
One morning, as you’re getting out of bed, an intense pain grips your feet. Your toe joints are swollen again. It’s been happening for months now. You decide it’s time to get the problem checked out, so you pay a visit to your doctor, who tells you that you have rheumatoid arthritis.
What happens next depends on who you are. If you’re white, for instance, with good health insurance and access to state-of-the-art care, your doctor probably doesn’t think twice before ordering a biopsy of your joint tissue and then sending the sample off for genetic testing. As luck would have it, according to the results, you’re a perfect match for a powerful new therapy. It’s woefully expensive, but luckily again, your insurance covers it. Within days, your pain and swelling are gone.
But what if you’re poor and uninsured? Even if you manage to cobble together enough money to pay for a genetic test out of pocket, there’s no way you can afford the recommended treatment. Or say you’re a person of color. Because researchers haven’t studied many people like you, no special therapy exists that targets your disease’s particular genetic profile. So your doctor prescribes the standard regimen of steroids and painkillers, which causes weight gain and puts you at risk for stomach ulcers. Plus, your feet still hurt.
This future scenario is, of course, hypothetical. But it reveals both the promise and the potential pitfalls of what’s known as precision medicine.
A revolutionary approach to patient care, precision medicine uses advanced biomedical tools, including genetic and molecular testing and big-data analytics, to help clinicians better predict which treatment and prevention strategies will work best for which patients. It aims to replace the current one-size-fits-all model – in which therapies and interventions are developed for the “average” person – with one that tailors care to each patient’s unique biology and life circumstances, including their race, finances, and living environment.
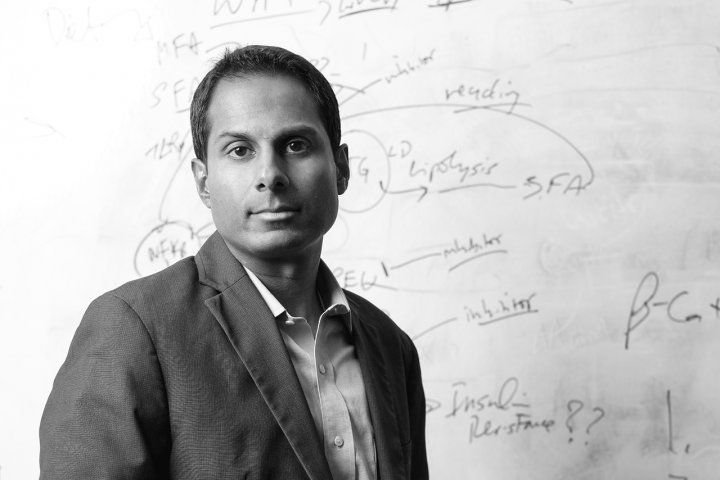
Diabetes expert Suneil Koliwad aims to identify biolgical markers for the disease to help personalize treatment regimens. Photo: Steve Babuljak
Ideally, this customization will bring faster, more effective care to more people. “In the next 30 years, for example, someone with type 2 diabetes will be immediately placed on the medicine that is best suited for their genetic predisposition, their ethnicity, their age, their sex, and the duration of time they’ve had the disease,” says Suneil Koliwad, MD, PhD, the Gerold Grodsky Professor at UC San Francisco’s Diabetes Center. “They’re not going to have to try one therapy, and if that doesn’t work, try another, and another.”
Yet, as Koliwad and other UCSF experts point out, a future in which precision medicine benefits everyone is not guaranteed. For that to happen, they argue, the health care industry must first tackle today’s health disparities, including differences in disease outcomes and access to care based on race, gender, and socioeconomic status. “The worst-case scenario is that certain populations will miss out” – either because some precision therapies won’t work for those populations or because they’ll be unaffordable – “and the gap between the ‘haves’ and ‘have-nots’ will widen,” says Hala Borno, MD, an oncologist and assistant professor of medicine at the UCSF Helen Diller Family Comprehensive Cancer Center.
