For as long as she can remember, Joanne Osmond has gone to bed at midnight and awakened around 3:30 a.m.
Not restless. Not groggy. Wide awake, ready for a new day.
Like others in her family, Osmond is a super-sleeper. For seven decades, she’s packed her prolonged days full of activity: as an adviser to small businesses, a member of her local school board, a state-level education leader, a Boy Scout volunteer, a church volunteer, a marathoner, a mountain climber, and a mother.
“I’m not brilliant, I’m not a genius,” she says. “But I’ve had more hours in the day, so I could work harder than most people.”
History is full of productive and powerful people, from Mozart to Thomas Edison, who claimed to sleep just four hours per night. But anyone trying to sleep-hack their way to greatness should be warned: The rare ability to succeed on so little sleep is a genetic trait, not a feat of will or skill. Sleep scientists at UC San Francisco are working to decode the relevant genes and find answers. By improving sleep, they hope to not only help you sleep better but also resolve a hidden public health crisis.
That may sound dramatic, but sleep deprivation can literally take years off your life. It is directly linked to obesity, insulin resistance, diabetes, increased cancer risk, cardiovascular disease, premature birth, and neurodegenerative diseases like Alzheimer’s. In addition, insomnia often triggers depression, and depression can lead to insomnia – a true cycle of misery.
Sleep is essential for our survival. It allows us to be happier, healthier, and smarter. So it’s time to give our sleep the respect and attention it deserves.”
Lack of sleep is also a killer for your immune system: In a gross but convincing study that involved giving a live cold virus to volunteers and then measuring the mucus and congestion among those who became infected, UCSF sleep expert Aric Prather, PhD, showed conclusively that the less people sleep, the more likely they are to get sick. (He has also shown that lack of sleep prior to receiving a vaccination can reduce its protective effect; he is currently studying this link among COVID vaccine recipients.)
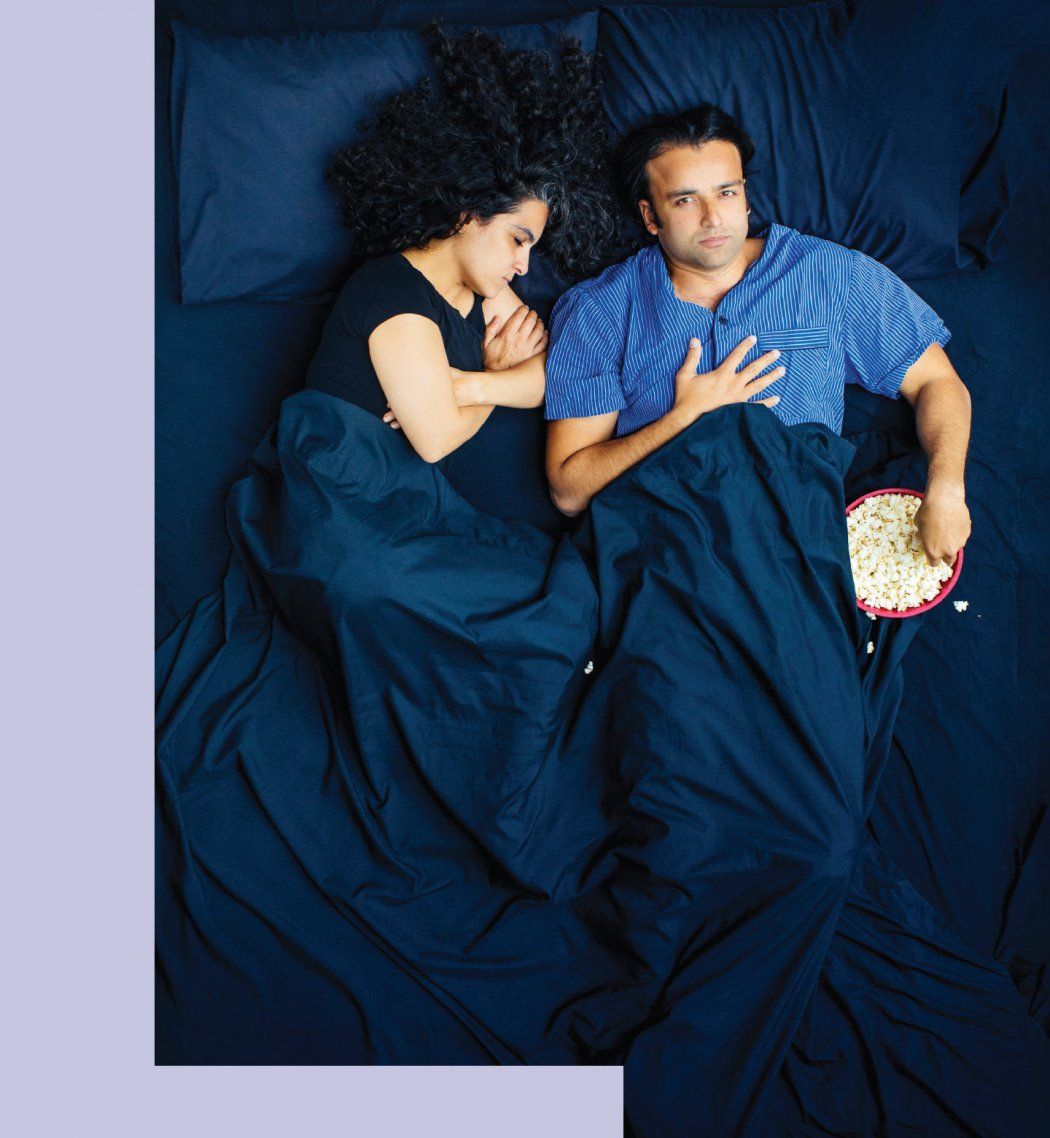
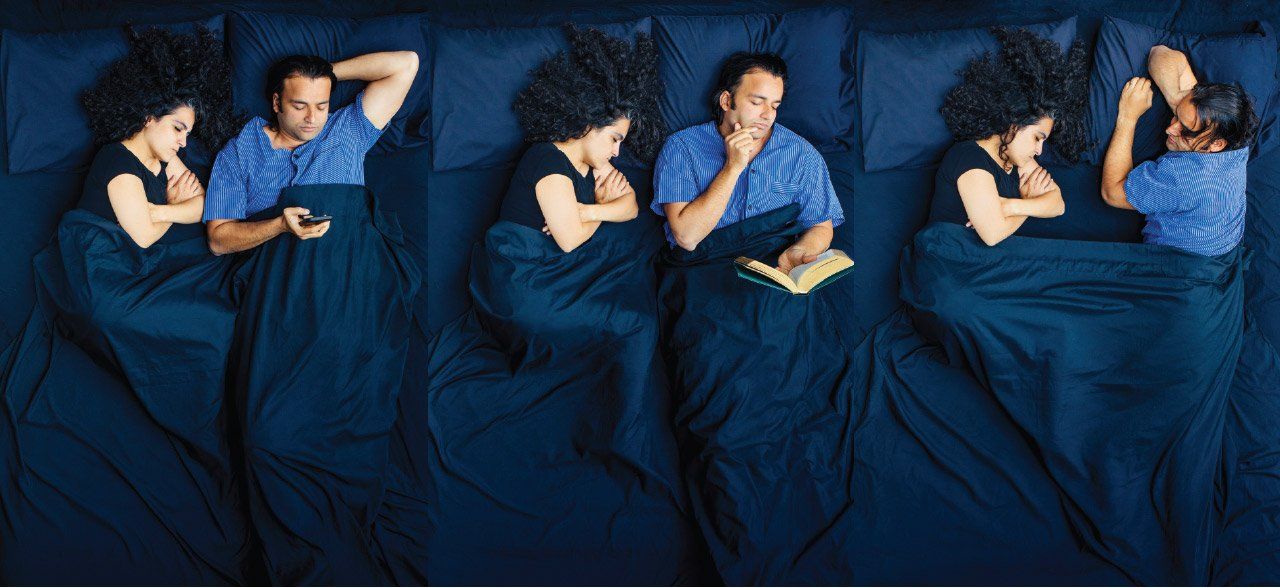
Sleep deprivation hurts us in other ways, too. Driving while drowsy is nearly as deadly as driving drunk. Without sleep, our minds are muddled and we are worse employees, worse students, worse friends, worse partners. How many marriages have crumbled, at least in part, due to how awful we are to the people we love when we are constantly exhausted?

