abdominal Radiology and the author of more than 100 articles and 22 book chapters, Yee is an ardent promoter of CTC and its high-tech holographic cousin.
A virtual colonoscopy allows doctors at UCSF to look for signs of disease in the bowels without the need for invasive cameras.
Her first study of the holographic imaging platform is in phase I, with CTC scans from 300 patients loaded and training of participating radiologists underway. Other UCSF explorations of holographic technology include a partnership with the Swedish company Phase Holographic Imaging to accelerate skin cancer research.
UCSF’s 3-D Imaging Lab, which Yee directs and where she developed the virtual holographic CTC process, melds the application of advanced imaging with research and the education of trainees from UCSF and around the world.
More reminiscent of a high-tech company’s conference room than a medical facility, the lab is located at the San Francisco VA and is home to multiple computer workstations loaded with state-of-the-art imaging software, some of which is not yet on the market. The lab’s specialized holographic medical imaging work- station, the True 3D Viewer, was developed by the Mountain View, Calif.-based company EchoPixel, which credits Yee for advancing the field with her insights. Yee now uses holographic technology with about 20 percent of her cases.
The marriage of three-dimensional virtual reality technology with medicine has elicited comparisons to the ever-more-sophisticated world of video gaming. Is that, perhaps, where Yee got some of her ideas? “I’ve never played,” she says with a laugh. “The goal was to have an impact on a common malignancy. For so many patients who develop colorectal cancer, if they had just come in for screening, we could have prevented it.”
A Less Invasive Procedure
Time for your colonoscopy!” Patients receive this dreaded directive to get screened, usually for the first time, around age 50. Even knowing the grim statistics – an estimated 132,700 new cases of colorectal cancer and 49,700 deaths in the United States in 2015, according to the American Cancer Society – doesn’t make colonoscopy any less of an ordeal.
The night before the test, there’s the “preparation,” which many patients find both challenging and unpleasant: No eating, except for Jell-O and clear liquids. Drinking a gallon of polyethylene glycol, a salty-tasting laxative. Spending hours near a toilet.
Then there’s the test itself: A six-foot-long flexible tube with a scope at one end is inserted the length of the colon, and a gastroenterologist “reads” the test as it’s happening.
“The procedure takes 20 to 30 minutes, and there’s a chance of perforation, bleeding or infection,” Yee explains. “You have to receive sedation, or it’s painful. There’s a recovery period, so you have to take a full day off from work, and because of the anesthesia, you can’t drive home by yourself, so someone else has to take time off, too.”
The procedure does have its advantages. It’s covered by Medicare, and if lesions or polyps are detected, they often can be removed during screening because the patient is already sedated. Still, it’s not surprising that the avoidance rate is high: despite a 90-percent survival rate when colorectal cancer is detected early, fewer than half of those who should get screening for colorectal cancer do so.
CTC still requires a prescan laxative, but only 10 ounces instead of 128 ounces. The test involves inserting a small tube a few inches into the colon to inflate it with carbon dioxide. No sedation is necessary, and the total scan time is 20 seconds: 10 seconds lying on your back, 10 seconds on your belly.
“There’s a lower frequency of complications, and you can come in first thing in the morning and then go about your daily activities afterward,” says Yee, who enthusiastically points out that when President Barack Obama underwent his first screening (in 2010, at age 45, because African-Americans have a higher incidence of colon cancer), he chose CTC.
President Obama’s choice allowed him to keep his presidential powers during the screening. His predecessor, former President George W. Bush, transferred presidential authority to Vice President Dick Cheney twice for about two hours while under general anesthesia and in recovery for conventional colonoscopies.