Koliwad puts it this way: “If we don’t get ahead of health disparities at the same time we’re developing these amazing precision technologies, we won’t have accomplished what we set out to do.”
In 30 years, health care [could] look really good for some people and really bad for others.”
Genomics’ Diversity Problem
The first step will be overcoming the lack of diversity in genetic research. Today, people of color make up nearly 40% of the U.S. population and are expected to become the majority by mid-century. Historically, however, genetic studies – which inform precision therapies and knowledge of disease risk – have almost exclusively enrolled whites.

Esteban Burchard, who studies disease disparities, says the lack of diversity in genetic reseach is “a glaring problem.” Photo: Steve Balbujak
In a world moving toward precision medicine, this racial bias is “a glaring problem,” says Esteban Burchard, MD, PhD, the Hind Distinguished Professor of Pharmaceutical Sciences and co-director of the UCSF Center for Genes, Environment, and Health. That’s because discoveries made about cohorts of mostly white participants may not apply to underrepresented groups, he explains. “There are important biological differences that are being missed.”
For instance, an estimated 86% of Asian Americans have genes that make them hypersensitive to warfarin, a common anticoagulant drug, meaning they could experience uncontrolled bleeding as a side effect of the drug at lower dosages than would most white Americans. Meanwhile, up to 75% of Pacific Islanders respond poorly to the drug clopidogrel, a blood thinner, which leaves them at higher risk of heart attack and stroke. And albuterol, the most-prescribed asthma medicine in the world, is least effective in African Americans and Puerto Ricans, Burchard and his colleagues have determined, even though the prevalence of childhood asthma is highest in these groups.
“The problem is even worse when you start talking about older adults,” says geriatrician John Newman, MD, PhD, a UCSF assistant professor of medicine. “There is very little clinical data on people over 75. They’re just not studied.”
“We have a lot of catch-up to do,” Burchard admits. Diversifying clinical data should be a top priority of health institutions and companies, he says. Otherwise, he warns, “in 30 years, health care will look really good for some people and really bad for others, simply because modern scientific advances have not been applied to all populations equally.”
Racial breakdown of participants in genome-wide association studies
Source: Martin et al., via Biorxiv
That’s beginning to change, thanks to efforts at UCSF and elsewhere. For example, the All of Us program, created in 2015 by the National Institutes of Health, aims to enroll at least 1 million people who reflect the diversity of the U.S. population. That includes people who historically have been left out of health research – not only seniors and racial and ethnic minorities but also rural Americans, people with disabilities, and those who identify as LGBTQ. The program will collect genetic and other medical and lifestyle information on the enrollees to create the largest health database of its kind.
“All of Us is an opportunity to understand how therapeutics, prevention, and screening can be done more effectively in different subpopulations of the U.S.,” says Robert Hiatt, MD, PhD, a professor of epidemiology and biostatistics who leads the program for UCSF, one of six recruitment centers in California. So far, Hiatt and his counterparts across the country have signed up over 350,000 participants, 80% of whom come from underrepresented populations.
The program achieves this degree of diversity through community engagement, Hiatt says. People can sometimes be hesitant to enroll in research studies due to language barriers, financial constraints, or other worries. So All of Us recruiters hand out information and talk with folks at community events and other venues, such as Cinco de Mayo celebrations or the Bay Area Aloha Festival.
Cells to Society
The importance of diversity to precision medicine’s success is hard to overstate. “If you look at obesity, or even cancer,” Hiatt explains, “these are big, hairy, complex societal problems. We need to understand the origins of differences that go beyond inherited biology – to the environmental, cultural, and social factors that shape disease.”
Scarlett Gomez, PhD, MPH, a UCSF professor of epidemiology and biostatistics, refers to such multidisciplinary scholarship as “cells to society.” She studies how social stressors affect outcomes for men with prostate cancer, a disease that disproportionately kills African Americans. “This is one of the biggest, longest-standing health disparities, and we don’t know why,” Gomez says. She suspects that biases in mortgage lending, redlining (refusing to issue loans for houses in certain neighborhoods), exposure to high levels of neighborhood crime, and other examples of what’s known as structural racism may play a role in increasing African Americans’ risk of developing more aggressive forms of the disease.