Sleep scientists Louis Ptáček, MD, and Ying-Hui Fu, PhD, have discovered several genes that lead to short, hyper-efficient sleep. Their findings are helping decode how sleep is regulated. Photo: Steve Babuljak
Considering the stakes, pioneering UCSF sleep research collaborators Ying-Hui Fu, PhD, and Louis Ptáček, MD, see sleep as the ultimate target for human wellness. “If we understand how our sleep is regulated – what makes us or keeps us from sleeping soundly – we can have better therapies for sleep disorders like insomnia,” says Ptáček, the University’s Coleman Professor of Neurodegenerative Diseases.
Fu puts it simply: “Sleep is essential for our survival. It allows us to be happier, healthier, and smarter. So it’s time to give our sleep the respect and attention it deserves.”
The mystery of sleep
There’s no question that the brain is doing astounding and essential work while we’re unconscious each night. It is processing memories, emotions, and new knowledge; recharging the immune system; flushing away toxins; and restoring our mental and physical energy. But no one is quite clear how it all works.
Many people imagine that in a sleep clinic, doctors can attach electrodes to the brains of sleeping subjects and peer into the inner workings of their insomnia. But the truth, explains Prather, an associate professor of psychiatry, is that when sleep is measured using polysomnography (a study with those electrodes), “they only provide a proxy for what’s going on in the brain. We’re trying to infer what’s happening throughout the brain, but we’re likely only scratching the surface.”
How does sleep create physical restoration? What role does it have in energy? What is the difference in brain activity for someone who reports getting a “good” sleep as opposed to a “poor” one?
Sleep researchers and clinicians from across the UCSF Weill Institute for Neurosciences are pushing for answers. “Our team is drilling down on this question of how much sleep people need in ways that are pushing the envelope forward and are ahead of most other places,” says Andrew Krystal, MD, vice chair of research in the Department of Psychiatry and Behavioral Sciences, the Dolby Professor of Psychiatry, and a leader of a cross-departmental initiative on the neuroscience of sleep.

Photo: Elena Zhukova
Here’s some of what we do know:
The process of falling and staying asleep is guided by two separate biological mechanisms: sleep pressure and circadian rhythms. These work in concert, vary significantly from person to person, and are exceptionally easy to throw out of whack.
Sleep pressure is the inevitable accumulation of sleepiness each day, caused by a gradual buildup of the molecule adenosine in your brain. (Adenosine is a byproduct of expending energy; it’s freed up from the energy-carrying molecule ATP, or adenosine triphosphate, which fuels all living cells.) The most commonly used drug in the world, caffeine, can fend off sleep pressure by temporarily blocking the brain’s adenosine receptors. But caffeine doesn’t stop adenosine from accumulating, which is why once caffeine clears your system, built-up sleep pressure can hit you like a tsunami.
Your circadian rhythms are much more nuanced. A 24-hour biological clock keeps time for your every cellular function, allowing your body to reliably anticipate and respond to its physiological needs – including sleep. The inner workings of this elegant clock are proteins that build up each night and degrade each day, and the whole system is reliant on environmental cues, most notably natural light.
So what’s keeping you awake?
With all this complexity, it’s not a surprise that there’s no one-size-fits-all answer to the question.
You literally can’t breathe.
The first possible cause to consider is sleep apnea: You are choking on your own collapsing airway, awakening over and over again, just enough to gasp for air, sometimes as often as once every minute. Although sleep apnea affects 22 million Americans, most people don’t recognize it in themselves and only seek treatment at the ultimatum of their miserable bed partner, whose endurance of nightly snoring, gasping, and choking sounds ensures their own variety of sleep deprivation. (No bed partner? Other warning signs include excessive daytime sleepiness and morning headaches.)
The good news: Once sleep apnea is diagnosed, treatments for it – lifestyle changes, oral appliances, and airway pressure devices – are very effective.
You are anxious or distressed.
Almost everyone has at least occasionally experienced the maddening exhaustion of wanting, needing, begging to fall asleep, but being stuck wide awake instead, mind racing. This is insomnia – which can show up as an inability to fall asleep or to stay asleep, or both – and it is often triggered by anxiety or psychological distress.
What’s going on? Basically, your nervous system is stuck in fight-or-flight mode, and the hormones cortisol, adrenaline, and noradrenaline keep your brain alert and ruminating. About 25% of Americans will suffer a short-term bout of insomnia in any given year, but it usually resolves on its own. For about a quarter of this group, however, the problem becomes chronic, lasting three months or longer. At that point, it’s definitely time to see a sleep specialist. (The best treatment for insomnia usually isn’t a pill.)
Your body’s clock is out of sync.
There are countless ways to confuse your circadian rhythms. Hop a flight halfway around the world and you’ll wake up before sunrise and be a staggering zombie by midafternoon. Stay up night after night, doom-scrolling or playing email catch-up, and you’ll find your regular bedtime is hard to get back to. Switch between day and night shifts, and you may find yourself snapping at loved ones, blanking out while driving, or rereading a sentence several times over, unable to focus.
Many of the sleep disorder patients Krystal sees have an out-of-sync rhythm called delayed sleep phase syndrome; they tend to stay up late and sleep late. There’s nothing inherently wrong with a late bedtime, but since the world doesn’t stop for late sleepers, this pattern generally leads to the terrible outcomes associated with too little sleep. “The goal in these cases is to fix the circadian rhythm problem,” Krystal says, “because you can’t drag a person to go to sleep at a time that their biology is not aligned with.”
Photos: Elena Zhukova
We live in an always-on culture.
Even those of us who don’t suffer from sleep apnea, insomnia, or sleep-phase disorders often don’t get the sleep we need. As UC Berkeley neuroscientist Matthew Walker, PhD, puts it in his New York Times bestseller, Why We Sleep, “Humans are not sleeping the way nature intended. The number of sleep bouts, the duration of sleep, and when sleep occurs [have] all been comprehensively distorted by modernity.”
Louis Ptáček puts it in these stark terms: “Right now, awareness of the impact of sleep deprivation is where we were with smoking 40 years ago. Back then, the tobacco industry fought to obscure the risks of cigarettes. Today, our entire society is fighting against sleep health, through this 24/7 culture we live in.”
Your genes play a role.
Super-sleepers like Joanne Osmond inherited a preternatural ability to thrive on only a few hours of sleep. But this genetic trait is very, very rare, so if you regularly sleep less than 7½ hours a night and suspect you might fall into this category, think again; chances are much higher that you are not only sleep deprived but also so used to living this way you can’t even see the problem. It’s true, however, that there’s much more variation in individuals’ sleep needs than we generally recognize. “A lot of people say everyone must sleep 7½ to 8½ hours or you’re not going to be healthy. That’s not true,” says Ptáček. “There are some people who require less, and some who require more.”
What’s more, genetics can account for extreme night owls (who might naturally sleep, for example, from 2 to 10 a.m.) and extreme morning larks (who might sleep from 8 p.m. to 4 a.m.). But unlike treatable circadian rhythm disorders, these patterns are inherited and lifelong. For anyone with these atypical sleep traits, obligations as simple as helping kids with after-dinner homework or showing up for morning classes or meetings can be serious problems. (Story continues below)
Sleep Hygiene
Common tips you can count on – and myths to watch out for
Healthy sleep habits are pretty straightforward: Keep a consistent wake-up time. Exercise. Avoid caffeine, alcohol, and big meals right before bed. Cultivate a cool, dark bedroom and banish devices. Make time to wind down before bed.
It’s easy to find these and other good habits online, but UCSF’s sleep experts warn that you may also find some common tips that you should take with a grain of salt:
Don’t: Force yourself into a consistent bedtime
A regular bedtime is great if you’re sleeping well. But if you can’t fall asleep, trying to force it will only make things worse. Instead, get up and do something relaxing until you’re sleepy. Lying awake perpetuates insomnia by stoking your anxiety and weakening your mind’s association that bed means sleep.