Greater awareness of such factors, she hopes, will allow clinicians and health policymakers to identify the best ways of reducing risk in these men. This kind of population-based approach to disease management is often called “precision public health” because it applies the principles of precision medicine – finding the right care for the right patient – to groups of people. It also differs from precision medicine in that it focuses more heavily on prevention than treatment.

Anita Sil, an expert in infectious diseases, hopes her research will help identify and care for communities especially susceptible to valley fever, a lung infection. Photo: Barbara Ries
The strategy may be particularly effective for controlling infectious diseases, which can be more virulent in some populations than others. Take valley fever, a lung infection caused by the fungus Coccidioides, which flourishes in the hot, dry soils of the American Southwest, including California’s Central Valley. Cases are on the rise, and symptoms range from benign to life-threatening. “We know that African Americans and Filipinos are much more likely [than white Americans] to have severe complications,” says Anita Sil, MD ’98, PhD ’96, a UCSF professor of microbiology and immunology. “But,” she adds, echoing Gomez, “we don’t know why.”
In the lab, Sil and her colleagues study the fungus’s life cycle, and its interactions with human immune cells, in the hope of solving this mystery. The researchers’ discoveries could help clinicians identify which communities are most susceptible to valley fever and then develop interventions designed specifically for them. This targeted approach, Sil says, “could help us combat a number of pathogens, not just the valley-fever fungus.”
The advantages of precision public health extend to chronic diseases, too. Type 2 diabetes, a common sugar-processing disorder, is just one example. Because studies show a link between diabetes risk and obesity, people who are overweight are often advised to slim down. But that may not be the best advice for everyone, says Koliwad, the diabetes expert. “The fact is, obesity doesn’t impact disease risk in all people equally,” he says. For example, in Southeast Asian, Native American, and some Latinx populations, people tend to develop diabetes at a lower BMI (body mass index) than the average white American, suggesting that weight has less effect on their risk of disease. Consequently, weight loss might not be the most effective risk-reduction strategy for these populations.
Ultimately, Koliwad and his colleagues aim to discover biological markers “at the molecular, cellular, and tissue level that will help us better understand a person’s lifetime risk in a very personalized and precise way,” he says. “Once we learn that information, we can customize nutrition, exercise regimens, and medications for each patient.” But until then, he says, establishing more precise prevention strategies based on broader categories, such as ethnicity, could go a long way toward improving standards of care.
[Patients] are not going to have to try one therapy, and if that doesn’t work, try another, and another.”
The Cost Conundrum
Even if precision medicine solves its diversity problem, however, there’s still a big elephant in the (exam) room: cost.
Oncology is one field where precision medicine has begun to take off. Physicians now can scrutinize a tumor’s DNA for mutations that might predict a good – or bad – response to available drugs. It’s called genomic sequencing, and that alone can cost upward of $5,000. The precision therapies that a patient may subsequently be prescribed, based on the results of genomic sequencing, can carry staggering price tags, too – often more than $10,000 a month. Private insurance plans may not cover these tests or therapies, leaving many Americans unable to afford this cutting-edge cancer care.
Increasingly, the health industry will face hard questions about who will get access to precision-medicine advances, who will pay for them, and which therapies are worth the price. “As with any health-care intervention, we need to assess the cost-benefit tradeoffs,” says Kathryn Phillips, PhD, a professor of clinical pharmacy and the founding director of UCSF’s Center for Translational and Policy Research on Personalized Medicine. “We have to figure out where to use these precision technologies most effectively, efficiently, and equitably.”
Many UCSF experts are optimistic that this can be done, given enough investment in addressing financial and health disparities. By personalizing the prevention and treatment of disease, they agree, precision medicine promises to not only improve but also save a great many lives. The real measure of its success, however, is whether it will fulfill that promise for all.
UCSF Magazine
Dive into the future of health in this special issue of UCSF Magazine.