Don’t: Obsess over sleep data from your smart devices
Aric Prather says today’s sleep trackers can’t accurately estimate sleep stages, but the analyses they generate may cause sleep anxiety. There’s actually a term for this: orthosomnia. Most people are better off just listening to their bodies and waking at a consistent time. “You know when you wake up and don’t feel refreshed,” says Prather. “You don’t need a device to tell you that.”
Don’t: Focus too much on blue light
Worried about the effect of your smartphone’s blue light on your sleep? Some evidence suggests that blue light exposure can impair sleep, but Prather says the hype may be stronger than the science. Likely more harmful to slumber are some kinds of content. Reading a relaxing book on your phone is probably fine. But the stimulation of emailing, texting, tweeting, or doom-scrolling the news could trigger insomnia. Even so, it wouldn’t hurt to turn on your phone’s blue-light filter.
Don’t: Misunderstand melatonin
Melatonin is one of the most commonly used supplements, and one of the most misunderstood. Melatonin does not make you sleepy. Your brain produces melatonin in response to darkness as part of your body’s internal clock. So melatonin supplements can help reset your circadian clock after a trans-Atlantic flight or some other disruption. But they are not the key to calming your racing thoughts.
Finding the missing puzzle pieces
No one has done more to understand the relationship between our genes and the mechanisms of sleep than Fu and Ptáček.
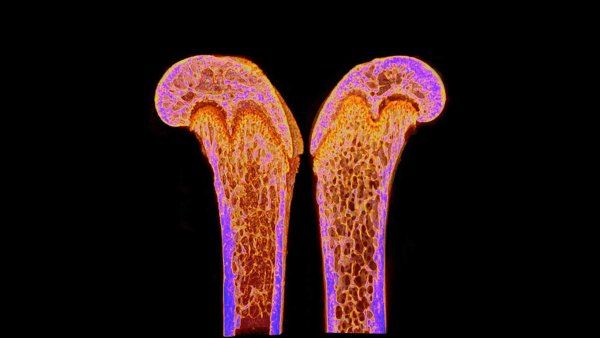
In 2009, Fu identified the first gene known to be responsible for “familial natural short sleep,” as Joanne Osmond’s extreme sleep efficiency is officially known. Fu discovered a tiny mutation in a gene called DEC2 and found that individuals with the mutation sleep significantly less than people without it. (To conclusively prove the matter, her team genetically engineered mice to express this same mutation; as predicted, the rodents slept less without decreasing their performance on physical or cognitive tests.)
Since that initial discovery, Fu and Ptáček have worked together tirelessly to find additional short-sleep genes, sequencing whole exomes of more than 30 families with this inherited trait, including Osmond’s family. The massive effort paid off in 2019 when they discovered mutations in three more genes that also lead to short, hyper-efficient sleep. They expect to publish several more such discoveries in the near future, and Ptáček speculates that, all told, there may be 10, 20, or more as-yet-undiscovered genes associated with familial natural short sleep.
As they find these additional pieces of the genetic puzzle, they are working with Krystal and another colleague, Liza Ashbrook, MD ’11, to decode how the underlying blueprints of sleep regulation work, why sleep benefits human wellness so dramatically, and what specific molecules and processes should be the targets of next-generation sleep medications and therapies. They believe that understanding these genes could provide all of us with more restorative sleep.
“When I hear the National Academy of Medicine talking about healthy aging,” says Fu, “they are talking about drugs and equipment to help old people. For me, I want to help everybody sleep efficiently to achieve long, healthy lives. That would be such a much bigger impact for humanity.”
For Osmond, however, the value of learning that her unusual sleep pattern is a genetic trait has been far more personal. For all the advantages the trait may confer, she has spent a lifetime being told that her minimal sleep pattern is unhealthy; a sister who shares the trait was even prescribed sleeping pills to “normalize” her nights. “I think it’s a very lonely type of life,” Osmond reflects. “When I finally learned that I’m this way because of my genes, I was like, ‘Oh, I’m not broken. I am OK.’”